|
Note: Large images and
tables on this page may necessitate printing in landscape mode.
Copyright
©2006 The McGraw-Hill Companies. All rights reserved.
Emergency
Medicine Atlas > Part 1. Regional
Anatomy > Chapter 10. Gynecologic and Obstetric
Conditions > Gynecologic Conditions >
|
Vaginitis
Associated Clinical Features
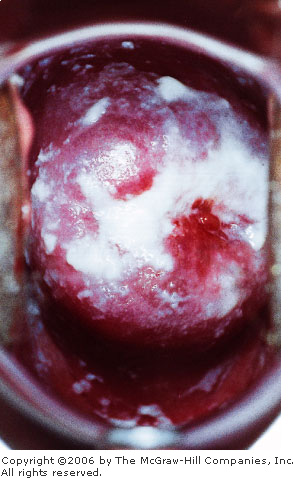
Candidal vaginitis is
characterized by a thick, curdy, white discharge (Fig. 10.1) and vulvar
discomfort. Intense vulvar erythema, pruritus, or burning are often
present. A microscopic slide prepared with 10% potassium hydroxide
yielding characteristic branch chain hyphae and spores establishes the
diagnosis (Fig. 21.16). The pH of the discharge is less than 4.5.
Predisposing factors that should be considered include oral
contraceptive, antibiotic, or corticosteroid use; pregnancy; and
diabetes. Sexually transmitted diseases are not usually associated with
isolated candidal vaginitis.
|
|
|
|
|
Candidal
Vaginitis Thick, curdy white
discharge secondary to candidal vaginitis. (Courtesy of Kevin J. Knoop,
MS, MD.)
|
|
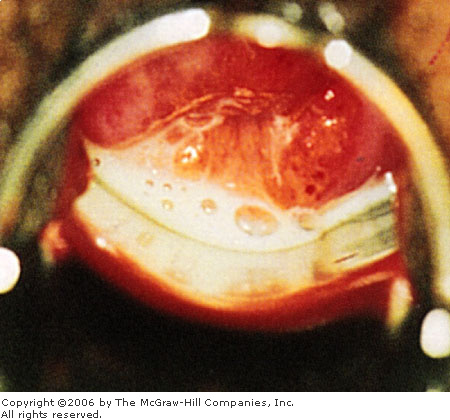
Trichomonas vaginitis presents as a
persistent, thin, copious discharge that is often frothy (Fig. 10.2),
green, or foul-smelling. The pH of these secretions is greater than 4.5.
The amount of vaginal and cervical erythema and inflammation varies
considerably; thus the diagnosis depends on the presence of motile
flagellates on normal saline wet-mount microscopy. Occasionally, multiple
petechiae on the vaginal wall (strawberry spots) or cervix (strawberry
cervix) are seen.
|
|
|
|
|
Trichomonas
Vaginitis Thin vaginal discharge suggestive of Trichomonas
vaginitis. (Courtesy of H. Hunter Handsfield: Atlas of Sexually
Transmitted Diseases. New York: McGraw-Hill; 1992.)
|
|
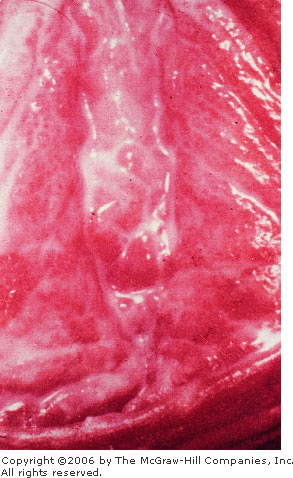
Bacterial vaginosis (previously termed Haemophilus
or Gardnerella vaginitis) is characterized by a malodorous,
homogeneous discharge (Fig. 10.3) with a pH greater than 4.5 and a
transient amine (fishy) odor when mixed with a drop of KOH solution
(positive sniff test). The presence of clue cells on normal saline wet
mount establishes the diagnosis (Fig. 21.13). Other associated vaginal or
abdominal complaints are minimal and, if significant, may represent
another disease process.
|
|
|
|
|
Gardnerella Vaginitis
Thin, milky white discharge suggestive of Gardnerella
vaginitis. (Courtesy of Curatek Pharmaceuticals.)
|
|
Differential Diagnosis
Vaginal foreign bodies,
especially in prepubescent girls, may present with a heavy white
discharge but would be unaccompanied by vulvar erythema or the
microscopic appearance of hyphae. Atrophic vaginitis is commonly found in
postmenopausal women and is distinguished from candidal vaginitis by
mucosal dryness, atrophy, dyspareunia, minimal discharge, and itching.
Other considerations include contact dermatitis, local irritation secondary
to tight-fitting underwear, and contact dermatitis from toiletry items.
Emergency Department Treatment
and Disposition
For candidal vaginitis,
various regimens of topical antifungal agents are the mainstay of
treatment (clotrimazole 1% cream, one applicatorful inserted high into
the vaginal vault for 7 nights, clotrimazole, two 100-mg vaginal tablets
for 3 nights or one 500-mg vaginal tablet for single-dose treatment).
Oral fluconazole (Diflucan, 150 mg as a single dose) is also effective.
Nystatin vaginal tablets (100,000 U daily for 2 weeks) are generally
considered safe for use in the first trimester of pregnancy.
For Trichomonas vaginitis,
a single, one-time dose of metronidazole (2 g) is generally curative.
Alternatively, 500 mg given twice daily can be used for recurrent or
refractory cases. Metronidazole is contraindicted in pregnancy and is
associated with an Antabuse-like reaction when taken with alcohol. For
the pregnant patient, clotrimazole (100-mg vaginal suppositories daily
for 7 to 14 days) may provide symptomatic relief.
For bacterial vaginosis, metronidazole
(500 mg twice daily for 7 days) is recommended in the nonpregnant
patient. Amoxicillin (500 mg tid for 7 days) or clindamycin (300 mg bid)
for 7 days is a safe but less effective alternative during pregnancy.
Treatment for asymptomatic infection or for male sexual partners is not
generally recommended.
Clinical Pearls
1. Diabetes mellitus or
immunosuppression should be considered in refractory or recurrent cases
of candidal vaginitis.
2. A history of balanitis in
the sexual partner should be sought and treated if present.
3. Trichomonas should be
considered a sexually transmitted disease. It is generally recommended,
therefore, that concomitant culturing for gonorrhea and Chlamydia
be performed. Serologic testing for syphilis, HIV, and hepatitis B should
be considered.
4. Patients treated with
metronidazole should abstain from alcohol for the duration of treatment
and for at least 24 h after their last dose.
|
|
Mucopurulent Cervicitis
Associated Clinical Features
The patient's chief complaint is
often a purulent vaginal discharge. Speculum examination reveals a
purulent, viscous discharge emanating from the cervical os (Fig. 10.4).
Otherwise, a purulent discharge may be seen on a cervical swab. A Gram's
stain may reveal either gram-negative intracellular diplococci consistent
with Neisseria gonorrhoeae (Fig. 21.11) or be nonspecific,
consistent with Chlamydia trachomatis, a coinfectant with the
gonococcus about 50% of the time. The diagnosis of pelvic inflammatory
disease should be considered, when accompanied by symptoms of lower
abdominal pain and signs of pelvic peritonitis such as cervical motion
and adnexal tenderness.
|
|
|

|
|
Mucopurulent
Cervicitis Viscous, opaque
discharge emanating from the cervical os, consistent with
mucopurulent cervicitis. The string from an intrauterine device is
seen descending through the os in this patient. (Courtesy of Sue
Rist, FNP.)
|
|
Differential Diagnosis
Physiologic cervical mucous
discharge at the time of ovulation may occur but is generally clear, with
few white blood cells on Gram's stain.
Emergency Department Treatment
and Disposition
Cultures for Chlamydia
trachomatis and N. gonorrhoeae should be obtained prior to
initiation of therapy. Ceftriaxone (125 mg as a single intramuscular
dose) provides coverage for N. gonorrhoeae. Single-dose oral
quinolones (ciprofloxacin, 500 mg, or ofloxacin, 400 mg) can be used in
penicillin-allergic patients. Doxycycline (100 mg) or ofloxacin (300 mg)
bid for 7 days or a single 1-g dose of azithromycin provides coverage for
Chlamydia. Erythromycin (base 500 mg qid for 7 days) is the
alternative for pregnant patients.
Clinical Pearls
1. The discharge of candidal,
trichomonal, or Gardnerella vaginitis is almost never limited
solely to the cervix.
2. Mucopurulent cervicitis is
almost always secondary to a sexually transmitted disease; thus sexual
partners should be treated as well.
3. Refer all patients for
formal gynecologic follow-up after culture and treatment, since early
cervical neoplasia may have a similar appearance.
|
|
Bartholin's Gland Abscess
Associated Clinical Features
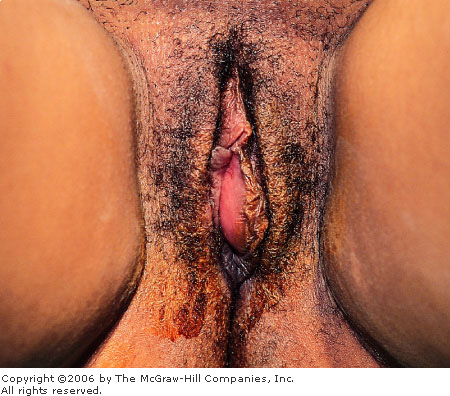
Bartholin's glands and ducts are
located over the lower third of the introitus near the labia minora. A
cyst or abscess can result from an obstructed duct, which usually occurs
secondary to scarring from trauma, delivery, or episiotomy. Infection of
the cyst is usually with mixed vaginal or fecal flora (Escherichia
coli) but may also contain Neisseria gonorrhoeae and Chlamydia
trachomatis. Progressive enlargement and infection lead to increasing
pain, swelling, and dyspareunia. A tender, fluctuant cystic mass with
surrounding labial edema is easily appreciated on examination (Fig.
10.5).
|
|
|
|
|
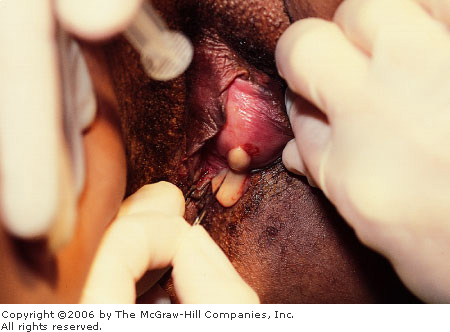
Bartholin's
Gland Abscess Typical
appearance of a Bartholin's gland abscess with the labial fluctuance
pointing medially. (Courtesy of the Medical Photography Department,
Naval Medical Center, San Diego, CA.)
|
|
Differential Diagnosis
Epidermal inclusion cysts and
sebaceous cysts of the labia majora may look similar but are generally
smaller. When they are inflamed or infected, maximal fluctuance generally
points toward the external aspect of the labium, as opposed to
Bartholin's gland cysts, which point medially. Occlusion and infection of
apocrine sweat glands can lead to subcutaneous abscess
formation—known as hidradenitis suppurativa. Vulvar hematoma,
leiomyoma, lipoma, and fibromas may occasionally be confused with a
noninfected Bartholin's cyst. Vulvar cancer usually arises in
postmenopausal women and is generally either ulcerated, excoriated, or
exophytic.
Emergency Department Treatment
and Disposition
Simple incision and drainage
(Fig. 10.6) followed by sitz baths provide the most effective and
expeditious relief on an emergency basis. Unfortunately, reocclusion and
reaccumulation of cystic swelling are common. Definitive therapy of
recurrent Bartholin's gland cysts involves marsupialization by suturing
the introital mucosa to the inner cyst wall.
|
|
|
|
|
Bartholin's
Gland Abscess Medial incision
of the cyst yielding purulent fluid, consistent with a Bartholin's
gland abscess. (Courtesy of the Medical Photography Department, Naval
Medical Center, San Diego, CA.)
|
|
Clinical Pearls
1. Antibiotics, although
commonly used, are usually not required.
2. Placement of a Word catheter
into the cyst cavity (Fig. 10.7) decreases the incidence of reocclusion,
but it must be allowed to remain in place for up to 6 weeks to ensure
epithelialization of the drainage tract.
|
|
|

|
|
Bartholin's
Gland Abscess Insertion and
inflation of a Word catheter into the cyst cavity. The free end of
the catheter can be tucked into the vagina for long-term placement,
allowing for epithelialization of the incision site. (Courtesy of the
Medical Photography Department, Naval Medical Center, San Diego, CA.)
|
|
|
|
Spontaneous Abortion
Associated Clinical Features
Spontaneous abortion is
associated with vaginal bleeding and abdominal discomfort. Severe pain,
heavy bleeding with the passage of clots or tissue (Fig. 10.8), and
hypotension may also be present. Threatened abortion is diagnosed
when mild cramping and vaginal bleeding are not accompanied by the
complete or partial extrusion of tissue, cervical dilation, or ectopic
pregnancy. Uterine cramping with progressive dilation of the cervix, with
or without partial extrusion of the products of conception, indicates the
presence of an inevitable abortion (Fig. 10.9). In an incomplete
abortion, some elements of the conceptus have passed, yet retained
intrauterine tissue leads to ongoing uterine cramping, cervical dilation,
and persistent bleeding.
|
|
|
|
|
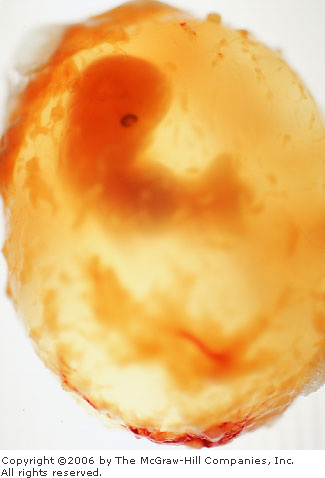
Spontaneous
Abortion Passage of tissue in
a spontaneous abortion at 4 weeks. (Courtesy of Lawrence B. Stack,
MD.)
|
|
|
|
|
|
|
Spontaneous
Abortion Dilation of the
cervical os with partial extrusion of tissue in the setting of an
inevitable abortion. (Courtesy of Robert Buckley, MD.)
|
|
Differential Diagnosis
Ectopic pregnancy should be
considered in all first-trimester females with lower abdominal pain or
vaginal bleeding. The presence of frank tissue passage or cervical
dilation essentially excludes this diagnosis. Large blood clots or an
intrauterine decidual cast (Fig. 10.10), however, may occasionally be
mistaken for products of conception.
|
|
|

|
|
Decidual
Cast A decidual cast or
organized clot may occasionally be mistaken for products of conception.
(Courtesy of the Medical Photography Department, Naval Medical
Center, San Diego, CA.)
|
|
Emergency Department Treatment
and Disposition
Intravenous access, fluid
resuscitation, cross-matching of blood, and urgent gynecologic
consultation should be implemented in the presence of severe pain, heavy
bleeding, or hypovolemia. All tissue should be sent to pathology for
definitive identification. Occasionally, patients who initially have an
open cervical os will rapidly expel the remaining products of conception,
with subsequent resolution of all pain and bleeding. These patients may
be discharged from the ED with the diagnosis of completed abortion if
otherwise clinically stable. Anti-Rh immunoglobulin (RhoGAM) should be
administered in all cases of vaginal bleeding in the pregnant patient
where the mother is Rh-negative and the father is Rh-positive.
Clinical Pearls
1. The passage of large clots
usually indicates rapid heavy bleeding.
2. Completed abortion is
characterized by the passage of tissue, followed by resolution of
bleeding and closure of the cervical os.
3. Fever, leukocytosis, pelvic
tenderness, and malodorous cervical discharge should suggest septic
abortion.
|
|
Genital Trauma and Sexual Assault
Associated Clinical Features
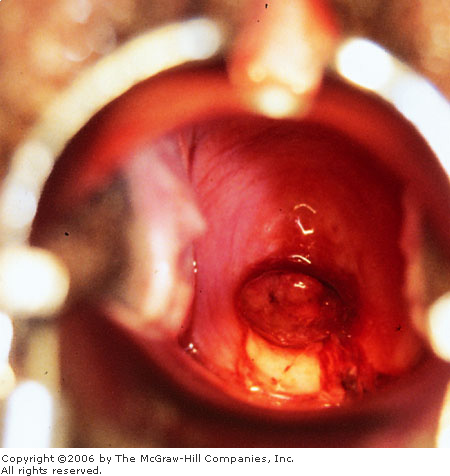
Patients who present for
examination and treatment following an incident of sexual assault are
ideally cared for by a multidisciplinary team capable of addressing the
immediate medical and psychosocial needs of the patient in concert with
forensic and legal requirements. A thorough general examination may
reveal associated contusions and other soft tissue injuries. A meticulous
inspection of the perineum, rectum, vaginal fornices, vagina, and cervix
is required to identify inflicted injuries. Toluidine staining and colposcopy
are often useful in enhancing less apparent injuries such as those to the
posterior fourchette following sexual assault (Fig. 10.11). These are
most commonly found between the 3 and 9 o'clock distribution when the
patient is examined in the dorsal lithotomy position. Perianal
lacerations (Fig. 10.12) may also be seen as toluidine-enhanced linear
tears (Fig. 10.13). Examination of the cervix and posterior vaginal vault
may reveal injuries to those structures (Fig. 10.14).
|
|
|

|
|
Genital
Trauma (Posterior Fourchette)
Linear tears to the posterior fourchette—due to sexual
assault—enhanced by toluidine staining. (Courtesy of Hillary J.
Larkin, PA-C, and Lauri A. Paolinetti, PA-C.)
|
|
|
|
|
|
|
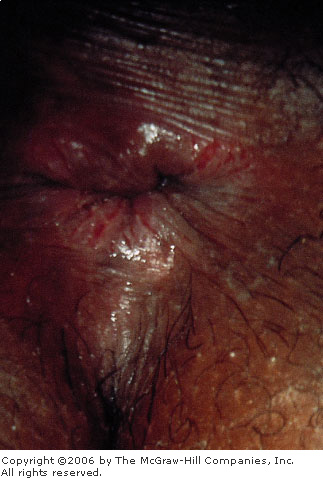
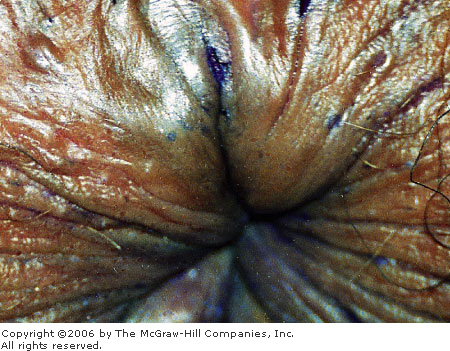
Genital
Trauma (Perianal) Perianal
lacerations following sexual assault. (Courtesy of Hillary J. Larkin,
PA-C, and Lauri A. Paolinetti, PA-C.)
|
|
|
|
|
|
|
Genital
Trauma (Toluidine Staining)
Toluidine staining showing subtle perianal lacerations following
forceful anal penetration. (Courtesy of Aurora Mendez, RN.)
|
|
|
|
|

|
|
Genital
Trauma (Cervix) Cervical
trauma in an elderly victim of sexual assault. Petechiae and freshly
bleeding abrasions are noted from 10 to 3 o'clock. (Courtesy of
Hillary J. Larkin, PA-C, and Lauri A. Paolinetti, PA-C.)
|
|
Differential Diagnosis
Perineal injuries from accidental
trauma may be indistinguishable from those of sexual assault and should
be interpreted in the context of the history. The assessment of assault
or rape is technically a legal one; therefore the examiner should be
careful to document the medical appearance of the wounds rather than
speculate as to the specific mechanism by which each injury occurred.
Emergency Department Treatment
and Disposition
Treatment is preceded by forensic
evidence gathering, consisting of a Wood's lamp examination to identify
semen for collection, pubic hair sampling and combing, vaginal and
cervical smears (air-dried), a cervical and vaginal wet mount to identify
sperm, vaginal aspirate to test for acid phosphatase, and rectal or
buccal swabs for sperm. A prepackaged kit with directions may be
available to facilitate the collection of evidence.
Cervical cultures for Chlamydia
and Neisseria gonorrhoea should be obtained as well as serum
testing for syphilis, hepatitis, and HIV. Empiric antibiotic coverage
against sexually transmitted diseases should be provided and an oral
contraceptive offered (after confirming a nonpregnant state) to prevent
unwanted pregnancy.
Clinical Pearls
1. The medical care of the patient
who has been sexually assaulted should ideally be performed by
experienced supportive staff familiar with the details of forensic
evidence gathering and colposcopic photography.
2. Normal findings on physical
examination and no sperm on wet preparation do not exclude the
possibility of assault.
|
|
Uterine Prolapse
Associated Clinical Features
Uterine prolapse is defined as
the propulsion of the uterus through the pelvic floor or vaginal
introitus. In first-degree prolapse, the cervix descends into the lower
third of the vagina; in second-degree prolapse, the cervix usually
protrudes through the introitus; whereas in third-degree prolapse, or
procidentia, the entire uterus is externalized with inversion of the
vagina (Fig. 10.15). Symptoms include a sensation of inguinal traction,
low back pain, urinary incontinence, and the presence of a vaginal mass.
|
|
|

|
|
Third-Degree
Uterine Prolapse Note the
protrusion of the entire uterus with cervix visible through the
vaginal introitus. (Courtesy of Matthew Backer, Jr., MD.)
|
|
Differential Diagnosis
Uterine prolapse can occasionally
be confused with a cystocele, enterocele, or soft tissue tumor. These
disorders, which may all be accompanied by introital bulging, are easily
distinguished by the absence of cervicouterine descent.
Emergency Department Treatment
and Disposition
Patients with first- or
second-degree prolapse should be referred to a gynecologist for pessary
placement or surgical correction. With procidentia, the uterus should be
manually reduced into the vaginal vault and the patient placed at bed
rest until evaluated by a gynecologic consultant.
Clinical Pearl
1. With procidentia, the
exposed uterus is prone to abrasion and possible secondary infection.
|
|
Cystocele
Associated Clinical Features
A cystocele occurs when there is
relaxation and bulging of the posterior bladder wall and trigone into the
vagina (Fig. 10.16) and is usually due to birth trauma. Patients complain
of bulging or fullness over the introitus that is worsened with Valsalva
(Fig. 10.17) and relieved with recumbency. It is often associated with
urinary incontinence or symptoms of incomplete emptying. Most cystoceles,
however, are asymptomatic. Examination reveals a thin-walled bulging of
the anterior vaginal wall, which, in severe cases, may pass through the
introitus with Valsalva.
|
|
|

|
|
Cystocele Cystocele with bulging of the posterior
bladder wall into the vagina. (Courtesy of Matthew Backer, Jr., MD.)
|
|
|
|
|

|
|
Cystocele Cystocele worsening with Valsalva. (Courtesy
of Matthew Backer, Jr., MD.)
|
|
Differential Diagnosis
An enterocele may lead to a
similar bulging of the anterior vaginal wall but is much less common and
is generally limited to those patients who have had a hysterectomy.
Rectocele, uterine prolapse, and soft tissue tumors should also be
considered.
Emergency Department Treatment
and Disposition
Larger cystoceles or those
associated with urinary symptomatology, pain, or bothersome bulging
should be referred to a gynecologist for further evaluation.
Clinical Pearl
1. Most cystoceles are
asymptomatic and are detected incidentally at the time of pelvic
examination.
|
|
Rectocele
Associated Clinical Features
Most small rectoceles are
completely asymptomatic, though symptoms of introital bulging,
constipation, and incomplete rectal evacuation may occur. Bulging of the
introitus can be seen grossly on physical examination (Fig. 10.18) and
can become worse with Valsalva (Fig. 10.19). Rectovaginal examination
reveals a thin-walled protrusion of the rectovaginal septum into the
lower part of the vagina.
|
|
|

|
|
Rectocele This is characterized by bulging of the
posterior vaginal wall at the introitus. (Courtesy of Matthew Backer,
Jr., MD.)
|
|
|
|
|

|
|
Rectocele Worsening of the rectocele with Valsalva.
(Courtesy of Matthew Backer, Jr., MD.)
|
|
Differential Diagnosis
Cystocele, enterocele, uterine
prolapse, and soft-tissue tumors should all be easily distinguished by
careful inspection.
Emergency Department Treatment
and Disposition
Supportive measures with
hydration, laxatives, and stool softeners are generally all that is
needed to relieve the patient's symptoms. Those patients with large
symptomatic rectoceles who do not desire further childbearing are
candidates for posterior colpoperineorrhaphy.
Clinical Pearl
1. A rectocele is the
herniation of the rectovaginal wall and is usually due to childbirth.
|
|
Imperforate Hymen
Associated Clinical Features
The hymen is a membrane visible
at the introitus that separates the vestibule externally from the vagina
internally. The opening of the hymen can take on a variety of
shapes—annular, semilunar, cribiform, and septate. The congenital
absence of a hymenal orifice is called an imperforate hymen (IH). This
condition may become evident in infants or young children as a smooth,
glistening, protruding membrane due to the buildup of vaginal secretions
known as a mucocolpos. More commonly, an imperforate hymen presents in
adolescent girls with primary amenorrhea and recurrent abdominal pain.
The buildup of menstrual blood and secretions behind the hymen is called
hematocolpos and may become large enough to cause urinary retention by
pressing on the bladder neck.
Physical examination reveals a
smooth, dome-shaped, bluish-red bulging membrane (Fig. 10.20). A large,
smooth, cystic mass can often be palpated anteriorly on digital rectal
examination. Occasionally, the buildup of blood may spill over through
the fallopian tubes into the peritoneal cavity, resulting in signs of
pelvic or abdominal peritonitis.
|
|
|

|
|
Imperforate
Hymen A bulging mass at the
introitus is seen in this patient with abdominal distention and
amenorrhea. The imperforate hymen was diagnosed, with subsequent
incision and drainage of the hematocolpos. (Courtesy of Mark Eich,
MD.)
|
|
Differential Diagnosis
A complete transverse septum,
located in the midvagina, presents similarly to IH but is generally not
visible to simple inspection. Partial and complete vaginal agenesis may
be confused with IH in preadolescents. Both cystocele and rectocele
present as bulging masses at the introitus (see Figs. 10.16, 10.18) but
occur almost exclusively in multiparous women, thus excluding IH from
consideration. The presentation of a bulging membrane at the introitus
may be briefly confused with a bulging amniotic sac—history and
abdominal examination, however, should allow this possibility to be
quickly excluded.
Emergency Department Treatment
and Disposition
Imperforate hymen as well as
other abnormalities of the vaginal outlet should be referred to a
gynecologist for definitive treatment. This includes incision of the
hymen to allow drainage of the hematocolpos. Those instances detected in
preadolescence should ideally be referred to a practitioner who
specializes in pediatric cases.
Clinical Pearl
1. An imperforate hymen
presents in adolescent girls with primary amenorrhea and recurrent
abdominal pain.
|
|
Ectopic Pregnancy: Ultrasonographic Imaging
Associated Clinical Features
Ectopic pregnancy is the leading
cause of maternal obstetric morbidity in the first trimester of
pregnancy. Presentations commonly include mild vaginal bleeding and lower
abdominal pain, but patients can present in shock secondary to massive
hemorrhage. The menstrual history, although often unreliable, may reveal a
missed or recent abnormal menses. The presence of early signs of
pregnancy (breast changes, morning sickness, fatigue) is variable. On
examination, the uterus may be slightly enlarged, and adnexal tenderness
is not always present. The visualization of an intrauterine pregnancy
(IUP) by ultrasound (US) essentially excludes the diagnosis of ectopic
pregnancy, the exception being a rare dual pregnancy (IUP and ectopic).
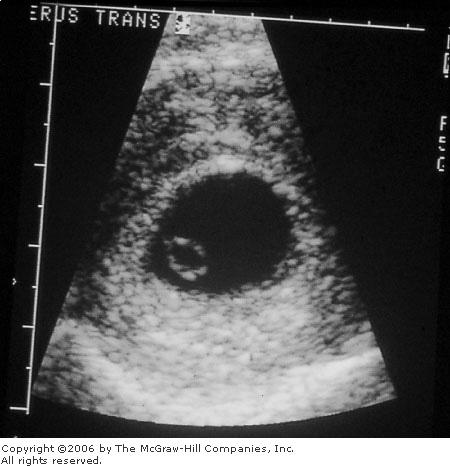
The appearance of a gestational sac at about 5 weeks (Fig. 10.21) is the
first significant finding on US suggestive of an IUP; however,
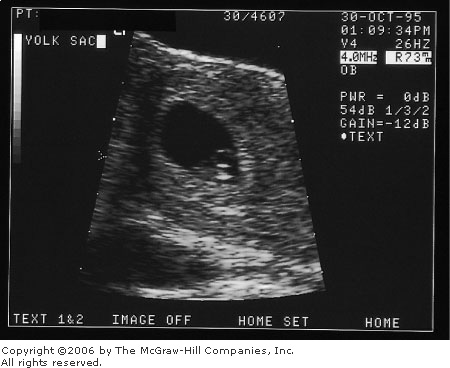
definitive diagnosis of IUP should be deferred until a yolk sac is
present (Fig. 10.22). A fetal pole develops next and can be seen on part
of the yolk sac (Fig. 10.23). The double decidual sac sign is evidence of
a true gestational sac and should be differentiated from the
pseudogestational sac formed from a decidual cast in ectopic pregnancy
(Fig. 10.24). When no gestational sac is visualized ("empty
uterus") (Fig. 10.25), ectopic pregnancy cannot be distinguished
from an early IUP too small to be seen on US.
|
|
|

|
|
|
|
Intrauterine
Gestational Sac Discrete ring
of an intrauterine gestational sac seen on transvaginal ultrasound.
No yolk sac is visualized. A double decidual sac sign is seen,
however, lending evidence of a true gestational sac versus a
pseudogestational sac formed from a decidual cast in ectopic
pregnancy. A thorough look in the adnexa is important in diagnosing
ectopic pregnancy when a gestational sac is the only finding.
(Courtesy of Janice Underwood.)
|
|
|
|
|
|
|
Intrauterine
Yolk Sac Discrete ring of an
intrauterine yolk sac within the gestational sac seen on transvaginal
ultrasound. Definitive diagnosis of IUP should be deferred until a
fetal pole is present in the sac. (Courtesy of Janice Underwood.)
|
|
|
|
|
|
|
|
|
Intrauterine
Fetal Pole Ultrasound image of
an intrauterine pregnancy with a fetal pole consistent with an 8-week
gestation. An umbilical cord can be seen interposed between the yolk
sac and the fetal pole. (Courtesy of Robert Buckley, MD.)
|
|
|
|
|

|
|
|
|
Ectopic
Pregnancy Transvaginal
ultrasound image of a right ectopic pregnancy with a decidual
reaction in the uterus resembling a gestational sac, or
"pseudosac." Visualization of a pseudogestational, or
"single," sac sign could be consistent with an early
gestational sac or an ectopic pregnancy with a uterine decidual cast.
(Courtesy of Janice Underwood.)
|
|
|
|
|

|
|
Empty
Uterus Transvaginal ultrasound
image of an apparently empty uterus. Ectopic pregnancy should be
strongly suspected if a transvaginal ultrasound reveals an empty
uterus in the setting of a serum quantitative hCG level above the
institution's discriminatory zone. (Courtesy of Janice Underwood.)
|
|
Differential Diagnosis
Ectopic pregnancy should be
considered in all first-trimester females presenting to the emergency
department with either lower abdominal pain or tenderness or vaginal
bleeding. A spontaneously completed abortion with an empty uterine cavity
may lead to confusion if the beta human chorionic gonadotropin ( hCG)
level is elevated above the institution's or sonographer's discriminatory
zone [generally between 1000 and 2000 mIU/mL (Third International
Standard)] and clinical evidence for the passage of products of
conception is lacking. Alternative causes of first-trimester lower
abdominal pain or vaginal bleeding include threatened or incomplete
abortion, molar pregnancy, ruptured corpus luteum cyst, adnexal torsion,
urinary tract infection, appendicitis, pelvic inflammatory disease, and
ureteral calculi. hCG)
level is elevated above the institution's or sonographer's discriminatory
zone [generally between 1000 and 2000 mIU/mL (Third International
Standard)] and clinical evidence for the passage of products of
conception is lacking. Alternative causes of first-trimester lower
abdominal pain or vaginal bleeding include threatened or incomplete
abortion, molar pregnancy, ruptured corpus luteum cyst, adnexal torsion,
urinary tract infection, appendicitis, pelvic inflammatory disease, and
ureteral calculi.
Emergency Department Treatment
and Disposition
Unstable patients require
aggressive resuscitation with fluid and blood followed by surgery. Stable
patients with an ultrasound diagnosis consistent with ectopic pregnancy
(Fig. 10.24) warrant immediate gynecologic consultation. Definitive
therapeutic options range from observation in asymptomatic patients with declining
hCG levels, traditional or laparoscopic surgery, to pharmacologic therapy
with methotrexate. Despite the diminished diagnostic accuracy of
ultrasound at lower levels (up to half of all ectopic pregnancies have a
serum hCG level less than 2000 mIU/mL), if there is a strong clinical
suspicion for ectopic pregnancy, gynecologic consultation should be
considered. Those patients in whom a normal IUP is visualized can be
safely discharged with early outpatient follow-up.
Clinical Pearls
1. Ectopic pregnancy should be
considered in all women of reproductive age presenting with vaginal
bleeding, abdominal pain or tenderness, or a missed menstrual period.
2. Failure to visualize an
intrauterine pregnancy by transvaginal ultrasonography by the time the
serum hCG level has reached approximately 1000 mIU/mL or by abdominal
ultrasound once it has reached a level of approximately 6000 mIU/mL is
highly suggestive of the diagnosis of ectopic pregnancy.
3. The ability of ultrasound
and quantitative  hCG to
diagnose ectopic pregnancy is highly dependent on the resolution of the
machine, the skill of the examiner, and the hCG to
diagnose ectopic pregnancy is highly dependent on the resolution of the
machine, the skill of the examiner, and the  hCG
assay used. Thus, every institution and examiner must develop a specific
"discriminatory zone," the level of hCG
assay used. Thus, every institution and examiner must develop a specific
"discriminatory zone," the level of  hCG on
which to base diagnostic decisions. hCG on
which to base diagnostic decisions.
4. A decidual cast in the
uterus of an ectopic pregnancy may resemble a gestational sac of an
intrauterine pregnancy on ultrasound.
5. Consider ectopic pregnancy
in any female of reproductive age presenting with syncope.
|
|
Molar Pregnancy (Hydatidiform Mole)
Associated Clinical Features
Molar pregnancy is part of a
spectrum of gestational trophoblastic tumors that include benign
hydatidiform moles, locally invasive moles, and choriocarcinoma. The
classic clinical presentation is painless first- or early
second-trimester vaginal bleeding with a uterine size larger than the
estimated gestational age based on the last menstrual period. Additional
clinical findings include nausea and vomiting, though this is often
indistinguishable from that found in normal pregnancy.
Signs of preeclampsia in the
first trimester or early second trimester (hypertension, headache,
proteinuria, and edema), are highly suggestive of this diagnosis.
Hyperthyroidism can be found in roughly 5% of cases. Acute respiratory
distress may occur owing to embolization of trophoblastic tissue into the
pulmonary vasculature, thyrotoxicosis, or simply fluid overload.
Moles commonly produce serum hCG
levels greater than 100,000 mIU/mL. The diagnosis is made by ultrasound.
Figure 10.26 demonstrates the classic finding of multiple intrauterine
echoes with no fetus.
|
|
|

|
|
Molar
Pregnancy "Snowstorm"
pattern demonstrating multiple intrauterine echoes with no fetus is
seen on transvaginal ultrasonography in a patient with a molar
pregnancy. Serum  HCG
was > 180,000 mIU/mL. (Courtesy of Robin Marshall, MD.) HCG
was > 180,000 mIU/mL. (Courtesy of Robin Marshall, MD.)
|
|
Differential Diagnosis
Spontaneous abortion and ectopic
pregnancy are much more common that molar disease and can generally be
differentiated based on typical ultrasound findings accompanied by
markedly elevated serum hCG levels.
Emergency Department Treatment
and Disposition
Gynecologic consultation for
dilatation and curettage (D & C) should be obtained in all cases. For
patients who are reliable for follow-up, suction curettage may be
performed in an outpatient setting when the uterine size is less than 16
weeks and there is no evidence of preeclampsia, hyperthyroidism, or
respiratory distress.
All cases must have close
outpatient monitoring of serum hCG levels to rule out the presence of
malignant gestational trophoblastic disease.
Clinical Pearls
1. All patients with
pregnancies of less than 20 weeks' gestation with clinical findings of
preeclampsia should have gestational trophoblastic disease ruled out.
2. A "snowstorm"
pattern on ultrasonography demonstrating multiple intrauterine echoes
with no fetus coupled with a high hCG level is typical of molar
pregnancy.
|
|
Third-Trimester Blunt Abdominal Trauma
Associated Clinical Features
Trauma is a major cause of maternal
and fetal mortality. In addition to the common injuries to a solid organ
and/or hollow viscus associated with blunt abdominal trauma, special
consideration should be given to the possibility of preterm labor,
fetal-maternal hemorrhage, uterine rupture, and, most importantly,
abruptio placentae. Abruptio placentae is defined as the premature
separation of the placenta from the site of uterine implantation. It is
found in up to 50% of major blunt trauma patients and up to 5% of those
with apparent minor injuries. There are generally signs of uterine
hyperactivity and fetal distress when significant placental detachment
occurs. Most patients have vaginal bleeding, although the margins of
detachment are above the cervical os in up to 20%, who therefore have
little or no vaginal bleeding. Laboratory evidence of a consumptive
coagulopathy is occasionally seen with significant abruption. Electronic
fetal monitoring is of paramount importance in all cases of significant
trauma in patients beyond 20 weeks' gestation. As the pregnancy
progresses toward term, a normal heart rate averages between 120 and 160
bpm. Rapid, frequent fluctuations in the baseline are characteristic of
normal "reactivity" (Fig. 10.27). The loss of this reactivity
can occur during a normal sleep cycle, following narcotic administration,
or, most importantly, in the setting of fetal hypoxia or distress (Fig.
10.28). Decelerations are transient reductions in the fetal heart rate.
Late decelerations begin after the contraction begins and return to
baseline well after it ends, with the nadir of the deceleration occurring
after the peak of the uterine contraction. Late decelerations should
suggest fetal hypoxia, especially when they are accompanied by a loss of
normal baseline beat-to-beat variability (Fig. 10.29). Variable
decelerations are characterized by deep, broad decreases in fetal heart
rate, often falling below 100 bpm (Fig. 10.30). They can occur slightly
before, during, or after the onset of a uterine contraction, hence the
term variable. Variable decelerations are caused by the transient
compression of the umbilical cord during a contraction and are rarely
associated with significant hypoxia or acidosis unless they are frequent
or prolonged. They are most commonly appreciated during the second stage
of labor, when forceful uterine compression transiently occludes the
umbilical cord as the infant is propelled through the birth canal.
|
|
|
|
|
Normal
Beat-to-Beat Variability (BBV)
A normal reactive fetal monitor strip showing a baseline heart rate
between 120 and 160 with fluctuations in the short- and long-term
heart rate. (Courtesy of Timothy Jahn, MD.)
|
|
|
|
|
|
|
Loss
of BBV Loss of beat-to-beat
variability (BBV) in the fetal heart rate, which may forewarn of
fetal distress. This same pattern may also be seen during a normal
sleep cycle or following maternal narcotic administration. (Courtesy
of Gerard Van Houdt, MD.)
|
|
|
|
|
|
|
Late
Deceleration The nadir of a
late deceleration always follows the peak of the uterine contraction
with the heart rate approaching the baseline after the completion of
the uterine contraction; this is suggestive of hypoxia. (Courtesy of
James Palombaro, MD.)
|
|
|
|
|
|
|
Variable
Deceleration Variable
decelerations are due to cord compression. They are characterized by
a rapid onset and recovery and may occur slightly before, during, or
after the onset of the contraction. (Courtesy of John O. Boyle, MD.)
|
|
Differential Diagnosis
Another alternative cause of
bright red vaginal bleeding in the third trimester of pregnancy is
placenta previa. This can generally be differentiated from abruption by
the visualization of a low-lying placenta on ultrasound.
Emergency Department Treatment
and Disposition
An obstetrician should be consulted
immediately in all trauma patients beyond 20 weeks' gestation. Blood for
type- and cross-matching, complete blood count, prothrombin time (PT),
partial thromboplastin time (PTT), fibrinogen, and fibrin degradation
products or D-dimer should be obtained.
It is generally recommended that patients undergo continuous tocofetal
monitoring for a minimum of 4 h to rule out preterm labor or fetal
distress. Ultrasound is essential in visualizing placental abruption.
Indications for emergency cesarean section include placental abruption,
signs of ongoing fetal distress, or uncontrolled maternal hemorrhage.
Clinical Pearls
1. Ecchymotic markings imparted
by a significant blunt force (Fig. 10.31) are not always present on a
gravid abdomen; thus, a careful history of the mechanism of trauma and
associated complaints is essential.
2. Anti-Rh immunoglobulin
should be administered for all cases of significant third-trimester blunt
abdominal trauma if the mother is Rh-negative and the father is
Rh-positive.
|
|
|

|
|
Gravid
Abdomen A third-trimester
gravid abdomen with ecchymotic markings imparted by a significant
blunt force. Fetal assessment should occur simultaneously with
maternal resuscitation. (Courtesy of John Fildes, MD.)
|
|
|
|
Ferning Pattern of Amniotic Fluid
Associated Clinical Features
Patients beyond the 20th week of
pregnancy presenting with a history of uncontrolled leakage of fluid
should undergo sterile speculum examination to determine the presence of
amniotic fluid. The diagnosis of membrane rupture can be made by
observing the passage of fluid from the cervix or pooling in the vaginal
vault. Without gross evidence of rupture, secretions from the vaginal
vault can be placed on a slide and allowed to air dry. The characteristic
arborization, or ferning pattern (Fig. 10.32), is diagnostic of amniotic
fluid, thus rupture of the membranes. In addition, the secretions can be
applied to nitrazine paper. The pH of normal vaginal secretions generally
falls between 4.5 and 5.5, whereas amniotic fluid generally ranges
between 7.0 and 7.5, yielding a dark blue tint.
|
|
|
|
|
Ferning
Pattern The arborization
pattern found when a drop of amniotic fluid is allowed to air dry on
a microscope slide, known as ferning. (Courtesy of Robert Buckley, MD.)
|
|
Differential Diagnosis
Urinary incontinence is the most
common alternative diagnosis in a third-trimester patient who presents
with a history of possible membrane rupture. The passage of the cervical
mucous plug, known as bloody show, may rarely be confused with the
passage of amniotic fluid. Although a small, subclinical amniotic fluid
leak can never be completely excluded, the presence of an acid pH, the
absence of gross fluid in the vaginal vault, and ferning all point
against the diagnosis of membrane rupture.
Emergency Department Treatment
and Disposition
All patients with confirmed
ruptured fetal membranes should be admitted to the labor and delivery
area and the obstetric consultant notified, irrespective of the presence
or absence of uterine contractions. The greatest risk to the fetus before
37 weeks is preterm delivery. The fetus at term is at risk for infection
secondary to chorioamnionitis if the time from membrane rupture to
vaginal delivery exceeds 24 h.
Clinical Pearls
1. With a strong suspicion of
membrane rupture by history and no objective evidence of amniotic fluid
on examination, a large sterile pad may be placed on the perineum and the
patient reexamined after brief ambulation. This assumes the absence of
uterine contractions and the presence of a reactive fetal monitor strip.
2. Umbilical cord prolapse
should be excluded with a speculum examination in all cases of membrane
rupture.
|
|
Emergency Delivery: Imminent Vertex
Delivery—Crowning
Associated Clinical Features
The second stage of labor begins
when the cervix is fully dilated, allowing for the gradual descent of the
head toward the vaginal outlet. As the head approaches the perineum, the
labia begin to separate with each contraction and then recede once the
contraction subsides. Crowning is the term applied when the head
separates the labial margins without receding at the end of the
contraction (Fig. 10.33).
|
|
|

|
|
Crowning Descent of the fetal head with separation of
the labia is known as crowning and heralds imminent vertex delivery.
(Courtesy of William Leninger, MD.)
|
|
Emergency Department Treatment
and Disposition
The appearance of crowning
heralds imminent vaginal delivery. Equipment for delivery and neonatal
resuscitation should be brought to the bedside. Both the on-call
obstetric consultant and pediatrician should be notified while
preparations are being made for ED delivery.
Clinical Pearls
1. Primigravida patients may
still require multiple sets of contractions and pushing to fully expel
the head through the vaginal outlet.
2. If meconium secretions are
detected well before delivery, continuous electronic tocofetal monitoring
should be begun and the obstetric and pediatric consultants notified.
|
|
Emergency Delivery: Normal Delivery Sequence
Associated Clinical Features
A gravid female with regular
forceful contractions and the urge to strain (push) can present without
warning. Crowning may be present and heralds imminent vaginal delivery.
Important historical questions include the number of previous
pregnancies, a diagnosis of twin gestations, and whether there is a
history of prenatal care or complications. The presence of greenish brown
fetal stool, known as meconium, is associated with fetal hypoxia and is a
clinical indicator of fetal distress. Fetal bradycardia or late
decelerations (Fig. 10.29) may be present and are also evidence of fetal
distress.
Differential Diagnosis
Complications (discussed below)
should be considered when the progress of delivery is altered or when the
presenting part is something other than the occiput. Twin gestations
should be considered in all emergency deliveries and asked about early in
the history.
Emergency Department Treatment
and Disposition
Intravenous access, oxygen, and
equipment for delivery and neonatal resuscitation (suction, oxygen,
warming light, etc.) are immediately obtained as preparation for the
impending delivery.
Delivery of the Head
As the vertex passes through the
vaginal outlet, extension of the head occurs, followed by the appearance
of the forehead and chin. Extension and delivery of the fetal head can be
facilitated by applying gentle pressure upward on the chin through the
perineum—known as the modified Ritgen maneuver (Fig. 10.34).
Simultaneously, the fingers of the other hand can be used to elevate the
scalp to help extend the head. Once the head has been delivered, the
occiput promptly rotates toward a left or right lateral position. At this
stage, the nuchal region should be swept to detect the presence of a
nuchal umbilical cord (see Fig. 10.45). Before the delivery of the
shoulders, the nasopharynx should be gently suctioned with a bulb syringe
to clear away any blood or amniotic debris. If thick meconium is present,
deeper and more thorough suctioning of the posterior pharynx and glottic
region should be accomplished with a mechanical suction trap, since
aspiration of thick meconium by the newborn can lead to pneumonitis and
hypoxia.
|
|
|

|
|
Modified
Ritgen Maneuver Modified
Ritgen maneuver: upward pressure is applied on the fetal chin through
the perineum. (Courtesy of William Leninger, MD.)
|
|
Delivery of the Shoulders
Delivery of the shoulders
generally occurs spontaneously with little manipulation. Occasionally,
gentle downward traction applied by grasping the sides of the head with
two hands eases the delivery of the anterior shoulder (Fig. 10.35). The
head can then be directed upward to permit the delivery of the posterior
shoulder (Fig. 10.36). Following delivery of both shoulders, the body and
legs are easily delivered. Attention is then directed toward the
immediate care of the newborn. The cord is doubly clamped and ligated
(Fig. 10.37) and inspected for three vessels: two umbilical arteries and
one umbilical vein (Fig. 10.38). The child's pediatrician should be
notified if a two-vessel umbilical cord is found at delivery. The newborn
is immediately placed under a warming lamp for drying and gentle
stimulation while being observed for signs of distress (heart rate <
100, limp muscle tone, poor color, weak cry).
|
|
|

|
|
Anterior
Shoulder Delivery Delivery of
the anterior shoulder is facilitated with downward traction.
(Courtesy of William Leninger, MD.)
|
|
|
|
|
|
|
Posterior
Shoulder Delivery Delivery of
the posterior shoulder with upward traction. (Courtesy of William
Leninger, MD.)
|
|
|
|
|

|
|
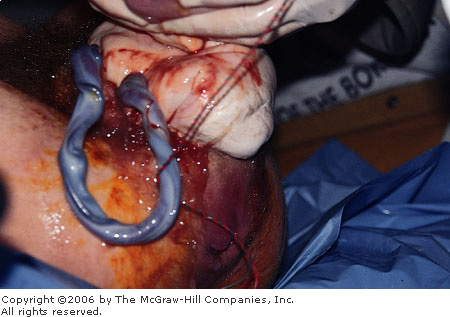
Clamping
the Cord The cord is clamped
immediately after delivery. (Courtesy of William Leninger, MD.)
|
|
|
|
|

|
|
|
|
Normal
Umbilical Cord Cross-sectional
view of the two arteries and single vein of a normal three-vessel
umbilical cord. (Courtesy of Jennifer Jagoe, MD.)
|
|
Delivery of the Placenta
Following delivery, gentle traction
can be placed on the cord while the opposite hand is used to massage the
uterine fundus (Fig. 10.39). The placenta will generally be delivered
within 15 to 20 min (Fig. 10.40) and should be grossly inspected.
Retention of small fragments should be suspected when inspection of the
placenta reveals evidence of a missing segment or cotyledon (Fig. 10.41).
The attending obstetric consultant should be notified, since retained
placental fragments often warrant manual exploration of the uterus,
especially in the context of persistent postpartum bleeding.
|
|
|

|
|
Placenta
Delivery Gentle traction is
applied to the cord while the opposite hand massages the uterus.
(Courtesy of William Leninger, MD.)
|
|
|
|
|

|
|
Placenta
Delivery Delivery of the
placenta. (Courtesy of William Leninger, MD.)
|
|
|
|
|

|
|
|
|
Placenta Placenta with a missing segment or cotyledon.
The missing placental tissue can be seen in the upper left-hand
corner of the photograph. (Courtesy of John O. Boyle, MD.)
|
|
Clinical Pearls
1. Both obstetric and pediatric
consultants should be alerted that preparations are being made for ED
delivery.
2. A two-vessel cord may be
found in about 1 in 500 singleton deliveries and is associated with an
increased incidence of congenital defects.
3. Retained placental fragments
should be considered in the setting of postpartum hemorrhage or
endometritis.
|
|
Umbilical Cord Prolapse in Emergency Delivery
Associated Clinical Features
In an overt cord prolapse, a loop
of umbilical cord is visualized either at the introitus (Fig. 10.42) or
on speculum examination following membrane rupture (Fig. 10.43).
Alternatively, a small loop of cord may be palpated at the cervical os.
In a funic cord prolapse, a loop of umbilical cord is palpated directly
through intact fetal membranes. Occult prolapse occurs when the umbilical
cord descends between the presenting part and the lower uterine segment
but is not visible or directly palpable on examination. Intermittent
compression of the umbilical cord with each uterine contraction may be
detected by the presence of variable decelerations of the fetal monitor
(see Fig. 10.30). The new onset of variable decelerations should always
prompt immediate cervical examination to rule out an overt cord prolapse.
Severe persistent bradycardia may ensue if cord compression is sustained
beyond the duration of the contraction, which is often the case in an
overt prolapse.
|
|
|

|
|
Umbilical
Cord Prolapse Prolapsed
umbilical cord visible at the vaginal introitus in a patient with
twin gestations. (Courtesy of Kevin J. Knoop, MD, MS.)
|
|
|
|
|
|
|
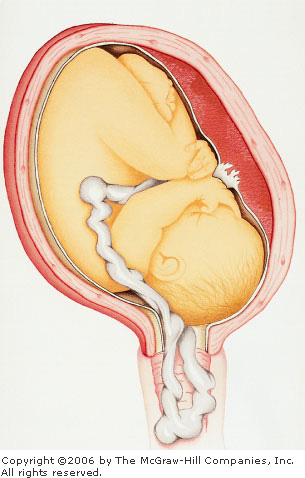
Umbilical
Cord Prolapse Schematic
drawing of an overt prolapse of the umbilical cord through a
partially dilated cervical os. (Courtesy of Judy Christensen.)
|
|
Differential Diagnosis
Rarely, an inexperienced examiner
may mistake a presenting hand or foot for a prolapsed cord. This may be
clarified by careful digital or speculum examination.
Emergency Department Treatment
and Disposition
Prolapse of the umbilical cord
presents an immediate threat to the fetal circulation and constitutes an
obstetric emergency. If an overt prolapse is detected in the ED, the
patient should immediately be placed in a knee-chest position and
continuous upward pressure applied by the examining hand to relieve the
pressure of the presenting part on the lower uterine segment. An
obstetrician should be summoned immediately and the patient taken
directly to the operating room for cesarean delivery. Continuous upward
pressure should be applied to the presenting part of the fetus at all
times during transport. Occasionally, precipitous vaginal delivery may
ensue in the ED shortly after a cord prolapse is detected. Resuscitative
equipment should be available in anticipation of a physiologically
compromised infant. If a funic prolapse is appreciated in the ED, an
obstetrician should be notified and the patient prepared for cesarean
delivery. Under no circumstance should the membranes be broken. Occult
prolapse is rarely appreciated in the ED.
Clinical Pearl
1. Pelvic examination to
exclude umbilical cord prolapse should be performed immediately following
rupture of membranes, the appearance of variable decelerations, or the
detection of bradycardia.
|
|
Breech Delivery
Associated Clinical Features
The incidence of singleton breech
presentation is approximately 3% but rises to higher than 20% in preterm
infants weighing less than 2000 g. In a frank breech, both hips are
flexed and both knees extended. In a complete breech, both hips and knees
are flexed, whereas a footling breech has one or both legs extended below
the buttocks. Frank breech is most common in full-term deliveries,
whereas footling presentation can be found in up to half of all preterm
deliveries. Breech deliveries carry a much higher mortality rate than
cephalic deliveries. Complications of breech delivery include umbilical
cord prolapse, nuchal arm obstruction, and difficulty in delivery of the
following head (Fig. 10.44).
|
|
|

|
|
Breech
Delivery Footling breech
vaginal delivery of the following head. (Courtesy of John O. Boyle,
MD.)
|
|
Emergency Department Treatment
and Disposition
The specific maneuvers for breech
extraction are beyond the scope of this text. If breech delivery appears
imminent, support and gentle traction should be applied as the various
parts spontaneously pass through the vaginal outlet, keeping in mind that
the biparietal diameter is greater than either the bitrochanteric or
bisacromial diameter.
Clinical Pearl
1. Immediate obstetric
consultation should be obtained in all breech deliveries.
|
|
Nuchal Cord in Emergency Delivery
Associated Clinical Features
The circumferential wrapping of
the umbilical cord around the child's neck occurs in about 20% of all
deliveries (Fig. 10.45). Tight approximation of the cord around the
infant's neck can lead to transient disruption of uterine blood flow
during contractions, leading to variable decelerations noted on the fetal
heart rate monitor (Fig. 10.30); it may also impede delivery once the
head passes through the introitus.
|
|
|

|
|
Nuchal
Cord A loose nuchal cord is
seen around the neck. (Courtesy of William Leninger, MD.)
|
|
Emergency Department Treatment
and Disposition
Once a cord is identified around
the neck, it should be slipped over the head using the index and middle
fingers. Occasionally two coils are identified.
Clinical Pearl
1. A loosely applied cord
should be pulled over the child's head. If the cord is wrapped too
tightly, it can be clamped and ligated on the perineum, followed by the
immediate delivery of the shoulders and body.
|
|
Shoulder Dystocia in Emergency Delivery
Associated Clinical Features
Shoulder dystocia is defined as
failure to deliver the shoulders, following delivery of the head, because
of impaction of the fetal shoulders against the pelvic outlet (Fig.
10.46). Risk factors include gestational diabetes, prior delivery of
large infants, and postterm delivery.
|
|
|

|
|
Shoulder
Dystocia Firm approximation of
the fetal head against the vaginal outlet consistent with shoulder
dystocia. (Courtesy of William Leninger, MD.)
|
|
Emergency Department Treatment
and Disposition
Shoulder dystocia is an acute
obstetric emergency, with the immediate life threat being asphyxia from
prolonged delivery. An obstetrician should be summoned immediately.
Equipment for neonatal resuscitation should be set up and, ideally, a
pediatric consultant should be summoned. In the absence of an obstetric
consultant, a wide episiotomy should be performed. The least invasive
maneuver is to forcefully flex the mother's knees toward her chest
(McRobert's maneuver). This extreme dorsal lithotomy position
occasionally allows for the appropriate engagement of the fetal
shoulders. If this is unsuccessful, a Wood's maneuver can be attempted by
hooking two fingers behind the infant's posterior scapula and rotating
the entire body in a screwlike manner. As the posterior shoulder rotates
upward, it can generally be delivered past the symphysis pubis. If the
Wood's maneuver fails to deliver the anterior shoulder, delivery of the
posterior arm may be attempted by inserting two fingers into the sacral
fossa and bringing down the entire posterior arm by flexing it at the
elbow. The remaining anterior shoulder should then deliver, either
spontaneously or else following rotation into the oblique position to
facilitate its delivery.
Clinical Pearls
1. Shoulder dystocia is an
acute obstetric emergency that requires quick action:
Call for help.
Cut a wide episiotomy.
Perform McRobert's maneuver.
Rotate the posterior shoulder.
2. After delivery, look for
fracture of the clavicles or humerus and possible brachial plexus injury.
|
|
Postpartum Perineal Lacerations
Associated Clinical Features
Lacerations to the perineum occur
commonly following a rapid, uncontrolled expulsion of the fetal head.
Postpartum perineal lacerations range from minor to severe.
Differential Diagnosis
Perineal lacerations due to birth
trauma are categorized into four groups. First-degree lacerations are
limited to the mucosa, skin, and superficial subcutaneous and submucosal
tissues (Fig. 10.47). Second-degree lacerations penetrate deeper into the
superficial fascia and transverse perineal musculature (Fig. 10.48). In
addition to these structures, a third-degree laceration disrupts the anal
sphincter, whereas a fourth-degree laceration extends into the rectal
lumen (Fig. 10.49).
|
|
|

|
|
First-Degree
Laceration First-degree
laceration limited to the mucosa, skin, and superficial subcutaneous
and submucosal tissues. There is no involvement of the underlying
fascia and muscle. (Courtesy of Jerry Van Houdt, MD.)
|
|
|
|
|

|
|
|
|
Second-Degree
Laceration There is disruption
of the hymenal ring and the deep perineal musculature, extending into
the vaginal mucosa and transversalis fascia, but no involvement of
the anal sphincter or mucosa. (Courtesy of Pamela Ambroz, MD.)
|
|
|
|
|

|
|
Fourth-Degree
Laceration Fourth-degree
perineal laceration revealing wide separation of the perineal fascia
and anal sphincter. The examiner's small finger is in the rectal
lumen, showing extension of the tear proximally. (Courtesy of Timothy
Jahn, MD.)
|
|
Emergency Department Treatment
and Disposition
In precipitous ED deliveries, the
repair of the episiotomy and/or perineal lacerations can often be
performed by the obstetric consultant, the details of repair being beyond
the scope of this book.
Clinical Pearl
1. Perineal laceration repair
fundamentally involves the sequential anatomic reapproximation, using
absorbable suture material, of the rectal mucosa, anal sphincter,
transverse perineal musculature, vaginal mucosa, and skin.
|
|