|
Note: Large images and
tables on this page may necessitate printing in landscape mode.
Copyright
©2006 The McGraw-Hill Companies. All rights reserved.
Emergency
Medicine Atlas > Part 1. Regional
Anatomy > Chapter 1. Head and Facial Trauma >
|
Basilar Skull Fracture
Associated Clinical Features
The skull base comprises the
floors of the anterior, middle, and posterior cranial fossae. Trauma resulting
in fractures to this basilar area typically does not have localizing
symptoms. Plain skull radiographs are poor in identifying these
fractures. Indirect signs of the injury may include visible evidence of
bleeding from the fracture into surrounding soft tissue, such as a
Battle's sign (Figs. 1.1, 1.2) or "raccoon eyes" (Fig. 1.3).
Bleeding into other structures—including hemotympanum (Fig. 1.4) or
blood in the sphenoid sinus seen as an air-fluid level—may also be
seen. Cerebrospinal fluid (CSF) leaks may also be evident and noted as
clear or pink rhinorrhea. If CSF is present, a dextrose stick test may be
positive. The fluid can be placed on filter paper and a "halo"
or double ring may be seen (Fig. 1.5).
|
|
|

|
|
Battle's
Sign Ecchymosis in the
postauricular area develops when the fracture line communicates with
the mastoid air cells, resulting in blood accumulating in the
cutaneous tissue. This patient had sustained injuries several days
prior to presentation. (Courtesy of Frank Birinyi, MD.)
|
|
|
|
|

|
|
Battle's
Sign A subtle Battle's sign is
seen in this patient with head trauma. This sign may take hours to
develop fully. (Courtesy of Lawrence B. Stack, MD.)
|
|
|
|
|

|
|
Raccoon
Eyes Ecchymosis in the
periorbital area, resulting from bleeding from a fracture site in the
anterior portion of the skull base. May also be caused by facial
fractures. (Courtesy of Frank Birinyi, MD.)
|
|
|
|
|
|
|
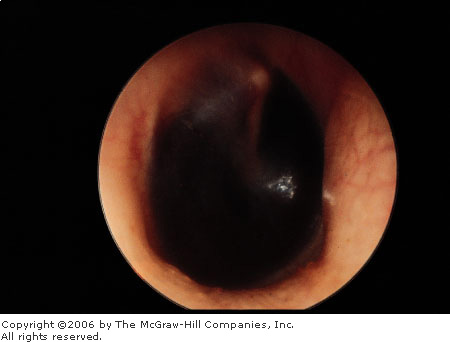
Hemotympanum Seen in a basilar skull fracture when the
fracture line communicates with the auditory canal, resulting in
bleeding into the middle ear. Blood can be seen behind the tympanic
membrane. (Courtesy of Richard A. Chole, MD, PhD.)
|
|
|
|
|

|
|
Cerebrospinal
Fluid Leak This example, from
the nose, can be difficult to distinguish from blood or mucus. The
distinctive double-ring sign, seen here, comprises blood (inner
ring) and CSF (outer ring). The reliability of this test
has been questioned. (Courtesy of David W. Munter, MD.)
|
|
Differential Diagnosis
Direct trauma without skull
fracture can result in external ecchymosis. Barotrauma can cause
hemotympanum. Facial injuries and fractures can cause facial ecchymosis.
Emergency Department Treatment
and Disposition
The mainstay of therapy is to
identify underlying brain injury, which is best accomplished by computed
tomography (CT). CT is also the best diagnostic tool for identifying the
fracture site, but fractures may not always be evident. Evidence of open
communication, such as a CSF leak, mandates neurosurgical consultation
and admission. Otherwise, the decision for admission is based on the
patient's clinical condition, other associated injuries, and evidence of
underlying brain injury as seen on CT. The use of antibiotics in the
presence of a CSF leak is controversial because of the possibility of
selecting resistant organisms.
Clinical Pearls
1. The clinical manifestations
of basilar skull fracture may take several hours to fully develop.
2. Since plain films are
unhelpful, there should be a low threshold for head CT in any patient
with head trauma, loss of consciousness, obtundation, severe headache,
visual changes, or nausea or vomiting.
3. The use of filter paper or a
dextrose stick test to determine if CSF is present in rhinorrhea is not
100% reliable.
|
|
Depressed Skull Fracture
Associated Clinical Features
Depressed skull fractures
typically occur when a large force is applied over a small area. They are
classified as open if the skin above them is lacerated (Fig. 1.6) and
closed if the overlying skin is intact. Abrasions, contusions, and
hematomas may also be present over the fracture site. The patient's
mental status can range from comatose to fully alert depending on the
extent of the associated brain injury. Soft tissue bleeding and swelling
may be present. Evidence of other injuries such as a basilar fracture or
facial fractures may also be present.
|
|
|

|
|
Depressed
Skull Fracture A scalp
laceration overlying a depressed skull fracture. Wearing a sterile
glove, the examiner should digitally explore all scalp lacerations
for evidence of fracture or depression. (Courtesy of David W. Munter,
MD.)
|
|
Differential Diagnosis
Direct trauma can cause
abrasions, contusions, hematomas, and lacerations without an underlying
depressed skull fracture. Every laceration to the scalp should be
explored and palpated to rule out depression of a fracture. Alterations
in mental status may occur with or without fracture. Penetrating injuries
to the skull and brain can produce a similar clinical picture.
Emergency Department Treatment
and Disposition
Plain films have been suggested
for suspected depressed skull fractures and if positive should be
followed by CT, which will more accurately demonstrate the degree of
depression as well as any underlying brain injury (Fig. 1.7). Others
suggest that plain films offer little diagnostic utility and recommend CT
with its more accurate bone windows for any suspected depressed skull
fracture. When depressed skull fractures are noted on plain films or CT,
immediate neurosurgical consultation is required. Open fractures also
require antibiotics and tetanus prophylaxis as indicated. The decision to
observe or operate immediately is made by the neurosurgeon. Children
below 2 years of age with skull fractures can develop leptomeningeal
cysts. These cysts, which are extrusion of CSF or brain through dural
defects, are associated with skull fractures. For this reason, children
below age 2 with skull fractures require follow-up or admission.
|
|
|
|
|
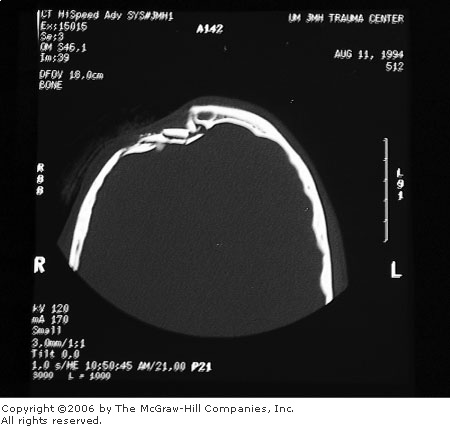
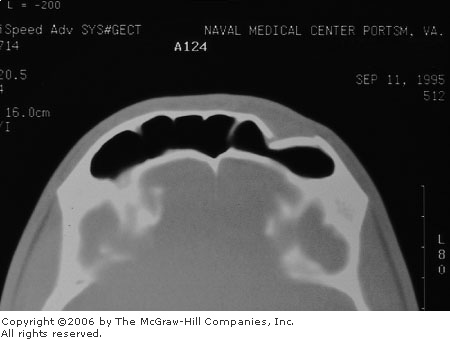
Depressed
Skull Fracture CT
demonstrating depressed skull fracture. (Courtesy of David W. Munter,
MD.)
|
|
Clinical Pearls
1. Gently palpate all scalp
injuries including lacerations for evidence of fractures or depression.
When fragments are depressed more than 3 to 5 mm below the inner table,
penetration of the dura and injury to the cortex are more likely.
2. Children with depressed
skull fractures are more likely to develop epilepsy.
3. The index of suspicion for
nonaccidental trauma should be raised for children below 2 years of age
with depressed skull fractures.
|
|
Nasal Injuries
Associated Clinical Features
Clinically significant nasal
fractures are almost always evident on examination, with deformity,
swelling, and ecchymosis present (Fig. 1.8). Injuries may occur to other
surrounding bony structures, including fractures of the orbit, frontal
sinus, or cribriform plate. A history of a mechanism with significant force,
loss of consciousness, or findings of facial bone injury or CSF leak
should alert the clinician to look for these associated injuries.
Epistaxis may be due to a septal or turbinate laceration but can also be
seen with fractures of surrounding bones, including the cribriform plate.
Septal hematoma (Fig. 1.9) is a rare but important complication that, if
untreated, may result in necrosis of the septal cartilage and a resultant
"saddle-nose" deformity.
|
|
|

|
|
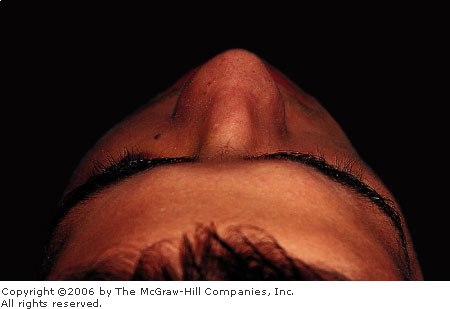
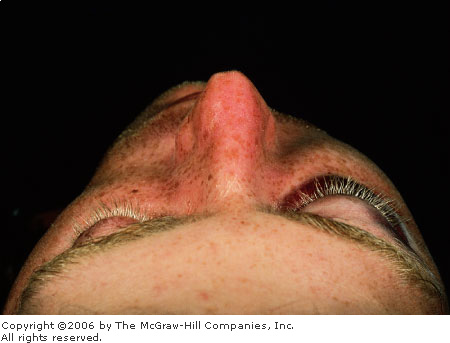
Nasal
Fracture Deformity is evident
on examination. Note periocular ecchymosis indicating the possibility
of other facial fractures (or injuries). The decision to obtain
radiographs is based on clinical findings. A radiograph is not
indicated for an isolated simple nasal fracture. (Courtesy of David
W. Munter, MD.)
|
|
|
|
|

|
|
Septal
Hematoma A bluish, grapelike
mass on the nasal septum. If untreated, this can result in septal
necrosis and a saddle-nose deformity. An incision, drainage, and
packing are indicated. (Courtesy of Lawrence B. Stack, MD.)
|
|
Differential Diagnosis
Nasal fractures may have
associated facial injuries—such as orbital, frontal sinus, or
cribriform plate fractures—and these more serious injuries must be
ruled out. A simple nasal contusion may present identically to a simple
nasal fracture with pain, swelling, and ecchymosis. A frontonasoethmoid
fracture has nasal or frontal crepitus and may have associated
telecanthus or obstruction of the nasolacrimal duct.
Emergency Department Treatment
and Disposition
Look for more serious injuries
first. Patients with associated facial bone deformity or tenderness may
require radiographs to rule out facial fractures. Nasal fractures rarely
require radiographs (Fig. 1.10). Obvious deformities are referred within
2 to 5 days for reduction, after the swelling has subsided. Nasal
injuries without deformity need only conservative therapy with an
analgesic and possibly a nasal decongestant. Septal hematomas must be
immediately drained, with packing placed to prevent reaccumulation. In
some cases, epistaxis may not be controlled by pressure alone and may
require nasal packing. Lacerations overlying a simple nasal fracture
should be vigorously irrigated and primarily closed with the patient
placed on antibiotic coverage. Complex nasal lacerations with underlying
fractures should be referred for closure. Nasal fractures with mild
angulation and without displacement may be reduced in the ED by
manipulating the nose with the examiner's thumbs into the correct
alignment.
|
|
|

|
|
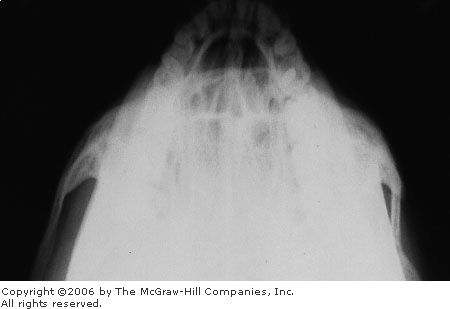
Nondisplaced
Nasal Fracture Radiograph of a
fracture of the nasal spine, for which no treatment other than ice
and analgesics is needed. This radiograph did not change the
treatment or disposition of the patient. (Courtesy of Lorenz F.
Lassen, MD.)
|
|
Clinical Pearls
1. Rule out any life threats or
serious associated injuries.
2. Control epistaxis to perform
a good intranasal examination. If there is no epistaxis or deformity,
treat the patient with ice and analgesics. If obvious deformity is
present, including a new septal deviation or deformity, treat with ice
and analgesics and provide ear/nose/throat (ENT) referral in 2 to 5 days for
reduction.
3. Although the effectiveness
of prophylactic antibiotics to prevent toxic shock syndrome is unproved,
every patient discharged with nasal packing should be placed on
antistaphylococcal antibiotics and referred to ENT in 2 to 3 days.
4. Consider cribriform plate
fractures in patients with clear rhinorrhea after nasal injury, with the
understanding that this finding may be delayed.
5. Check every patient for a
septal hematoma.
|
|
Fractures of the Zygoma
Associated Clinical Features
The zygoma bone has two major
components, the zygomatic arch and the body. The arch forms the inferior
and lateral orbit, and the body forms the malar eminence of the face.
Fractures to the zygoma are usually the result of blunt trauma. Direct
blows to the arch can result in isolated arch fractures (Fig. 1.11).
These present clinically with pain on opening the mouth secondary to the
insertion of the temporalis muscle at the arch or impingement on the
coronoid process. More extensive trauma can result in the "tripod fracture,"
which consists of fractures through three structures: the frontozygomatic
suture; the maxillary process of the zygoma including the inferior
orbital floor, inferior orbital rim, and lateral wall of the maxillary
sinus; and the zygomatic arch (Figs. 1.12, 1.13). Clinically, patients
present with a flattened malar eminence and edema and ecchymosis to the
area, with a palpable step-off on examination. Injury to the infraorbital
nerve may result in infraorbital paresthesia, and gaze disturbances may result
from injury to orbital contents. Subcutaneous emphysema may be caused by
a fracture of the antral wall at the zygomatic buttress.
|
|
|
|
|
Zygomatic
Arch Fracture Jug-handle view
of the zygomatic arch demonstrating a depressed fracture. In such a
case, operative reduction can be delayed for several days. (Courtesy
of Timothy D. McGuirk, DO.)
|
|
|
|
|
|
|
Zygomatic
Fracture Patient with blunt
trauma to the zygoma. Flattening of the right malar eminence is
evident. (Courtesy of Edward S. Amrhein, DDS.)
|
|
|
|
|
|
|
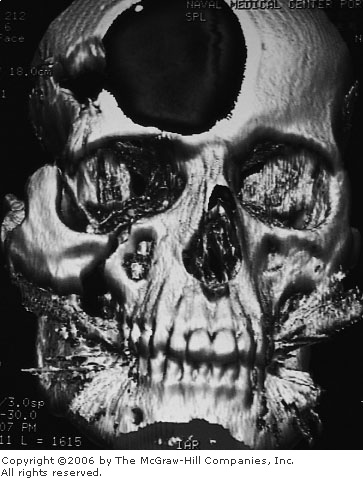
Tripod
Fracture The fracture lines
involved in a tripod fracture are demonstrated in this
three-dimensional CT reconstruction. The large defect in the frontal
area is artifact from the reconstruction. (Courtesy of Patrick W.
Lappert, MD.)
|
|
Differential Diagnosis
Other facial fractures, including
LeFort II and III fractures, may involve the zygoma bone or orbit. These
fractures typically involve more extensive facial trauma. Orbital blowout
fractures may present with entrapment and ocular injuries, but the malar
eminence appears normal.
Emergency Department Treatment
and Disposition
Plain films, including a Waters
view and "jug-handle" view (a submental-vertex view of the
zygomatic arches), demonstrate the fracture and evaluate the
zygomaticomaxillary complex. In the case of a tripod fracture, facial CT
will best show the involvement and degree of displacement. Since plain
films often do not adequately demonstrate all elements of the fracture,
patients with evidence of a tripod fracture should have CT on an urgent
basis to help identify the extent of bony injuries. The CT results guide
the need for urgent referral. Simple zygomatic arch or tripod fractures
without eye injury can be treated with ice and analgesics and referred
for delayed operative consideration in 5 to 7 days. More extensive tripod
fractures or those with eye injuries should be referred more urgently.
Decongestants and broad-spectrum antibiotics are generally recommended
for tripod fractures, since the fracture crosses into the maxillary
sinus.
Clinical Pearls
1. Tripod fractures are often
associated with orbital and ocular trauma. Palpate the zygomatic arch and
orbital rims carefully for a step-off deformity.
2. Examine for eye findings
such as diplopia, hyphema, or retinal detachment. Check for infraorbital
paresthesia indicating injury or impingement of the second division of
cranial nerve V.
3. Visual inspection of the
malar eminence from several angles (especially by viewing the area from
over the head of the patient in the coronal plane, Fig. 1.12) allows
detection of a subtle abnormality.
4. Insist on adequate
radiographs of the zygomatic arches, which require good positioning of
the patient.
|
|
LeFort Facial Fractures
Associated Clinical Features
All LeFort facial fractures
involve the maxilla (Fig. 1.14). Clinically, the patient has facial
injuries, swelling, and ecchymosis (Figs. 1.15, 1.16). LeFort I fractures
are those involving an area under the nasal fossa. LeFort II fractures
involve a pyramidal area including the maxilla, nasal bones, and medial
orbits. LeFort III fractures, sometimes described as craniofacial dissociation,
involve the maxilla, zygoma, nasal and ethmoid bones, and the bones of
the base of the skull. Airway compromise may be associated with LeFort II
and III fractures. Physical examination is sometimes helpful in
distinguishing the three. The examiner places fingers on the bridge of
the nose and tries to move the central maxillary incisors with the other
hand. If only the maxilla moves, a LeFort I is present; movement of the
upper jaw and nose indicates a LeFort II; and movement of the entire
midface and zygoma indicates a LeFort III. Because of the extent of
LeFort II and III fractures, they may be associated with cribriform plate
fractures and CSF rhinorrhea. The force required to sustain a LeFort II
or III fracture is considerable, and associated brain or cervical spine
injuries are common.
|
|
|
|
|
LeFort
Fractures Illustration of the
fracture lines of LeFort I (alveolar), LeFort II (zygomatic maxillary
complex), and LeFort III (cranial facial dysostosis) fractures.
|
|
|
|
|

|
|
LeFort
Facial Fractures Clinical
photograph of patient with blunt facial trauma. Note the ecchymosis
and edema. This patient sustained a LeFort II/III fracture (a LeFort
II fracture on one side and a LeFort III on the other), and
associated intracranial hemorrhages. (Courtesy of Stephen Corbett,
MD.)
|
|
|
|
|

|
|
LeFort
Facial Fractures Clinical
photograph of patient with blunt facial trauma. Patient demonstrates
the classic "dish face" deformity (depressed midface)
associated with bilateral LeFort III fractures. (Courtesy of Robert
Schnarrs, MD.)
|
|
Differential Diagnosis
LeFort II and III fractures can
be difficult to distinguish, and combination LeFort fractures (e.g.,
LeFort II on one side and LeFort III on the other) are common. Tripod and
frontonasoethmoid fractures may be present in blunt facial trauma as
well.
Emergency Department Treatment
and Disposition
Patients with associated facial
bone deformity or tenderness may require radiographs to rule out facial
fractures. Plain facial films will reveal the presence of facial
fractures but are less helpful in determining the type or extent. Head
and facial CT, including three-dimensional re-creations, offer much more
useful information. Management of LeFort I fractures may involve only
dental splinting and oral surgery referral, but management of LeFort II
and III fractures normally requires admission because of associated injuries
as well as definitive operative repair. Epistaxis may be difficult to
control in LeFort II and III fractures, in rare cases requiring
intraoperative arterial ligation.
Clinical Pearls
1. Attention should be focused
on immediate airway management, since the massive edema associated with
LeFort II and III fractures may quickly lead to airway compromise.
2. Nasotracheal intubation
should be avoided because of the possibility of intracranial passage.
3. Any serious facial trauma
may also be associated with cervical spine injuries.
4. Associated cranial injuries
are common and are best evaluated by CT.
5. If not recognized, an occult
CSF leak may result in significant morbidity. Suspected CSF leaks require
neurosurgical consultation.
6. The best diagnostic modality
for delineation of the extent of injuries is CT of the facial bones.
|
|
Orbital Blowout Fracture
Associated Clinical Features
Blowout fractures occur when the
globe sustains a direct blunt force. There are two mechanisms of injury.
The first is a true blowout fracture, where all energy is transmitted to
the globe. The spherical globe is stronger than the thin orbital floor,
and the force is transmitted to the thin orbital floor or medially
through the ethmoid bones, with the resultant fracture. The object
causing the injury must be smaller than 5 to 6 cm, otherwise the globe is
protected by the surrounding orbit. Fists or small balls are the typical
causative agents. This mechanism of injury is more likely to cause
entrapment and globe injury. The second mechanism of injury occurs when
the energy from the blow is transmitted to the infraorbital rim, causing
a buckling of the orbital floor. Entrapment and globe injury is less
likely with this mechanism of injury. Patients with blowout fractures have
periorbital ecchymosis and lid edema (Figs. 1.17, 1.18) but may sustain
eye injuries as well, including chemosis, subconjunctival hemorrhage, or
infraorbital numbness from injury to the infraorbital nerve. Other eye
injuries should be sought and ruled out with a careful physical
examination; they include corneal abrasion, hyphema, enophthalmos,
proptosis, iridoplegia, dislocated lens, retinal tear, retinal
detachment, and ruptured globe. If the inferior rectus muscle is extruded
into the fracture, it may become entrapped; upward gaze is then limited,
with resultant diplopia (Figs. 1.19, 1.20). Because of the communication
with the maxillary sinus, subcutaneous emphysema is common.
|
|
|

|
|
Orbital
Ecchymosis Sustained from
blunt trauma to the globe, with some of the force directed to the
inferior orbital rim. This patient presents with subtle signs only
(ecchymosis and swelling with no entrapment or eye injury) yet has
the classic signs on plain films (Figure 1.18). This patient
demonstrates that orbital floor fractures can present with subtle
physical findings. (Courtesy of Kevin J. Knoop, MD, MS.)
|
|
|
|
|
|
|
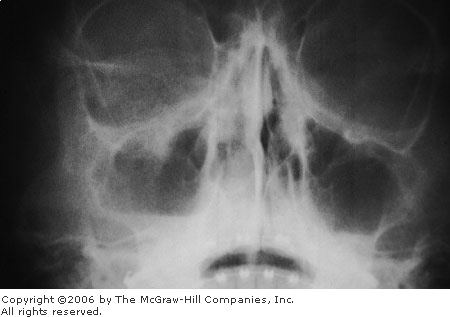
Blowout
Fracture Plain film
demonstrating a fracture of the floor of the right orbit, with a
teardrop sign due to extruded orbital contents. There is an
associated air-fluid level in the maxillary sinus due to blood. Note
the two lines seen at the inferior orbit: the infraorbital rim and
inferior floor of the orbit. These are well visualized on the
unaffected side but disrupted on the affected side. (Courtesy of
Kevin J. Knoop, MD, MS.)
|
|
|
|
|

|
|
Inferior
Rectus Entrapment The inferior
rectus muscle is entrapped within the blowout fracture. When the
patient tries to look upward, the affected eye has limited upward
gaze. The patient experiences diplopia with this maneuver. (Courtesy
of Lawrence B. Stack, MD.)
|
|
|
|
|

|
|
Blowout
Fracture with Entrapment CT of
the patient in Fig. 1.19 demonstrating the entrapped muscle extruding
into the maxillary sinus. (Courtesy of Lawrence B. Stack, MD.)
|
|
Differential Diagnosis
Orbital contusions present with
similar physical findings. Fractures of the orbital rim are clinically
similar to orbital blowout fractures. Other facial fractures (zygoma,
tripod, LeFort) may involve the orbital floor but are associated with
more extensive injuries to the face outside of the orbit.
Emergency Department Treatment
and Disposition
Plain radiography to include a
Caldwell view (showing orbital rim and walls) and a Waters view (orbital
floor and roof) demonstrates the fracture. Patients without eye injury or
entrapment may be treated conservatively with ice and analgesics and
referred for follow-up in 2 to 3 days. Patients with blood in the
maxillary sinus are usually treated with antibiotics. Strongly consider
an ophthalmology consultation in patients with a true blowout fracture
(all energy transmitted to the globe), since up to 30% of these patients
sustain a globe injury. Patients with entrapment should receive a CT of
the orbits and be referred on a same-day basis. Most specialists will
observe fractures with entrapment for 10 to 14 days to allow for
resolution of edema prior to operative repair.
Clinical Pearls
1. Enophthalmos, limited upward
gaze, diplopia with upward gaze, or infraorbital anesthesia from
entrapment or injury to the infraorbital nerve should heighten suspicion
of a blowout fracture.
2. Compare the pupillary level
on the affected side with the unaffected side, since it may be lower from
prolapse of the orbital contents into the maxillary sinus. Subtle
abnormalities may be appreciated as an asymmetric corneal light reflex
(Hirschberg's reflex).
3. Subcutaneous emphysema on
clinical examination, a soft-tissue teardrop along the roof of the
maxillary sinus on plain film, or an air-fluid level in the maxillary
sinus on plain film should also be interpreted as evidence of a blowout
fracture.
4. Some patients present with
unusual complaints—for example, of an eye swelling up after the
patient blows his or her nose (from subcutaneous emphysema) or air
bubbles emanating from the tear duct.
5. Carefully examine the eye
for visual acuity, hyphema, or retinal detachment. Remember to assess the
nose for a septal hematoma.
|
|
Mandibular Fractures
Associated Clinical Features
A history of blunt trauma,
mandibular pain, and possible malocclusion is normally seen with
mandibular fractures. A step-off in the dental line (Fig. 1.21) or
ecchymosis or hematoma to the floor of the mouth are often present.
Mandibular fractures may be open to the oral cavity, as manifest by gum
lacerations. Dental trauma may be associated. Other clinical features
include inferior alveolar or mental nerve paresthesia, loose or missing
teeth, dysphagia, trismus, or ecchymosis of the floor of the mouth
(considered pathognomonic) (Figs. 1.22, 1.23). Multiple mandibular
fractures are present in more than 50% of cases because of the ring-like
structure of the mandible. Mandibular fractures are often classified as
favorable or unfavorable, depending on the location and resultant
displacement forces exerted by the associated musculature. Those
fractures displaced by the masseter muscle are unfavorable (Fig. 1.24)
and inevitably require fixation, whereas fractures that are not displaced
by traction are favorable and in some cases will not require fixation.
Injuries creating unstable mandibular fractures may create airway
obstruction because the support for the tongue is lost. Mandibular
fractures are also classified based on the anatomic location of the
fracture (Fig. 1.25).
|
|
|

|
|
Open
Mandibular Fracture The open
fracture line is evident clinically. There is slight misalignment of
the teeth. (Courtesy of Edward S. Amrhein, DDS.)
|
|
|
|
|

|
|
Sublingual
Hemorrhage Hemorrhage or
ecchymosis in the sublingual area is pathognomonic for mandibular
fracture. (Courtesy of Lawrence B. Stack, MD.)
|
|
|
|
|

|
|
Bilateral
Mandibular Fracture The
diagnosis is suggested by the bilateral ecchymosis seen in this
patient. (Courtesy of Lawrence B. Stack, MD.)
|
|
|
|
|

|
|
Unfavorable
Mandibular Fracture Dental
panoramic view demonstrating a mandibular fracture with obvious
misalignment due to the distracting forces of the masseter muscle.
(Courtesy of Edward S. Amrhein, DDS.)
|
|
|
|
|
|
|
Classification
of Mandibular Fractures
Classification based on anatomic location of the fracture.
|
|
Differential Diagnosis
Contusions have a similar
presentation and can be differentiated only radiographically. Dislocation
of the mandibular condyles may also result from blunt trauma and will
always have associated malocclusion, typified by an inability to close
the mouth. Isolated dental trauma may have a similar presentation, and
underlying mandibular fracture should be ruled out.
Emergency Department Disposition
and Treatment
The best view for evaluating
mandibular trauma is a dental panoramic view, which should be obtained if
available. Plain films should include anteroposterior (AP), bilateral
oblique, and Townes views to evaluate the condyles. Nondisplaced
fractures can be treated with analgesics, soft diet, and referral to oral
surgery in 1 to 2 days. Displaced fractures, open fractures, and
fractures with associated dental trauma need more urgent referral. All
mandibular fractures should be treated with antibiotics effective against
anaerobic oral flora (clindamycin, amoxicillin clavulanate) and tetanus
prophylaxis given if needed. The Barton's bandage has been suggested to
immobilize the jaw in the ED.
Clinical Pearls
1. The presence of disfiguring
facial injuries can be distracting. The primary consideration in the
evaluation of the patient with facial fractures is the assessment and treatment
of life-threatening injuries.
2. Any patient with trauma and
malocclusion should be considered to have a mandibular fracture.
3. The most sensitive sign of a
mandibular fracture is malocclusion. The jaw will deviate toward the side
of a unilateral condylar fracture on maximal opening of the mouth. A
nonfractured mandible should be able to hold a tongue blade between the
molars tightly enough to break it off. There should be no pain in
attempting to rotate the tongue blade between the molars.
4. Bilateral parasymphyseal
fractures may cause acute airway obstruction in the supine patient. This
is relieved by pulling the subluxed mandible and soft tissue forward and,
in patients in whom the cervical spine has been cleared, by elevating the
patient to a sitting position.
|
|
External Ear Injuries
Associated Clinical Features
Injuries to the external ear may
be open or closed. Blunt external ear trauma may cause a hematoma
(otohematoma) of the pinna (Fig. 1.26), which, if untreated, may result
in cartilage necrosis and chronic scarring or further cartilage formation
and permanent deformity ("cauliflower ear") (Fig. 1.27). Open
injuries include lacerations (with and without cartilage exposure) and
avulsions (Fig. 1.28).
|
|
|

|
|
Pinna
Hematoma A hematoma has
developed, characterized by swelling, discoloration, ecchymosis, and
flocculence. Immediate incision and drainage or aspiration is
indicated, followed by an ear compression dressing. (Courtesy of C.
Bruce MacDonald, MD.)
|
|
|
|
|

|
|
Cauliflower
Ear Repeated trauma to the
pinna or undrained hematomas can result in cartilage necrosis and
subsequent deforming scar formation. (Courtesy of Timothy D. McGuirk,
DO.)
|
|
|
|
|

|
|
Avulsed
Ear This ear injury, sustained
in a fight, resulted when the pinna was bitten off. Plastic repair is
needed. The avulsed part was wrapped in sterile gauze soaked with
saline and placed in a sterile container on ice. (Courtesy of David
W. Munter, MD.)
|
|
Differential Diagnosis
These injuries are normally
self-evident. Pinna hematomas and contusions can sometimes be difficult
to distinguish, but flocculence is the hallmark of the hematoma.
Emergency Department Treatment
and Disposition
Pinna hematomas must undergo
incision and drainage or large needle aspiration using sterile technique,
followed by a pressure dressing to prevent reaccumulation of the
hematoma. This procedure may need to be repeated several times; hence,
after ED drainage, the patient is treated with antistaphylococcal
antibiotics and referred to ENT or plastic surgery for follow-up in 24 h.
Lacerations must be carefully examined for cartilage involvement; if this
is present, copious irrigation, closure, and postrepair oral antibiotics
covering skin flora are indicated. Simple skin lacerations may be
repaired primarily with nonabsorbable 6-0 sutures. The dressing after
laceration repair is just as important as the primary repair. If a
compression dressing is not placed, hematoma formation can occur. Complex
lacerations or avulsions normally require ENT or plastic surgery
referral.
Clinical Pearls
1. Pinna hematomas may take
hours to develop, so give patients with blunt ear trauma careful
discharge instructions, with a follow-up in 12 to 24 h to check for
hematoma development.
2. Failure to adequately drain
a hematoma, reaccumulation of the hematoma owing to a faulty pressure
dressing, or inadequate follow-up increases the risk of infection of the
pinna (perichondritis) or of a disfiguring cauliflower ear.
3. Copiously irrigate injuries
with lacerated cartilage, which can usually be managed by primary closure
of the overlying skin. Direct closure of the cartilage is rarely
necessary and is indicated only for proper alignment, which helps lessen
later distortion. Use a minimal number of absorbable 5-0 or 6-0 sutures
through the perichondrium.
4. Lacerations to the lateral
aspect of the pinna should be minimally debrided because of the lack of
tissue at this site to cover the exposed cartilage.
5. In the case of an avulsion
injury, the avulsed part should be cleansed, wrapped in saline-moistened
gauze, placed in a sterile container, then placed on ice to await
reimplantation by ENT.
|
|
Frontal Sinus Fracture
Associated Clinical Features
Blunt trauma to the frontal area
may result in a depressed frontal sinus fracture. Often, there is an
associated laceration (Fig. 1.29). Isolated frontal fractures (Figs.
1.30, 1.31) normally do not have the associated features of massive blunt
facial trauma such as seen in LeFort II and III fractures. Careful nasal
speculum examination may reveal blood or CSF leak high in the nasal
cavity. Posterior table involvement can lead to mucopyocoele or epidural
empyema as late sequelae. Involvement of the posterior wall of the
frontal sinus may occur and result in cranial injury or dural tear.
|
|
|

|
|
Frontal
Laceration Any laceration over
the frontal sinuses should be explored to rule out a fracture. This
laceration was found to have an associated frontal fracture.
(Courtesy of David W. Munter, MD.)
|
|
|
|
|

|
|
Frontal
Sinus Fracture Fracture defect
seen at the base of a laceration over the frontal sinus. (Courtesy of
Jeffrey Kuhn, MD.)
|
|
|
|
|

|
|
Frontal
Sinus Fracture Fracture of the
outer table of the frontal sinus is seen under this forehead
laceration. (Courtesy of Lawrence B. Stack, MD.)
|
|
Differential Diagnosis
Simple lacerations or contusions
of the frontal area may not involve fractures. Frontal fractures may be
part of a complex of facial fractures, as seen in frontonasoethmoid
fractures, but generally more extensive facial trauma is required.
Emergency Department Treatment
and Disposition
Frontal sinus fractures revealed
on plain films of the frontal bones, including posteroanterior (PA),
lateral, and Waters views, may be quite subtle. The extent of the frontal
injury, especially posterior table involvement, is best investigated with
bone windows on CT (Fig. 1.32). Fractures involving only the anterior
table of the frontal sinus can be treated conservatively with referral to
ENT or plastic surgery in 1 to 2 days. Fractures involving the posterior
table require urgent neurosurgical referral. Frontal sinus fractures are
usually covered with high-dose antibiotics against both skin and sinus
flora (second- or third-generation cephalosporins). ED management also
includes control of epistaxis, application of ice packs, and analgesia.
|
|
|
|
|
Frontal
Sinus Fracture CT of the
patient in Figure 1.29 demonstrating a fracture of the anterior table
of the frontal sinus. (Courtesy of David W. Munter, MD.)
|
|
Clinical Pearls
1. Explore every frontal
laceration digitally before repair. Digital palpation is sensitive for
identifying frontal fractures, although false positives from lacerations
extending through the periosteum can occur.
2. Communication of irrigating
solutions with the nose or mouth indicates a breach in the frontal sinus.
3. For serious injuries, a CT
scan is mandatory to assess the posterior aspect of the sinus and for
possible intracranial injury.
|
|
Traumatic Exophthalmos
Associated Clinical Features
Normally the result of blunt
orbital trauma, the exophthalmos develops as a retrobulbar hematoma pushes
the globe outward. Patients present with periorbital edema, ecchymosis
(Fig. 1.33), a marked decrease in visual acuity, and an afferent
pupillary defect in the involved eye. The exophthalmos, which may be
obscured by periorbital edema, can be better appreciated from a superior
view (Fig. 1.34). Visual acuity may be affected by the direct trauma to
the eye, compression of the retinal artery, or, more rarely, neuropraxia
of the optic nerve.
|
|
|

|
|
Traumatic
Exophthalmos Blunt trauma
resulting in periorbital edema and ecchymosis, which obscures the
exophthalmos in this patient. The exophthalmos is not obvious in the
AP view and can therefore be initially unappreciated. Figure 1.34
shows the same patient viewed in the coronal plane from over the
forehead. (Courtesy of Frank Birinyi, MD.)
|
|
|
|
|
|
|
Traumatic
Exophthalmos Superior view,
demonstrating the right-sided exophthalmos. (Courtesy of Frank
Birinyi, MD.)
|
|
Differential Diagnosis
Periorbital ecchymosis and edema
can result from blunt trauma without a retrobulbar hematoma. Traumatic
chemosis can present with exophthalmos. Visual impairment can result from
retinal detachment, hyphema, globe rupture, or any number of nontraumatic
conditions. Nontraumatic exophthalmos can be caused by cavernous sinus
thrombosis, a complication of frontal sinusitis, or endocrine
(thyrotoxicosis) disorders.
Emergency Department Treatment
and Disposition
CT is the best modality to
determine the presence and extent of a retrobulbar hematoma and
associated facial or orbital fractures (Fig. 1.35). Referral to ENT and
ophthalmology is indicated on an urgent basis. An emergent lateral
canthotomy decompresses the orbit and can be performed in the ED.
Emergency treatment can be sight-saving.
|
|
|

|
|
Retrobulbar
Hematoma CT of the patient in
Figs. 1.33 and 1.34 with right retrobulbar hematoma and traumatic
exophthalmos. (Courtesy of Frank Birinyi, MD.)
|
|
Clinical Pearls
1. The retrobulbar hematoma and
resultant exophthalmos may not develop for hours. Give careful discharge
instructions to any patient with periorbital trauma.
2. Perform a careful ophthalmic
examination including visual acuity, since associated conditions such as
hyphema or retinal detachment are common.
3. A subtle exophthalmos may be
detected by looking down over the head of the patient and viewing the eye
from the coronal plane.
4. Lateral canthotomy is
indicated for emergent treatment of patients with traumatic exophthalmos
who demonstrate profound ischemic signs and symptoms of an afferent
pupillary defect and decreased vision.
5. An afferent pupillary defect
in a patient with blunt trauma to the face or eye with normal visual
acuity may be pharmacologically induced.
|
|