|
Note: Large images and
tables on this page may necessitate printing in landscape mode.
Copyright
©2006 The McGraw-Hill Companies. All rights reserved.
Emergency
Medicine Atlas > Part 1. Regional
Anatomy > Chapter 11. Extremity Trauma > Upper
Extremity >
|
Acromioclavicular Joint Separation
Associated Clinical Features
Injury to the acromioclavicular
(AC) joint is a common finding in the ED, resulting from direct trauma
with an adducted arm or indirectly from a fall on an outstretched arm
with pressure directed to the joint (Fig. 11.1). There are three degrees
of injury (Fig. 11.2). A first-degree injury is equivalent to a sprain.
There is an incomplete tear of the ligament. Radiographs are negative. A
second-degree injury consists of subluxation of the AC joint and
disruption of the ligament. Subluxation of the clavicle from the
acromion, of less than 50% the diameter of the clavicle, is only evident
on stress radiographs. Complete disruption of the AC, coracoacromial, and
coracoclavicular ligaments is a third-degree injury. Radiographs reveal
more than 50% displacement of the clavicle from the acromion. All
patients complain of pain at the joint site with moderate to severe
amounts of swelling. Stress radiographs are obtained by suspending 5 to
10 lb of weight from each arm and taking a bilateral anteroposterior (AP)
shoulder film. The joint space and any subluxation are easily visualized.
|
|
|
|
|
Acromioclavicular
Joint Separation Subtle
prominence of the left distal clavicle. The upward displacement of
the clavicle is due to stretching or disruption of the suspending
ligaments. (Courtesy of Frank Birinyi, MD.)
|
|
|
|
|
|
|
Acromioclavicular
Joint Injuries Classification
of acromioclavicular joint injuries. (Adapted with permission from
Rockwood CA, Green DP, Bucholz RW: Rockwood and Green's Fractures in
Adults, 3d ed. Philadelphia: Lippincott; 1991.)
|
|
Differential Diagnosis
Clavicular fracture, scapular
fracture, rotator cuff injury, shoulder dislocation, contusion, or
isolated coracoclavicular ligament damage can be confused with AC joint
separation.
Emergency Department Treatment
and Disposition
First- and second-degree injuries
are treated with rest, ice, analgesics, and a simple sling until acute
pain with movement is relieved. Third-degree injury treatment is
controversial. Many experts advocate immobilization with a sling for 3
weeks, whereas others advocate operative repair. Orthopedic referral is
essential for all third-degree injuries.
Clinical Pearls
1. The AC joint stress test is
an accurate means of testing for AC joint separation. The patient is
instructed to bring the arm across the chest and try to align the opposite
shoulder with the elbow. The production of pain over the AC joint
confirms the diagnosis.
2. Since first- and
second-degree separations are managed conservatively, stress views rarely
alter management.
|
|
Shoulder Dislocation
Associated Clinical Features
Anterior shoulder dislocations
are the most common dislocation seen in the ED. They are caused by
external rotation and abduction that disrupts the capsule and
glenohumeral ligaments. The affected extremity is held in slight
abduction and external rotation. Often, the patient supports the
dislocated shoulder with the other arm. The acromion becomes prominent
and there is a squared-off box-like appearance to the top of the
shoulder. The rounded contour of the deltoid is lost (Fig. 11.3). These
patients complain of shoulder pain and refuse to move the shoulder on the
affected side. Many patients will appear diaphoretic and pale. A
neurologic examination of the upper extremity should be performed to rule
out associated injury, most commonly of the axillary nerve (sensation
over the deltoid). Radiographic examination is necessary to evaluate for
associated fracture (Fig. 11.4). Posterior shoulder dislocations are
commonly missed because of subtle radiographic findings (Figs. 11.5 and
11.6). The arm is held internally rotated and adducted. There is no
external rotation. On examination, a posterior prominence exists.
Posterior dislocations commonly occur during seizures. The Hill-Sachs
deformity (an impaction of the humeral head) can occur in a significant
percentage (11 to 50%) of these patients.
|
|
|

|
|
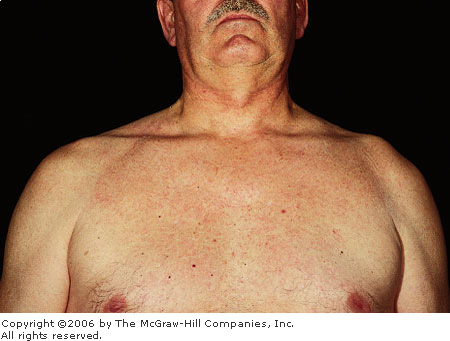
Anterior
Shoulder Dislocation This
right anterior shoulder dislocation occurred when the patient fell
while playing basketball. There is an obvious contour deformity as
well as prominence of the acromion. (Courtesy of Kevin J. Knoop, MD,
MS.)
|
|
|
|
|

|
|
Anterior
Shoulder Dislocation
Radiographic evaluation of this anterior shoulder dislocation
demonstrates that the humeral head is not in the glenoid fossa but is
located anterior and inferior to it. (Courtesy of Kevin J. Knoop, MD,
MS.)
|
|
|
|
|

|
|
Posterior
Shoulder Dislocation AP
radiograph of this rare type of shoulder dislocation. Because of
internal rotation of the greater tuberosity, the humeral head appears
like a dip of ice cream on a cone, thus called the "ice cream
cone sign." (Courtesy of Alan B. Storrow, MD.)
|
|
|
|
|

|
|
Posterior
Shoulder Dislocation A
scapular Y view of the same patient in Fig. 11.5 confirms the
diagnosis. (Courtesy of Alan B. Storrow, MD.)
|
|
Differential Diagnosis
Acromioclavicular separation,
fracture of the greater tuberosity, humeral fracture, and fracture of the
humeral head are commonly mistaken for a shoulder dislocation prior to
radiographic examination.
Emergency Department Treatment
and Disposition
Closed reduction is the treatment
of choice and may require conscious sedation. There are many methods to
reduce shoulder dislocations, including Stimson,
traction-countertraction, and external rotation. Neurovascular and
radiographic examination should occur before and after reduction. The
patient should be placed in a sling and swathe after reduction. The
shoulder should remain immobilized for 2 to 5 weeks (shorter periods for
older patients owing to their greater propensity to develop shoulder
stiffness).
Clinical Pearls
1. Patients with a dislocated
shoulder usually cannot touch the contralateral shoulder with the hand of
the affected side.
2. Relaxation of the pectoral
musculature is an excellent aid in shoulder reduction. This can be accomplished
by manual massage of the muscle. Some patients can relax this muscle
voluntarily when asked to do so (e.g., weightlifters).
3. Luxatio erecta (Fig. 11.7)
is inferior glenohumeral dislocation. The humeral head is forced below
the inferior aspect of the glenoid fossa. These patients present with the
arm locked 180 degrees overhead.
|
|
|
|
|
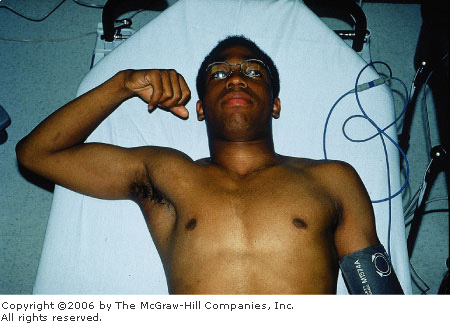
Luxatio
Erecta Hyperabduction may
cause the relatively rare inferior dislocation known as luxatio
erecta. The patient presents with the arm held in elevation and the
humeral head may be palpated along the lateral chest wall. (Courtesy
of Kevin J. Knoop, MD, MS.)
|
|
|
|
Biceps Tendon Rupture
Associated Clinical Features
Rupture of the biceps may occur
anywhere along its route. It occurs most commonly in the dominant
extremity of men between 40 and 60 years of age when an unexpected
extension force is applied to the flexed arm. It may be associated with
chronic bicipital tenosynovitis. When it occurs proximally, the patient
notes a sharp pain in the bicipital groove and the muscle may be noted to
contract within the arm (Fig. 11.8). It may be helpful to have the
patient hold his or her arm abducted and externally rotated at 90
degrees. Flexion at the elbow will cause the biceps to move away from the
shoulder. Rupture may also occur at the tendon insertion into the radial
tuberosity at the elbow, often in an area of preexisting tendon degeneration.
This diagnosis is made on the basis of a history of a painful, tearing
sensation in the antecubital region. A snap or pop may also occur. The
ability to palpate the tendon in the antecubital fossa may indicate
partial tearing of the biceps tendon.
|
|
|

|
|
Biceps
Tendon Rupture The biceps is
noted to contract within the arm after biceps tendon rupture.
(Courtesy of Daniel L. Savitt, MD.)
|
|
Differential Diagnosis
Muscle strain, partial tendon
rupture, and deep venous thrombosis should be considered.
Emergency Department Treatment
and Disposition
Nonoperative treatment consists
of gentle range-of-motion exercises, anti-inflammatory medication, and
physical therapy. This type of treatment results in restoring about 60%
of normal strength of the biceps tendon. Operative treatment of proximal
or distal ruptures is indicated for patients who wish to try to restore normal
strength to the biceps tendon.
Clinical Pearls
1. Early surgical reattachment
to the coracoid, bicipital groove, or radial tuberosity is recommended
for optimal results.
2. Rupture in the belly of the
biceps is treated conservatively.
|
|
Elbow Dislocation
Associated Clinical Features
Dislocations of the elbow can be
anterior, posterior, medial, or lateral. All dislocations require
immediate reduction to relieve pain and prevent circulatory compromise.
Elbow dislocations are caused by a considerable amount of force, and
approximately 40% have an associated fracture. Posterior dislocation is
the most common (Fig. 11.9), occurring after a fall on an outstretched
hand. The arm is extended and abducted. The elbow is held in a flexed
position and is swollen, tender, and deformed. The olecranon is very
prominent. Neurovascular status must be evaluated immediately because of
associated injury. Anterior dislocations are rare. They occur if the
elbow is in a flexed position and is hit from behind on the olecranon. The
elbow is extended with the forearm supinated and elongated. The upper arm
appears shortened. Injury to nerves and vessels is more common with
anterior dislocation.
|
|
|

|
|
Posterior
Elbow Dislocation This patient
dislocated his elbow while playing basketball. Note the flexed
position of the elbow and the prominence of the olecranon. (Courtesy
of Frank Birinyi, MD.)
|
|
Differential Diagnosis
Contusion, radial or ulnar
fracture, or supracondylar fracture of the humerus are commonly confused
with an elbow dislocation until examined radiographically.
Emergency Department Treatment
and Disposition
Most patients require analgesia
and muscle relaxants prior to reduction. After reduction, the elbow
should be immobilized in 90 to 120 degrees of flexion in a posterior
splint and sling. Neurologic and radiographic examination should occur
after any attempt at reduction. The patient should be observed in the ED
for vascular compromise. Elbow dislocations with associated fractures may
make closed reduction difficult and also leave the joint unstable. In
these cases, consultation with an orthopedic surgeon is recommended prior
to reduction attempts.
Clinical Pearls
1. Patients should not be
placed in a circular cast because of the necessity for reexamination.
2. Factors that increase the
index of suspicion for arterial injury include pulselessness prior to
reduction, open dislocations, and concurrent serious traumatic injury.
3. The ulnar nerve is the most
common nerve injured.
4. For posterior dislocations,
palpate the two epicondyles and the tip of the olecranon. If they are in
the same plane, a supracondylar fracture is likely. If the olecranon is
displaced, a dislocation is likely.
|
|
Elbow Fractures
Associated Clinical Features
Direct trauma or fall on an
outstretched hand may result in elbow fractures. The patient is usually
unable to extend the elbow but has pain on supination/pronation. AP,
lateral and oblique views of the elbow should visualize most elbow
fractures. The radial head should be aligned with the capitellum on all
views (Fig. 11.10). The presence of a "fat pad" sign on x-ray
can be indicative of trauma. The anterior fat pad may be seen on normal
radiographs but may be displaced anteriorly and superiorly by effusion or
hemarthrosis (sail sign). The posterior fat pad is not normally
visualized and if seen is indicative of effusion or hemarthrosis (Fig.
11.11).
|
|
|
|
|
Radiographic
Elbow Relationships The
anterior humeral line (1–2) should normally pass through the
middle third of the capitellum. With an extension-type supracondylar
fracture, this line will transect the anterior third of the
capitellum or pass anterior to it. The radiocapitellar line (drawn
through the center of the radius, 3–4) should also pass through
the center of the capitellum. Disruption of this relationship may
indicate fracture of the radial neck or dislocation.
|
|
|
|
|

|
|
Supracondylar
Fracture This radiograph shows
both a pronounced anterior fat pad (sail sign) and posterior fat pad
indicative of a supracondylar fracture. (Courtesy of Alan B. Storrow,
MD.)
|
|
Supracondylar fractures often
occur in patients 5 to 10 years old. At this age the tensile strength of
the collateral ligaments and the joint capsule of the elbow are greater
than the bone itself. Neurovascular insult occurs in 7% of supracondylar
fractures, with the radial, median, and ulnar nerves equally injured. Ulnar
nerve impingement may occur, causing distal neuropraxia or injury.
Capitellum fractures occur from
direct forces, a fall on an outstretched arm, or as an indirect result of
posterior elbow dislocation. With a force directed at the radial head,
shearing of the capitellum causes anterior displacement of the fracture
segment. Radiographically, the joint capsule depicts a swelling along the
anteriorly displaced fragment. This fracture is commonly associated with
fractures of the radial head, which are common but may be subtle and
require a high index of suspicion.
Differential Diagnosis
Posterior elbow dislocation,
nursemaid's elbow, and inter- or transcondylar fractures should be
considered.
Emergency Department Treatment
and Disposition
Treatment of supracondylar
fractures is influenced by angulation and displacement as well as
associated soft tissue injuries (especially neurovascular). Adult
patients usually require surgical intervention. In general, an orthopedic
consultant best handles decisions regarding reduction of significantly
angulated and displaced fractures. If neurovascular compromise exists,
the emergency physician may need to apply forearm traction to reestablish
distal pulses. If the pulse is not restored with traction, emergent
operative intervention for brachial artery exploration or fasciotomy is
indicated. The indications for primary open reduction are (1) those
fractures in which there is inability to obtain a satisfactory closed
reduction; (2) vascular injury; or (3) an associated fracture of the
humerus or forearm in the same limb. In children, nondisplaced,
nonangulated fractures can be splinted (90 degrees of flexion); angulated
fractures require reduction and splinting; and displaced fractures
require reduction and percutaneous pinning on an urgent basis, within 12
to 24 h. Fractures of the capitellum and radial head are treated with
immobilization in a posterior long arm splint with the elbow in 90
degrees of flexion and the forearm in supination, analgesics, and control
of swelling. Complications of displaced capitellum fractures include
arthritis, avascular necrosis, and decreased range of motion. More severe
fractures may need radial head excision to prevent malunion and joint
malfunction. Patients with uncomplicated fractures may begin
range-of-motion exercises within 3 to 7 days to reduce the risk of
permanent loss of elbow motion from joint contracture. Intraarticular
fractures, which may require radial head excision or fixation, should be
referred to an orthopedist within 1 week for definitive management.
Clinical Pearls
1. Ten percent of children with
supracondylar fractures temporarily lose their radial pulse due to joint
swelling after injury. This usually resolves and does not present
long-term sequelae.
2. Capitellum and radial head
fractures often occur together.
3. Bleeding around the elbow
raises suspicion of an open fracture or open joint and requires urgent
orthopedic consultation.
4. The presence of a joint
effusion with a history of trauma is presumptive evidence of a fracture.
|
|
Forearm Fractures
Associated Clinical Features
Fractures of the wrist and elbow
usually involve a fall onto the outstretched arm, while fractures of the
forearm shaft are more commonly the result of a direct blow. Injury to
one of the bones of the forearm is often associated with fracture or
dislocation of the other; therefore one must examine joints above and
below involved bones both radiologically and clinically when injury to
one forearm bone is identified. AP and lateral views of the wrist,
forearm, and elbow are required when a forearm fracture is suspected.
Functional deficits in the hand are important clues to identification of
occult injury to forearm nerve and vascular structures that could require
immediate surgical intervention. Monteggia's fracture-dislocation (Figs.
11.12, 11.13) is an ulnar fracture (usually proximal third) with
associated proximal dislocation of the radial head. Dislocation is
associated with about 7% of ulnar fractures. Forearm shortening can be
noted, and significant forearm swelling is often present. Such a fracture
is associated with significant radial nerve injury in 17% of cases.
|
|
|

|
|
Monteggia's
Fracture Patients with a
Monteggia's fracture present with swelling and pain in the forearm
and often a palpable radial head in the antecubital fossa. (Courtesy
of Alan B. Storrow, MD.)
|
|
|
|
|

|
|
Monteggia's
Fracture Radiograph A
Monteggia's fracture is defined by a fracture of the proximal
one-third of the ulna combined with dislocation of the radial head.
(Courtesy of Alan B. Storrow, MD.)
|
|
Galeazzi's fracture-dislocation
is a fracture of the distal one-third of the radius with dislocation of
the distal radioulnar joint. It occurs three times more often than a
Monteggia fracture. Tenderness over the distal radioulnar joint is noted,
in addition to swelling, tenderness, and possibly deformity at the
fracture site.
Isolated fractures of the middle
ulna may result from direct trauma and are termed nightstick fractures.
High-energy injuries to the forearm may result in fractures of both the
radius and ulna at midshaft, resulting in a grossly deformed and unstable
injury.
Differential Diagnosis
Simple contusion, compartment
syndrome, and muscular injuries should be considered.
Emergency Department Treatment
and Disposition
Both Monteggia's and Galeazzi's
fracture-dislocations require orthopedic consultation and are treated
with immobilization in a long-arm splint (with elbow flexed at 90
degrees). The forearm is placed in a neutral position for a Monteggia
fracture and pronated for Galeazzi fracture. Treatment is usually
surgical for both injuries, although children may be treated by reduction
and casting.
Clinical Pearls
1. Any ulnar fracture with
greater than 10 degrees of angulation or with a bony fragment displaced
more than 50% of the bones' diameter is considered displaced and requires
surgical correction.
2. Isolated proximal ulnar
fractures are rare. Always suspect a Monteggia fracture-dislocation and
closely examine the radial head for dislocation or other evidence of
injury. A line drawn through the radial shaft and head must align with
the capitellum in all views to exclude dislocation (see Fig. 11.10).
3. A distal ulnar styloid
fracture, if found, can be a clue to a Galeazzi's fracture. It is
associated with Galeazzi's injury in approximately 60% of cases.
4. Fractures of the forearm may
result in compartment syndrome.
|
|
Fractures of the Distal Radius
Associated Clinical Features
Falls on an outstretched arm are
common and the forces involved with this mechanism of injury are often
significant enough to break both the radius and the ulna. Open fractures
are common, and one must look closely for overlying soft tissue injury.
Distal radial fractures account for 17% of all fractures treated in the
ED. In the elderly they are usually extraarticular metaphyseal fractures,
whereas in younger patients they are usually intraarticular with
displacement of the joint surface. There are four types of radial
fractures, associated with commonly known eponyms: Colles' fracture,
Smith's fracture, Barton's fracture and Hutchinson's (chauffeur's)
fracture.
A Colles' fracture is dorsal
displacement and angulation of the distal radius and is the most common
wrist fracture in adults. Colles' fracture is usually an extension injury
associated with significant bony displacement and obvious "dinner
fork" deformity on physical examination (Fig. 11.14).
|
|
|

|
|
Colles'
Fracture The classic
dinner-fork deformity is demonstrated in this photograph. The distal
forearm is displaced dorsally. (Courtesy of Cathleen M. Vossler, MD.)
|
|
Smith's fracture is a distal metaphyseal fracture with
volar displacement and angulation. This usually results from a blow to
the dorsum of the wrist or hand or a hyperflexion injury. Radiography
reveals distal volar displacement. Examination reveals deformity and pain
in the distal radius (Figs. 11.15, 11.16, 11.17).
|
|
|

|
|
Smith's
Fracture A Smith's fracture is
sometimes described as a reverse Colles'. (Courtesy of Frank Birinyi,
MD.)
|
|
|
|
|

|
|
Smith's
Fracture The radiograph
reveals volar displacement of the distal radial fragment together
with the bones of the wrist and hand. (Courtesy of Frank Birinyi,
MD.)
|
|
|
|
|
|
|
Distal
Forearm Fractures These
illustrations depict three different types of distal forearm
fractures: Smith's, Barton's, and Hutchinson's. (Adapted from Simon
R: Emergency Orthopedics: The Extremities. Norwalk, CT: Appleton
& Lange; 1987, pp 118–119.)
|
|
Barton's fracture (Fig. 11.17) is
a fracture of the dorsal rim of the distal radius. The rim of the distal
radius, commonly a triangular bone fragment, is displaced dorsally. It
may be associated with dislocation of the radiocarpal joint.
A chauffeur's or Hutchinson's
fracture (Fig. 11.17) is an avulsion fracture of the distal radial
styloid that occurs from a force transmitted from the scaphoid to the
styloid. It may be considered an unstable fracture secondary to an
associated ligamentous injury.
Emergency Department Treatment and
Disposition
ED evaluation and management of
these fractures is similar because certain fracture characteristics
define instability. Comminuted, displaced, unstable, and open fractures
or those with neurologic or vascular compromise require prompt orthopedic
attention. In addition, fractures with greater than 20 degrees of
angulation or with more than 1 cm of shortening are potentially unstable
and deserve aggressive management. Initial immobilization can be
accomplished with a double sugar-tong splint. Stable fractures respond
well to closed reduction and casting for 6 to 8 weeks. Most closed
Colles' and Smith's fractures can be managed with closed reduction in the
ED with use of finger traps, local anesthesia via hematoma or Bier block,
and gentle manipulation to restore anatomic alignment. Detailed discharge
instructions should be given regarding symptoms of median nerve
impingement, including paresthesias and hand weakness, which should
prompt return to the ED.
Clinical Pearls
1. All fractures of the distal
radius must be evaluated for median nerve function before and after
reduction.
2. Colles' fractures warrant a
high index of suspicion for intraarticular injury, especially when a
radial styloid fracture is noted.
3. With a Hutchinson's
fracture, associated ligamentous injuries should be sought, especially
scapholunate dissociation and perilunate and lunate dislocation.
|
|
Carpal and Carpometacarpal Dislocations
Associated Clinical Features
Carpal and carpometacarpal
dislocations are serious wrist injuries usually occurring from
hyperextension. Their diagnosis requires careful physical and
radiographic examination. Patients complain of decreased range of motion,
pain, swelling, and ecchymosis.
Lunate dislocation (Fig. 11.18)
can occur in a volar or dorsal position with the lunate displaced
relative to the other carpal bones (Fig. 11.19). The normal lunoradial
relationship is disrupted. The median nerve is most commonly involved and
should be evaluated.
|
|
|

|
|
Lunate
Dislocation This photograph
demonstrates swelling associated with a volar lunate dislocation.
(Courtesy of Cathleen M. Vossler, MD.)
|
|
|
|
|

|
|
Lunate
Dislocation Radiographic
examination of a dorsal lunate dislocation. (Courtesy of Cathleen M.
Vossler, MD.)
|
|
If the lunoradial articulation is intact and the
other carpal bones are dislocated relative to the lunate, it is termed a
perilunate dislocation. (Figs. 11.20, 11.21).
|
|
|

|
|
Perilunate
Dislocation This patient
sustained a fall on his outstretched hand with impact on the palm.
The force transmitted through the radius and lunate disrupted the
lunate-capitate articulation. The capitate and other carpal bones
were driven posteriorly with respect to the lunate, resulting in the
prominent dorsal deformity. (Courtesy of Alan B. Storrow, MD.)
|
|
|
|
|

|
|
Perilunate
Dislocation This slightly
oblique radiograph of the patient in Figure 11.20 reveals dorsal
displacement of the carpal bones in relation to the lunate. The
lunate does have slight anterior rotation, although its relationship
with respect to the distal radius is intact. (Courtesy of Alan B.
Storrow, MD.)
|
|
Another potentially serious injury is scapholunate
dislocation, often mistakenly diagnosed as a sprained wrist. Although the
physical examination may be unremarkable except for wrist pain, an
anteroposterior (AP) radiograph reveals a widening of the scapholunate
joint space (Fig. 11.22). This space is normally less than 3 mm. A space
of 4 mm or greater should prompt suspicion of this problem. In addition,
the lateral radiograph may reveal an increase of the scapholunate angle
to greater than 60 to 65 degrees (normal 45 to 50 degrees).
|
|
|

|
|
Scapholunate
Dislocation Radiographic
evidence of a scapholunate dislocation. Note the widened scapholunate
joint space. This injury is often misdiagnosed as simple wrist
sprain. (Courtesy of Alan B. Storrow, MD.)
|
|
All these dislocations may present with concomitant
fractures of the carpal bones or distal forearm. A scaphoid fracture is
particularly troublesome, since misdiagnosis of this problem can result
in later delayed healing or avascular necrosis (Fig. 11.23). This
potentially serious problem is due to lack of a direct blood supply to
the proximal portion of the bone. Tenderness on palpation of the anatomic
snuffbox, or with axial loading, is a common finding. Unfortunately,
negative radiographs do not rule out an occult scaphoid fracture.
|
|
|

|
|
Scaphoid
Fracture Fracture of the
wrist, or middle third, of the scaphoid. These injuries can be
associated with delayed healing and avascular necrosis. (Courtesy of
Alan B. Storrow, MD.)
|
|
Carpometacarpal dislocations are fortunately rare,
since they are often devastating injuries requiring extensive repair
(Fig. 11.24). Functional loss is marked and common.
|
|
|
|
|

|
|
Carpometacarpal
Dislocation This uncommon
injury occurred after a fall from a ladder onto an outstretched hand.
Note the prominent deformity of the proximal metacarpals, II to IV,
on the dorsal hand. Also note the normal prominence of the ulnar
styloid, which helps the examiner in anatomic localization of the
dislocation (A). Radiographic examination of the patient depicted
above (B). (Courtesy of Alan B. Storrow, MD.)
|
|
Differential Diagnosis
Arthritis, carpal tunnel
syndrome, and joint infections should be considered in patients with
wrist pain.
Emergency Department Treatment
and Disposition
Initial management includes
adequate radiographic evaluation followed by ice, elevation, and
splinting. Referral to a hand specialist is essential for adequate
reduction and long-term care.
Clinical Pearls
1. A true lateral wrist
radiograph best demonstrates a lunate dislocation by exhibiting the usual
cup-shaped lunate bone as lying on its side and displaced either dorsally
or volarly.
2. On lateral wrist
radiographs, the metacarpal, capitate, lunate, and radius should all be
aligned so that a line drawn through the long axis will bisect all four
bones including the lunate. If this is not found, then some element of
dislocation, subluxation, or ligamentous instability exists.
3. Patients in whom there is a
clinical suspicion of an occult scaphoid fracture (anatomic snuff-box
tenderness or axial load tenderness of the thumb without radiologic
evidence of fracture) should receive a thumb spica splint and a repeat
examination in 7 to 10 days.
|
|
Clenched Fist Injury
Associated Clinical Features
The clenched fist injury
classically occurs during a fight when the metacarpophalangeal (MCP)
joint contacts human teeth, resulting in a laceration in the skin (Fig.
11.25). Many patients will not divulge the true circumstances surrounding
the injury; therefore all wounds at the MCP joint are considered a
clenched fist injury until proven otherwise. Once these wounds occur, the
inoculated organisms are sealed in a warm, closed environment, allowing
rapid spread and destruction. Serious complications can result, including
infection, loss of function, and amputation. Most wounds are
polymicrobial. Patients who present initially may have little evidence of
intra-articular injury on physical examination, whereas those who present
more than 18 h after injury are more likely to have evidence of
infection, including pain, swelling, erythema, and purulent drainage.
|
|
|

|
|
Clenched
Fist Injury The small
lacerations seen in this photograph were sustained from human teeth
during a fight. Note the subtle black ink bar stamp across the
proximal metacarpals of the right hand; this may reveal a clue about
the wound's etiology. (Courtesy of Lawrence B. Stack, MD.)
|
|
Differential Diagnosis
Abrasions or lacerations
secondary to a source other than human teeth can be mistaken for a
clenched fist injury.
Emergency Department Treatment
and Disposition
All wounds should be irrigated,
debrided, explored, elevated, and immobilized. Patients should receive
antibiotics directed at both oral and skin flora. Tetanus prophylaxis is
given if needed. Radiographs should be obtained to evaluate for fractures
and any foreign bodies remaining in the wound. These wounds should never
be closed initially. All patients require careful follow-up with a hand
specialist. Reliable patients who present early, without evidence of
infection or significant medical history (e.g., diabetes), and no
involvement of bone, joint, or tendon may be treated on an outpatient
basis. They must return in 24 h for a wound check, sooner if any signs of
infection develop. Any patient who does not meet these requirements must
be hospitalized for intravenous antibiotics and wound care.
Clinical Pearls
1. Complications include
cellulitis, lymphangitis, septic arthritis, abscess formation,
osteomyelitis, and tenosynovitis.
2. All wounds need to be
examined in full flexion and extension so that tendon injuries are not
missed. A tendon injury sustained with the fingers flexed will be missed
if the hand is examined only in extension due to the retraction of the
tendon with extension.
|
|
Boxer's Fracture
Associated Clinical Features
A boxer's fracture is a
metacarpal neck fracture of the fifth and sometimes fourth digit, which
commonly occurs after a direct blow to the metacarpophalangeal joints of
the clenched fist. The proximal metacarpal bone is angulated dorsally and
the metacarpal head is angulated volarly. On physical examination, the
"knuckle" is missing and can be palpated on the volar surface
(Figs. 11.26, 11.27). Any associated laceration should be considered secondary
to impact with human teeth ("fight bite," see "Clenched
Fist Injury" Fig. 11.25).
|
|
|

|
|
Boxer's
Fracture This boxer's fracture
occurred when the patient punched a wall with his hand. There is loss
of the "knuckle" when the dorsum of the hand is examined,
especially noticeable when the patient makes a fist. (Courtesy of
Cathleen M. Vossler, MD.)
|
|
|
|
|

|
|
Boxer's
Fracture Radiographic
examination reveals a fracture through the neck of the metacarpal and
volar displacement of the fractured segment. (Courtesy of Cathleen M.
Vossler, MD.)
|
|
Differential Diagnosis
Fracture of the metacarpal head
or metacarpal shaft, hematoma, sprain, clenched fist injury, and
metacarpophalangeal dislocation are often mistaken for a boxer's fracture
until radiographic evaluation is performed.
Emergency Department Treatment
and Disposition
Prior to reduction, the injury
must be evaluated for rotational malalignment. This is easily done by
having the patient place all fingers in the palm; all fingers should
point to the scaphoid bone (Fig. 11.28). Rotational deformities of
greater than 15% require reduction. An ulnar nerve block provides
sufficient anesthesia for the fifth metacarpal, but median and radial
nerve blocks should be used for the other metacarpals. Hematoma block can
be used as an alternative. Once adequate anesthesia is achieved,
reduction can be attempted. A nondisplaced nonangulated fracture requires
no reduction. Treatment includes ice, elevation, and immobilization in a
gutter splint. For reduction, the distal interphalangeal (DIP), proximal
interphalangeal (PIP), and metacarpophalangeal (MCP) joints are all held
in flexion at 90 degrees. Pressure is exerted on the proximal phalanx,
directed upward to push the metacarpal head dorsally back into position.
At the same time, the metacarpal shaft is stabilized with pressure on the
dorsum over the shaft. The patient should be splinted with the MCP at 90
degrees of flexion. Postreduction radiographs are necessary to ensure
adequate reduction. Early follow-up (within 7 days) with a hand
specialist is essential, since simple splinting may not adequately
maintain proper reduction and fractures with higher degrees of angulation
and instability may require fixation.
|
|
|

|
|
Rotational
Deformity Malpositioning of
the right fifth digit due to a boxer's fracture. Normally, all the
digits point toward a single spot on the scaphoid. (Courtesy of
Alexander T. Trott, MD.)
|
|
Clinical Pearls
1. Fractures of the second and
third metacarpal neck will not tolerate any angulation and require
orthopedic referral for anatomic reduction. Fractures of the fourth and
fifth metacarpal neck can tolerate up to 30 and 50 degrees of angulation,
respectively, before function is impaired.
2. Subtle malrotation can be
recognized by looking at the alignment of the nail beds with the digits
flexed. Complications include collateral ligamentous damage, extensor
injury damage, and malposition or clawing of the fingers secondary to
incomplete reduction.
|
|
Peripheral Nerve Injury
Associated Clinical Features
Ulnar nerve injury results in the
classic claw-hand deformity (Fig. 11.29) because of the wasting of small
hand muscles. The deformity is formed by hyperextension of the
metacarpophalangeal joint and flexion at the proximal and distal
interphalangeal joints of the fourth and fifth digits. There is wasting
of the interosseous and hypothenar muscles, as well as the hypothenar
eminence (Fig. 11.30). The patient is unable to abduct or adduct the
digits.
|
|
|

|
|
Claw
Hand This photograph
demonstrates the claw-hand appearance resulting from median and ulnar
nerve injury. Note metacarpophalangeal joint hyperextension.
(Courtesy of Daniel L. Savitt, MD.)
|
|
|
|
|

|
|
Claw
Hand Atrophy of the thenar and
hypothenar eminences also occurs as a result of damage to the median
and ulnar nerves, respectively. Note the concavity to the hypothenar
eminence. (Courtesy of Cathleen M. Vossler, MD.)
|
|
Median nerve damage also results
in the claw-hand deformity, but to the second and third digits. Damage to
the proximal portion of the nerve results in weakness of wrist flexion,
forearm pronation, thumb apposition, and flexion of the first three
digits. Atrophy of the thenar eminence also occurs. There is a sensory
loss over the area of distribution for each nerve. These findings are not
seen acutely but are chronic signs from an old injury.
Wrist drop is the most common
symptom seen with radial nerve damage, occurring in situations of acute
compression. It is frequently referred to as Saturday night palsy (as
when a person who has been drinking alcohol falls asleep on an arm or
with the arm over a chair and there is temporary damage to the nerve).
Differential Diagnosis
Rheumatoid arthritis,
osteoarthritis, and undiagnosed proximal (cervical osteophyte) or distal
(carpal tunnel syndrome) entrapment syndromes can be mistaken for
peripheral nerve injury.
Emergency Department Treatment
and Disposition
Treatment is aimed at recognizing
the underlying cause of the nerve damage. Such causes include laceration
of the nerve, compression from swelling, or hematoma formation. In the
ED, splinting and appropriate referral is the treatment.
Clinical Pearl
1. Long-term nerve injury
results in muscle wasting. Prior to any nerve damage, the thenar and
hypothenar eminences have a full appearance. This is lost in patients
with nerve damage. Initially, there is flattening of each eminence,
followed by a concave or hollow appearance.
|
|
Bennett's and Rolando's Fractures
Associated Clinical Features
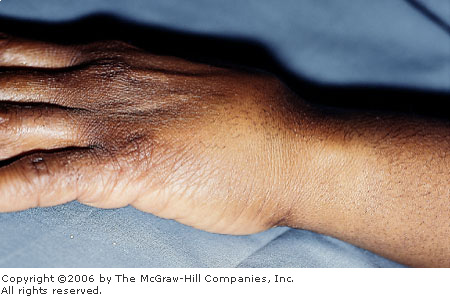
These patients complain of pain,
swelling, and decreased range of motion at the base of the thumb (Fig.
11.31). Bennett's fracture is an intraarticular fracture at the ulnar
aspect of the base of the first metacarpal with disruption of the
carpometacarpal joint (Fig. 11.32). The first metacarpal is displaced
radially and proximally, with subluxation or complete dislocation (Fig. 11.33).
Rolando's fracture is an intraarticular comminuted fracture at the base
of the first metacarpal, with dorsal and volar fragments resulting in a
Y- or T-shaped intraarticular fragment (Fig. 11.34).
|
|
|

|
|
Bennett's
Fracture Bennett's fracture
involves the base of the first metacarpal. The digit is swollen and
ecchymotic over the affected area. (Courtesy of Daniel L. Savitt,
MD.)
|
|
|
|
|

|
|
Bennett's
Fracture Radiographic
examination of a Bennett's fracture illustrates an intraarticular
fracture at the base of the first metacarpal with the metacarpal
displaced radially and proximally. (Courtesy of Cathleen M. Vossler,
MD.)
|
|
|
|
|
|
|
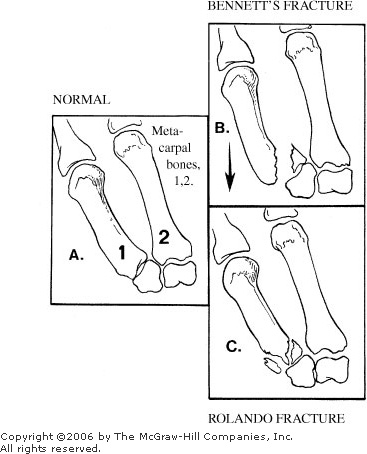
Intraarticular
Fractures of the First Metacarpal Base (A). An intraarticular fracture at the base of
the first metacarpal with radial and proximal displacement is a
Bennett's fracture (B). A comminuted intraarticular fracture at the
base of the first metacarpal is a Rolando's fracture (C).
|
|
|
|
|

|
|
Rolando's
Fracture Note the comminuted
intraarticular fracture at the base of the first metacarpal.
(Courtesy of Cathleen M. Vossler, MD.)
|
|
Differential Diagnosis
Sprain, fracture of the first
metacarpal shaft, or a gamekeeper's thumb (disruption of the ulnar
collateral ligament of the metacarpophalangeal joint) are commonly
mistaken for Bennett's or Rolando's fracture prior to radiographic
evaluation.
Emergency Department Treatment
and Disposition
The treatment of these fractures
in the ED consists of ice, elevation, and immobilization in a thumb spica
splint and early referral to a hand specialist. These fractures generally
require operative reduction and fixation.
Clinical Pearls
1. Carpometacarpal dislocations
are frequently difficult to reduce and require open reduction and fixation
approximately 50% of the time.
2. Osteoarthritis is a common
long-term complication, even after optimal management.
|
|
Boutonnière and Swan Neck Deformities
Associated Clinical Features
The boutonnière deformity is a
result of injury or disruption to the insertion of the extensor tendon on
the dorsal base of the middle phalanx. Common causes of this problem are
proximal interphalangeal (PIP) joint contusion, forceful flexion of the
PIP joint against resistance, and palmar dislocation of the PIP joint.
Initially, a deformity may be absent but will develop over the course of
time if the injury remains untreated. The lateral bands sublux and exert
a proximal pull on the middle phalanx. The result is flexion of the PIP
joint and extension of the DIP joint (Figs. 11.35, 11.36).
Radiographically, a small fragment of bone may be visualized at the
proximal portion of the dorsal aspect of the middle phalanx.
|
|
|
|
|
Boutonnière
Deformity This depiction of a
boutonnière deformity illustrates the rupture of the central slip and
the resultant subluxation of the lateral bands. The subluxation
exerts a pull on the middle phalanx resulting in the deformity.
|
|
|
|
|

|
|
Boutonnière
Deformity A boutonnière
deformity of the fourth digit. Note the flexion of the PIP joint and
the extension of the DIP joint. (Courtesy of E. Lee Edstrom, MD.)
|
|
Swan-neck deformity occurs as a result of the
shortening of interosseous muscles secondary to systemic diseases such as
rheumatoid arthritis. The digit is contorted with hyperextension of the
PIP and flexion of the distal interphalangeal (DIP) and
metacarpophalangeal (MCP) joints (Fig. 11.37).
|
|
|

|
|
Swan-Neck
Deformity A swan-neck
deformity of the index finger. Note the hyperextension of the PIP
joint and the flexion of the DIP joint. (Courtesy of Cathleen M.
Vossler, MD.)
|
|
Differential Diagnosis
Fracture, dislocation, or tendon
damage can be mistaken for a boutonnière or swan neck deformity.
Emergency Department Treatment
and Disposition
In dealing with a closed injury
resulting in a boutonnière deformity, immobilization of the PIP joint in
extension is adequate. Splinting the MCP and DIP joints is not necessary.
The splint should be used for 4 weeks, at which point active range of
motion can start. Open injuries must be carefully explored and repaired.
Swan-neck deformities are treated by splinting the digit to prevent further
deformity. Both deformities require referral to a hand specialist.
Clinical Pearls
1. Boutonnière deformity
generally develops weeks after the initial injury as the lateral bands
contract; therefore, it is frequently missed in the ED. Early diagnosis can
be made with the proper examination of the finger. The digit should be
adequately anesthetized and then examined for range of motion and joint
stability.
2. Any injury involving the
dorsal PIP surface should be reexamined for development of a boutonnière
deformity after 7 to 10 days.
3. Surgical repair may be
required for cases where conservative therapy yields inadequate results.
|
|
High-Pressure Injection Injury
Associated Clinical Features
A large number of commercial
devices are able to deliver liquids and gases at high pressures.
Occasionally, substances from these devices are injected into the body,
especially the upper extremities. The most common devices include spray
guns, diesel injectors, and hydraulic lines. The injury occurs when the
device accidentally fires during cleaning or mishandling. The injury can
be very misleading if seen soon after the event. On early examination, a
small puncture wound or no apparent break in the skin may be found, with
minimal swelling. Swelling and pain increase over time (Fig. 11.38).
Vascular compromise can occur directly from compression secondary to
swelling or from the inflammatory response that the body produces to the
materials injected. The injected material tends to spread along fascial
planes, so the extent of injury can be quite misleading and is often
subtle on initial presentation.
|
|
|

|
|
High-Pressure
Injection Injury This
photograph illustrates injury incurred by a grease gun. The patient
was cleaning the device and the gun accidently discharged into his
hand. Note the swelling and erythema. The patient was taken to the
operating room for initial debridement. (Courtesy of Richard
Zienowicz, MD.)
|
|
Differential Diagnosis
Puncture wound, hematoma, or
tenosynovitis can be confused with a hydraulic pressure injury.
Emergency Department Treatment
and Disposition
Immediate operative debridement
is the treatment of choice. Therefore, early consultation with a hand
specialist is necessary. Radiographic examination evaluates for fracture
and may outline spread of injected material. Tetanus and broad-spectrum
antibiotics should be administered. The affected extremity should be
elevated and splinted.
Clinical Pearls
1. Do not be misled by the
"benign" appearance of the initial injury.
2. Delays in treatment can lead
to compartment syndrome.
3. Digital blocks are
contraindicated because of the potential for increased tissue pressure
and compromise of tissue perfusion.
|
|
Phalangeal Dislocations
Associated Clinical Features
Phalangeal dislocations are
common and can occur at all three finger joints. Distal interphalangeal
(DIP) dislocations are the rarest but can occur when a force is applied
to the distal phalanx. Gross deformity is noted on examination, with the
distal phalanx generally displaced dorsally. Proximal interphalangeal
(PIP) dislocations (Figs. 11.39, 11.40) are common and easily reducible.
These are generally dislocated dorsally, caused by hyperextension, and
may have associated damage to the volar plate (Fig. 11.41). PIP volar
dislocations can be irreducible secondary to rupture of the extensor
tendon or herniation of the proximal phalanx through the extensor mechanism,
both requiring operative repair. Metacarpophalangeal (MCP) joint dorsal
dislocations are often due to hyperextension.
|
|
|

|
|
Phalangeal
Dislocation This patient
dislocated the long finger PIP joint during an altercation. The PIP
joint is displaced dorsally with an obvious deformity. (Courtesy of
Cathleen M. Vossler, MD.)
|
|
|
|
|

|
|
Phalangeal
Dislocation This photograph
illustrates medial angulation of the ring finger, suggesting PIP
dislocation. (Courtesy of Daniel L. Savitt, MD.)
|
|
|
|
|

|
|

|
|
Volar
Plate Injury This photograph
demonstrates the subtle PIP swelling and ecchymosis of the third
(long) digit often seen with a volar plate injury (A). Hyperextension
injuries cause disruption of the volar plate and result in swelling,
ecchymosis, and tenderness along the volar aspect of the joint. These
injuries are initially treated conservatively with splinting, but if
they are unstable, operative repair is required. (Courtesy of Daniel
L. Savitt, M.D.) Radiographic examination of the digit reveals a
small fragment on the proximal volar surface of the PIP joint (B).
(Courtesy of Cathleen M. Vossler, MD.)
|
|
Differential Diagnosis
Phalangeal fracture, metacarpal
fracture, tendon damage, ligamentous injury, or boutonnière deformity can
be confused with a phalangeal dislocation.
Emergency Department Treatment
and Disposition
Digital nerve block is
appropriate anesthesia for the PIP and DIP joints. Ulnar, median, or
radial nerve blocks are necessary for the MCP joints. Reduction with
splinting is the treatment of choice. Reduction is accomplished via
hyperextension of the joint with concurrent application of horizontal
traction. Flexion at the MCP joint will facilitate reduction of distal
joints. Postreduction radiographs are necessary to ensure adequate
reduction. The DIP joint should be splinted in slight flexion and the PIP
joint in 20 degrees of flexion for 3 to 5 weeks, depending on the degree
of ligamentous damage. Hand specialist follow-up is mandatory.
Clinical Pearls
1. All joints should be tested
for instability after reduction, using a digital nerve block to
facilitate testing.
2. PIP joint volar dislocation
can be unstable, requiring open reduction and internal fixation.
3. Joint dislocations that have
volar plate entrapment may be impossible to reduce and require surgical
repair for successful reduction.
|
|
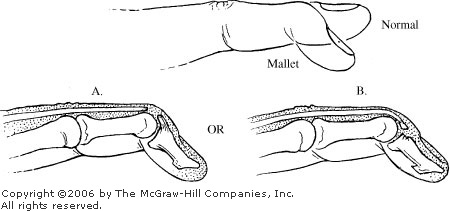
Mallet Finger
Associated Clinical Features
Mallet finger commonly occurs
after the distal finger, specifically the distal interphalangeal (DIP)
joint, is forcibly flexed, as from a sudden blow to the tip of the
extended finger. This injury represents complete avulsion or laxity of
the extensor tendon from the proximal dorsum of the distal phalanx (Fig.
11.42). The patient presents with an inability to extend the distal
phalanx, and it remains in a flexed position (Fig. 11.43). On radiograph,
a small chip fragment on the dorsum at the DIP joint may be visualized.
|
|
|

|
|
Mallet
Finger This photograph depicts
a mallet finger. The distal phalanx is held in flexion and the
patient is unable to extend it. (Courtesy of Kevin J. Knoop, MD, MS.)
|
|
|
|
|
|
|
Mallet
Finger This illustration
demonstrates that the unopposed flexion of the DIP joint is secondary
to the complete tear of the tendon (A), or an avulsion of a small
chip fragment (B).
|
|
Differential Diagnosis
Intraarticular fracture of the
distal phalanx, distal tuft fracture, or extensor tendon laceration can
be confused with a mallet finger.
Emergency Department Treatment
and Disposition
A closed mallet finger without
involvement of the joint can be treated by splinting the DIP joint in
extension to mild hyperextension. True hyperextension is to be avoided.
This splint should be worn for 6 to 8 weeks, at which point active range
of motion begins. There is no need to splint the other joints. Motion of
the PIP joint should not be blocked with the splint. Hand surgery
follow-up is required.
Clinical Pearls
1. During follow-up, some
patients exhibit hyperextension of the distal phalanx while out of the
splint. This is due to a weakness in the volar plate. These patients
should be splinted with the DIP joint in flexion and followed closely.
2. Avulsion of a significant
portion of the articular surface (more than one-third) may require open
reduction with internal fixation by a hand surgeon.
|
|
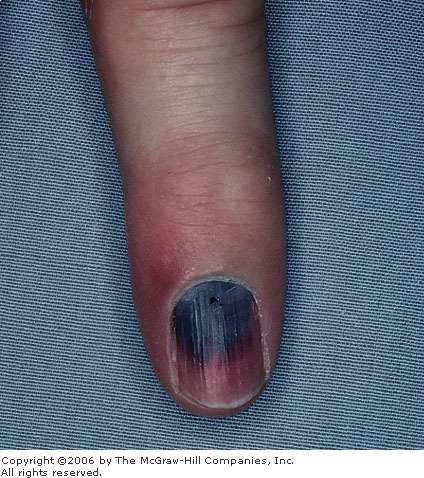
Subungual Hematoma
Associated Clinical Features
A subungual hematoma is a
collection of blood found underneath the nail, usually occurring
secondary to trauma to the distal fingers (Fig. 11.44). These lesions can
be quite painful because of pressure beneath the nail. There can also be
swelling, tenderness, and a decreased range of motion of the associated
finger. Associated injuries include nail bed trauma (Fig. 11.45) and
distal tuft fractures.
|
|
|
|
|
Subungual
Hematoma This subungual
hematoma occurred after the patient hit his finger with a hammer. The
hematoma covers approximately 50% of the subungual area. (Courtesy of
Margaret P. Mueller, MD.)
|
|
|
|
|

|
|
Nail
Bed Laceration Bleeding from a
nail bed laceration causes a subungual hematoma. This image depicts a
nail bed laceration seen after removal of the nail. (Courtesy of Alan
B. Storrow, MD.)
|
|
Differential Diagnosis
A nail bed melanoma may resemble
a subungual hematoma and is differentiated from a hematoma by lack of a
history of recent trauma and subsequent appearance of the
"lesion."
Emergency Department Treatment
and Disposition
A radiograph should be done to
evaluate for possible fracture. If the subungual hematoma covers less
than 25%, trephining the nail with a sterile needle or electrocautery is
adequate to relieve pain by allowing drainage. Management of larger
hematomas is somewhat controversial. Some authors advocate removal of the
nail if the hematoma covers more than 50% of the nail or there is an
associated fracture. A more recent conservative approach states that
removal of the nail is best reserved for those injuries that damage the
nail plate and surrounding tissues, regardless of the size of the
hematoma or presence of a tuft fracture. In many cases, trephination of
the nail is sufficient to relieve pain.
Clinical Pearls
1. Subungual hematomas are a
sign of nail bed injury.
2. Subungual hematomas with
surrounding nail bed and nail fold injuries require nail removal and evaluation
of the nail bed for injury and careful repair if needed.
3. A hand-held,
high-temperature, portable cautery device is a good tool for drainage of
a subungual hematoma.
|
|
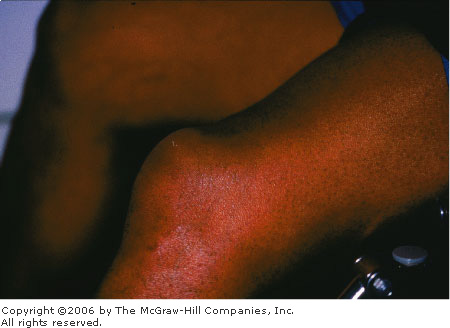
Compartment Syndrome
Associated Clinical Features
Compartment syndrome develops
when the pressure in a closed or inelastic fascial space increases to a
point where it causes compression and dysfunction of vascular and neural
structures. The five "Ps" that characterize compartment
syndrome are pain, pallor, paresthesias, increased pressure, and
pulselessness.
The earliest symptom is severe
pain out of proportion to the physical findings. The pain is worsened
with passive stretching of muscle within the compartment.
Anesthesia-paresthesia is an early sign of nerve compromise. Motor weakness
and pulselessness are late signs. Causes include compression, exercise,
circumferential burns, frostbite, constrictive dressings, arterial
bleeding, soft tissue injury, and fracture. Locations where compartment
syndrome can occur include the interossei of the hand, volar and dorsal
compartments of the forearm (Fig. 11.46), the gluteus medius, and
anterior, peroneal, and deep posterior compartments of the leg (Fig.
11.47). A creatine phosphokinase (CPK) of 1000 to 5000 U/mL may add to
suspicion of the diagnosis. Myonecrosis (Fig. 11.48) can cause
myoglobinuria and renal failure.
|
|
|

|
|
Compartment
Syndrome A swollen and tense
right forearm typical for the presentation of compartment syndrome.
(Courtesy of Lawrence B. Stack, MD.)
|
|
|
|
|

|
|
Compartment
Syndrome Anterior compartment
syndrome of the left leg is manifested by anterior tibial pain, tense
"woody" swelling, and erythema. Early in the course,
passive plantarflexion may cause referred pain to the compartment.
Later, the patient may develop foot drop. (Courtesy of Timothy
Coakley, MD.)
|
|
|
|
|

|
|
Compartment
Syndrome, Late Sequelae Muscle
necrosis may result from compartment syndrome, as seen in this
patient, who has undergone fasciotomy. (Courtesy of Kevin J. Knoop,
MD, MS.)
|
|
Differential Diagnosis
Soft tissue swelling, deep venous
thrombosis (DVT), neuropraxia, cellulitis, arterial intimal damage,
snakebite, inflammation, or hematoma formation can be mistaken for a
compartment syndrome.
Emergency Department Treatment
and Disposition
The initial treatment is removal
of any constrictive dressing and frequent evaluation. If there is no
improvement or there are no constrictive dressings in place,
decompression via a fasciotomy should be considered. Intracompartmental
pressure monitoring (Fig. 11.49) should be performed to assess the need
for immediate decompression. Pressures greater than 30 mmHg with signs
and symptoms are suggestive of compartment syndrome, whereas pressures
greater than 40 are diagnostic.
|
|
|

|
|
Compartment
Pressures Intracompartmental
pressure monitoring can be accomplished with commercially available
devices. Normal tissue pressures should be less than 10 mmHg.
(Courtesy of Selim Suner, MD, MS.)
|
|
Clinical Pearls
1. The diagnosis of compartment
syndrome should be made early and be based on clinical evaluation and the
mechanism of injury. Crush or compression injuries should heighten
suspicion.
2. The most common areas of the
extremities affected by compartment syndrome are the anterior compartment
of the lower leg due to proximal tibial fractures and the volar
compartment of the forearm secondary to fracture of the ulna or radius
and supracondylar fracture.
3. If a compartment syndrome is
suspected, the compartment pressure should be measured.
|
|
Hip Dislocations
Associated Clinical Features
Hip dislocations can be anterior,
posterior, or central. Posterior hip dislocations are the most common,
resulting from forces exerted on a flexed knee (e.g., a passenger in a
motor vehicle accident whose knees hit the dashboard). The extremity is
found shortened, internally rotated, and adducted (Fig. 11.50).
Associated fractures occur commonly. Anterior hip dislocations occur when
there is forced abduction to the femoral head, which forces the head out
through a tear in the anterior capsule. Anterior dislocations can be
superior (pubic) or inferior (obturator). The leg is abducted, externally
rotated, and flexed with an inferior anterior hip dislocation. A
superoanterior hip dislocation has the leg positioned in extension,
slight abduction, and external rotation. Patients complain of severe hip
pain and decreased range of motion.
|
|
|

|
|

|
|
Hip
Dislocation Typical clinical
appearance and patient position of a left posterior hip dislocation.
Note internal rotation of the affected extremity (A). Radiograph of
patient (B). (Courtesy of Cathleen M. Vossler, MD.)
|
|
Differential Diagnosis
Fractures of the femoral head,
pelvis, femoral neck, acetabulum, and femoral shaft are sometimes mistaken
for hip dislocations on initial examination.
Emergency Department Treatment
and Disposition
Treatment for dislocations is
early closed reduction using sedation, analgesia, and muscle relaxants.
Anterior dislocations are reduced using strong in-line traction with the
hip flexed and internally rotated, followed by abduction. Posterior
dislocations are reduced using in-line traction with the hip flexed to 90
degrees, followed by gentle internal to external rotation. A
neurovascular examination and radiographic evaluation should occur before
and after any attempts at reduction. Orthopedic consultation should be
obtained as early as possible. These patients require admission, with
frequent neurovascular evaluation.
Clinical Pearls
1. Complications of posterior
hip dislocations include sciatic nerve injury and avascular necrosis.
2. Immediate reduction is
imperative. The longer the delay in reduction, the greater the incidence
of avascular necrosis.
3. Patients with prosthetic
joints are at greater risk for dislocation, which can occur after only
slight trauma.
|
|
Hip Fracture
Associated Clinical Features
Fractures of the femoral head and
femoral neck and intertrochanteric fractures are termed hip fractures.
For classification, hip fractures are generally divided into
intracapsular (femoral head and neck fractures) and extracapsular
(trochanteric, intertrochanteric, and subtrochanteric fractures) (Fig.
11.51). Accurate classification is important because of the different
prognosis associated with each group. Intracapsular fractures are more
likely to be associated with disruption of the vascular supply and
resultant avascular necrosis. On the other hand, extracapsular fractures
rarely impair the vascular supply.
|
|
|
|
|
Hip
Fractures This illustration
depicts the different types of proximal femoral fractures.
|
|
All patients have complete immobility at the hip
joint. Complaints include hip and groin pain, tenderness, and an
inability to walk or place pressure on the affected side. There is
shortening of the affected leg as well as abduction and external rotation
(Fig. 11.52). Intertrochanteric fractures are associated with significant
pain, a shortened extremity, marked external rotation, swelling, and
ecchymosis around the hip (Fig. 11.53). Fractures of the femoral neck are
suggested when the extremity is held in slight external rotation,
abduction, and shortening. Dislocation of the hip is commonly associated
with femoral head fractures. Patients with anterior dislocation and a
femoral head fracture hold the lower extremity in abduction and external
rotation. Patients with a posterior dislocation hold the extremity in
adduction and internal rotation and display notable shortening.
|
|
|

|
|
Hip
Fracture Patients with hip
fractures often present with the affected extremity shortened,
externally rotated, and abducted. Note the rotation and shortening in
this patient with a right intertrochanteric fracture. (Courtesy of
Cathleen M. Vossler, MD.)
|
|
|
|
|

|
|
Hip
Fracture Radiographic
examination reveals an intertrochanteric fracture. (Courtesy of
Cathleen M. Vossler, MD.)
|
|
The femoral head has a tenuous
vascular supply which includes three sources: the artery of the
ligamentum teres, the metaphyseal arteries, and the capsular vessels. Any
injury that disturbs the anatomy of the hip can lead to compromise of
this vascular supply.
Shenton's line and the normal
neck shaft angle of 120 to 130 degrees (obtained by measuring the angle
of the intersection of lines drawn down the axis of the femoral shaft and
the femoral neck) should be checked in all suspicious injuries.
Differential Diagnosis
Pelvic fracture, femoral shaft
fracture, stress fracture, and hip dislocation are sometimes mistaken for
a hip fracture prior to radiographic examination.
Emergency Department Treatment
and Disposition
Once the patient is stabilized,
the hip fracture is reduced via traction. Femoral head
fracture-dislocations are an orthopedic emergency and require immediate
reduction. A neurovascular examination should be carefully performed
before and after any reduction attempts. Orthopedic consultation should
be obtained early, since these patients will require admission and in
most cases surgical reduction and fixation.
Clinical Pearls
1. Hip pain can be referred to
other areas. Therefore, in any patient complaining of knee or thigh pain,
consider the possibility of a hip fracture.
2. Fracture-dislocation of the
femoral head requires great forces, and associated injuries such as
chest, intraabdominal, and retroperitoneal injuries should be considered.
3. Intracapsular fractures
usually have much less blood loss than extracapsular fractures because of
hematoma containment within the capsule.
4. Fractures of the hip may be
diagnosed by auscultation of differences in bone conduction between the
patient's two extremities. This is performed by placing the stethoscope's
diaphragm on the anterosuperior iliac spine and giving the patella
several soft taps.
5. In the elderly, hip
fractures are usually secondary to a fall. Be sure to address the cause
of the fall to rule out a pathologic etiology (i.e., acute myocardial
infarction, syncope, etc.).
|
|
Pelvic Fracture
Associated Clinical Features
Pelvic fractures range in
severity from stable pubic rami fractures to unstable fractures with
hemorrhagic shock. Pain is the most frequently encountered complaint.
Blood at the urethral meatus, a high-riding prostate, gross hematuria, or
a scrotal hematoma (Fig. 11.54) are all signs of associated urinary tract
injury. Ecchymosis of the anterior abdominal wall, flank, sacral, or
gluteal region should be regarded as a sign of serious hemorrhage. Blood
found during rectal examination may indicate puncture of the wall of the
rectum from a pelvic fracture. Leg shortening may also be seen. A careful
neurologic examination is necessary, since there may be compromise of the
sciatic, femoral, obturator, or pudendal nerves.
|
|
|

|
|
Pelvic
Fracture Pelvic fractures may
require emergent external fixation to help control hemorrhage.
Scrotal hematoma, or Destot's sign, suggests a pelvic fracture.
(Courtesy of Cathleen M. Vossler, MD.)
|
|
Differential Diagnosis
Femoral fracture, hip fracture,
or intraabdominal or retroperitoneal pathology (including hemorrhage,
perforated viscus) can be confused with pelvic fractures.
Emergency Department Treatment
and Disposition
Management includes initial
stabilization and evaluation for any life-threatening injuries. Patients
may require multiple large-bore IVs and type and crossmatch with blood
readily available. Hemorrhagic shock occurs secondary to bleeding from a
pelvic fracture and is the major cause of death in these patients.
Retroperitoneal bleeding is unavoidable and up to 6 L of blood can easily
be lost. Early orthopedic consultation is critical for emergent external
fixation. Angiography should be performed to control small bleeding sites
if there is continued exsanguination.
Clinical Pearls
1. MAST (medical antishock
trousers) may be used to temporarily stabilize pelvic fractures.
2. Don't assume that a pelvic
fracture is the sole cause of hemorrhagic shock in a patient. Look for
other sources.
3. Posterior pelvic fractures
are more likely to result in hemorrhage and neurovascular damage.
Anterior pelvic fractures are more likely to cause urogenital damage.
4. Urinary tract injury is
highly associated with pelvic fracture and must be ruled out. If there
are any signs of genitourinary injury, a Foley catheter should not be
placed until a retrograde urethrogram has been performed.
5. Displacement of pelvic ring
fractures is usually associated with fracture or dislocation of another
ring element (Fig. 11.55).
|
|
|

|
|
Pelvic
Fracture Radiographic
examination reveals bilateral sacroiliac joint diastasis, complete
transverse fracture of the sacrum, and comminuted fractures of the
right superior and inferior pubic rami. (Courtesy of Cathleen M.
Vossler, MD.)
|
|
|
|
Femur Fracture
Associated Clinical Features
Femoral fractures occur secondary
to great forces, like those associated with motor vehicle accidents. The
diagnosis is usually evident on visualization of the thigh (Fig. 11.56)
and confirmed radiographically (Fig. 11.57). The position of the leg can
help determine at which point the femur is fractured. Commonly associated
injuries include hip fracture and dislocation as well as ligamentous
injury to the knee. Hematoma formation is common.
|
|
|

|
|
Femur
Fracture A closed midshaft
femoral fracture. Note the deformity in the middle of the thigh,
consistent with this injury. (Courtesy of Daniel L. Savitt, MD.)
|
|
|
|
|

|
|
Femur
Fracture Radiographic
examination reveals a comminuted displaced distal femoral fracture.
(Courtesy of Cathleen M. Vossler, MD.)
|
|
Differential Diagnosis
Pelvic fracture, hematoma, hip
fracture, hip dislocation, and contusion can be mistaken for femoral
fracture prior to radiographic examination.
Emergency Department Treatment
and Disposition
Initial management includes
stabilization and evaluation for any life-threatening injuries. It is
important to keep in mind that a large amount of blood loss can occur
(average blood loss for a femoral shaft fracture is 1000 mL). These
patients should have two large-bore intravenous lines and be crossmatched
for blood products should they become necessary. The extremity should be
immobilized and splinted with a traction device such as a Hare splint.
Once this is accomplished, radiographic evaluation of the extremity
should be performed. Orthopedic consultation should be obtained and
admission arranged. The majority of intertrochanteric and subtrochanteric
fractures require operative fixation and stabilization. An open fracture
is an orthopedic emergency; these patients require tetanus prophylaxis,
antibiotic coverage, and emergent irrigation and debridement in the
operating room.
Clinical Pearls
1. Pain can be referred. Any
injury between the lumbosacral spine and the knee can be referred to the thigh
or knee.
2. Vascular compromise can
occur and should be suspected with an expanding hematoma, absent or
diminished pulses, or progressive neurologic signs. Neurovascular status
needs to be assessed frequently.
3. Femoral shaft fractures can
mask the clinical findings of a hip dislocation; thus radiographs of the
pelvis and hips should be obtained routinely.
|
|
Knee Extensor Injuries
Associated Clinical Features
The quadriceps and its associated
tendons predominantly extend the knee. This mechanism may be disrupted by
quadriceps or patellar tendon rupture or patellar fracture. Collagen
disorders, degenerative disease, tendon calcifications, and fatty tendon
degeneration may predispose to these problems.
Quadriceps tendon ruptures are
more common than patellar tendon ruptures and are more often seen in the
elderly. Forced flexion during quadriceps contraction (as in a fall from
a curb) may cause sudden buckling and pain. The patella is inferiorly
displaced with proximal ecchymosis and swelling. A soft tissue defect at
the distal aspect of the quadriceps may be apparent on examination (Fig.
11.58). Proximal displacement of the patella with inferior pole
tenderness and swelling suggest a patellar tendon rupture (Fig. 11.59).
Lateral radiographs help distinguish between the two (Fig. 11.60).
|
|
|
|
|
Quadriceps
Tendon Rupture Inferior
displacement of the patella and a distal quadriceps defect suggest
quadriceps tendon rupture. (Courtesy of Robert Trieff, MD.)
|
|
|
|
|

|
|
Patellar
Tendon Rupture Proximal
displacement of the patella and inferior pole tenderness may be
subtle, as in this patient with left patellar tendon rupture.
(Courtesy of Kevin J. Knoop, MD, MS.)
|
|
|
|
|

|
|
Patellar
Tendon Rupture A lateral
radiograph of the patient in Fig. 11.59 reveals the proximal patellar
displacement seen with complete patellar tendon rupture. (Courtesy of
Kevin J. Knoop, MD, MS.)
|
|
Patellar fractures may be
transverse, stellate, or vertical. They may be caused by direct trauma or
through avulsion secondary to the quadriceps pull against resistance.
Tenderness, swelling, and sometimes a palpable defect are present.
Differential Diagnosis
Knee dislocation, patellar
contusion, or proximal femoral fracture may be confused with knee
extensor mechanism injuries.
Emergency Department Treatment
and Disposition
An optimal outcome for quadriceps
or patellar tendon rupture is realized with early consultation,
immobilization, and consideration of operative repair. There are
nonsurgical advocates who recommend conservative treatment.
Nondisplaced transverse patellar
fractures should be treated with long-leg splinting in full extension and
referral to orthopedics. Patients with displaced patellar fractures
generally receive operative treatment or excision of the patella.
Clinical Pearls
1. Patients with complete
ruptures have loss of active extension of the knee.
2. Avulsion of the tibial
tuberosity may also show a hide-riding patella on physical and
radiographic examination.
3. Magnetic resonance imaging
may distinguish partial from complete tears.
4. Patellar fractures may be
complicated by future degenerative arthritis or focal avascular necrosis.
|
|
Patellar Dislocations
Associated Clinical Features
Patellar dislocations result from
direct trauma to the patella. A force is applied to the upper portion of
the patella at the same time as a rotational force affects the knee. The
most common dislocations are lateral, but horizontal, superior, and
intercondylar dislocations also occur. These tend to be recurrent owing
to the resultant increased laxity of the supporting structures. Patients
who have had recurrent dislocations often reduce the dislocation prior to
arrival at the ED. Common complaints include pain, swelling, and a
deformity in the knee. Physical examination reveals fullness or deformity
in the lateral aspect of the knee (Fig. 11.61). Fractures of the patella
or femoral condyle occur in 5% of patients.
|
|
|

|
|
Patellar
Dislocation This photograph
depicts a lateral patellar dislocation of the right knee. Note the
obvious lateral deformity of the right patella. (Courtesy of Cathleen
M. Vossler, MD.)
|
|
Differential Diagnosis
Distal femoral fracture,
quadriceps rupture, patellar tendon rupture, patellar fracture, or knee
dislocation can be mistaken for a patellar dislocation.
Emergency Department Treatment
and Disposition
Reduction is easily accomplished
and results in immediate relief of pain. Lateral dislocations are reduced
by flexing the hip, extending the knee, and gently directing pressure
medially on the patella. Other dislocations generally require open
reduction. Radiographic examination should be obtained to document
patellar position as well as evaluate for fracture. These patients
require a knee immobilizer or long leg cast in full extension for 4 to 6
weeks. Orthopedic consultation should be obtained, since these patients
require further evaluation.
Clinical Pearls
1. A dislocated patella may
reduce spontaneously prior to presentation and should be addressed as a
possibility in any patient who presents with knee pain. This may be
elucidated by inquiring about a knee deformity at the time of injury that
is no longer present.
2. Complications of patellar
dislocation include degenerative arthritis, recurrent dislocations, and
fractures.
3. The patellar apprehension
test should be performed on these patients: patients have the sensation
that the patella will dislocate when there is lateral pressure placed on
the patella, at which point they grab for their knee.
|
|
Knee Dislocation
Associated Clinical Features
The peak incidence of knee
dislocation is in the third decade of life. It is more common in males.
Knee dislocations are classified by the direction of tibial displacement
relative to the femur. They may be anterior (Fig. 11.62), posterior (Fig.
11.63), medial, lateral, or rotary. Anterior dislocations account for 50
to 60% of dislocations and usually occur after high-energy hyperextension
injuries. Two-thirds of all knee dislocations are secondary to motor
vehicle crashes, with the remainder from falls, from sports, and from
industrial injuries. Anterior dislocations are associated with a high
incidence of associated popliteal artery and peroneal nerve injuries. The
affected limb will have gross deformity around the knee with swelling and
immobility; peroneal nerve injury manifests itself with decreased
sensation at the first web space with impaired dorsiflexion of the foot.
Many of these dislocations will reduce spontaneously prior to arrival in
the ED.
|
|
|

|
|
Anterior
Knee Dislocation A radiograph
demonstrating anterior displacement of the tibia in relation to the
femur. (Courtesy of Selim Suner, MD, MS.)
|
|
|
|
|
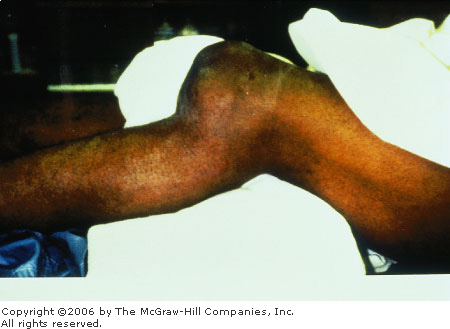
|
|
Posterior
Knee Dislocation A clinical
photograph demonstrating posterior displacement of the tibia in
relation to the femur. (Courtesy of Paul R. Sierzenski, MD.)
|
|
Differential Diagnosis
Tibia/fibular fractures, knee
fractures, femoral fractures, or patellar dislocation may mimic knee
dislocation.
Emergency Department Treatment
and Disposition
Emergent treatment includes early
reduction, immobilization, assessment of distal neurovascular function,
and emergent orthopedic referral. The knee should be evaluated for valgus
and varus stability at 20 degrees flexion. Reduction of anterior
dislocation is accomplished by having an assistant apply longitudinal
traction on the leg while keeping one hand on the tibia and
simultaneously lifting the femur anteriorly back into position. A
posterior splint with the knee in 15 degrees of flexion is used for immobilization
and to avoid tension on the popliteal artery. The patient should be
admitted for observation and arteriography. Historically, arteriography
was advocated for all anterior knee dislocations even with a normal
postreduction vascular examination; however, low-energy knee dislocations
with normal postreduction vascular examinations may not require
arteriography and can be followed by serial examination. Duplex Doppler
ultrasonography has been advocated by some authors and correlates well
with arteriography but may miss intimal tears.
Clinical Pearls
1. Knee dislocations are often
associated with a fracture of the proximal tibia.
2. The presence of distal
pulses in the foot does not rule out an arterial injury; there is a 10%
incidence of popliteal injury despite present distal pulses.
3. Vascular repair after 8 h of
injury carries an amputation rate of greater than 80%.
|
|
Tib-Fib Fractures
Associated Clinical Features
The tibia sustains a high
frequency of fractures secondary to direct trauma because of its
subcutaneous location. Tibial fractures may be complicated by nonunion,
neurovascular injury, or compartment syndrome. Suspect tibial fractures
with trauma to the lower extremity, pain, and inability to bear weight.
Tibial diaphyseal fractures carry a high risk for compartment syndrome,
and distal neurovascular status should always be documented.
Fibular fractures may be isolated
or be associated with injuries of the tibia (Fig. 11.64). Isolated
fibular fractures are caused by direct trauma to the lateral aspect of
the leg. Contrary to tibial fractures, complications of isolated fibular
fractures are rare. The fibula is a non-weight-bearing structure, so
isolated fractures are anatomically splinted by an intact tibia. Distal
fibular fractures may include a disrupted ankle joint, as evidenced by a
widened or nonuniform mortise on the AP radiograph.
|
|
|

|
|
Tib-Fib
Fracture Deformity associated
with a midshaft tibial and fibular fracture. (Courtesy of Kevin J.
Knoop, MD, MS.)
|
|
The Maisonneuve fracture is a
combination of an oblique proximal fibular fracture, disruption of the
interosseous membrane and tibiofibular ligament distally, and a medial
malleolar fracture or tear of the deltoid ligament. This fracture occurs
when an external rotational force is applied to the foot, producing a
fracture of the proximal third of the fibula. Physical examination
findings include tenderness at the anteromedial ankle joint capsule or at
the ankle syndesmosis in combination with proximal fibular tenderness.
Differential Diagnosis
Contusion, disseminated vascular
coagulation, compartment syndrome, and sprains must be considered.
Emergency Department Treatment
and Disposition
Treatment of tibial fractures
depends on whether they are open or closed and on the degree of
displacement. All open fractures require immediate orthopedic referral
for surgical treatment and reduction. Closed fractures that cannot be
reduced may also need open reduction. Patients with isolated nondisplaced
tibial fractures may be splinted, started on ice therapy, and referred
for outpatient treatment. Treatment of fibular fractures is dictated by
the degree of pain experienced by the patient and the involvement of the
ankle joint. Nondisplaced fractures can be treated with an air cast,
while those with displacement should be place in a sugar-tong splint and
referred for short-term orthopedic evaluation. Treatment of a Maisonneuve
fracture depends on the status of the ankle mortise. An intact mortise
with no joint space widening can be treated by casting. A mortise not in
anatomic alignment requires open reduction.
Clinical Pearls
1. Early follow up is required
for all tibial fractures owing to the risk of compartment syndrome.
2. The peroneal nerve crosses
over the head of the fibula and is subject to injury with a Maisonneuve
fracture.
3. Some patients with
Maisonneuve fracture may complain only of ankle pain. Maisonneuve
fracture represents about 1 in 20 ankle fractures, so always examine the
proximal fibula in patients complaining of ankle pain.
|
|
Fracture Blisters
Associated Clinical Features
Fracture blisters are vesicles or
bullae that arise secondary to swelling from soft tissue injury and
fracture formation (Fig. 11.65). The most commonly affected areas include
the tibia, ankle, and elbow. Patients note blister formation within 1 to
2 days after the initial trauma. Patients complain of pain, swelling, ecchymosis,
and decreased range of motion. Complications include infection, deep
venous thrombosis, and compartment syndrome.
|
|
|

|
|
Fracture
Blisters Fracture blisters in
a patient who fell down four steps on the evening prior to
presentation. The patient had initially complained of ankle pain,
decreased range of motion, and an inability to bear weight. Upon
awakening the next morning, he noted ecchymosis, swelling, and
blister formation. Radiographics revealed fracture of the fibula.
(Courtesy of Daniel L. Savitt, MD.)
|
|
Differential Diagnosis
Sprain, fracture, cellulitis,
necrotizing fasciitis, compartment syndrome, or burns can be mistaken for
fracture blisters.
Emergency Department Treatment
and Disposition
Blisters are generally left
intact, and the underlying fracture is treated.
Clinical Pearls
1. Blisters can be seen with
other conditions, including barbiturate overdose; in the setting of
trauma, however, they frequently indicate an underlying fracture.
2. Blisters are managed in a
similar fashion to second-degree burns.
|
|
Achilles Tendon Rupture
Associated Clinical Features
Rupture of the Achilles tendon
occurs most frequently in middle-aged males involved in athletic
activities. Three mechanisms result in this injury: a direct blow to the
tendon, forceful dorsiflexion of the ankle, or increased tension on an
already taut tendon. Rupture occurs 2 to 3 cm above the tendon's
attachment to the calcaneus (Fig. 11.66). Patients complain of a feeling
of being hit in the posterior aspect of the lower leg. They may hear or
feel a pop. There is weakness when pushing off of the foot; pain, edema,
and ecchymosis develop. Thompson's test can be diagnostic of an Achilles
rupture (Fig. 11.67). The patient should be placed in a prone position;
the gastrocnemius muscle should be grasped and squeezed. If the Achilles
tendon is even partially intact, then the foot will plantarflex; if ruptured,
there will be no movement of the foot.
|
|
|

|
|
Achilles
Tendon Rupture This photograph
depicts a patient with a right Achilles tendon rupture. Note the loss
of the normal resting plantarflexion on the right owing to disruption
of the tendon. This is seen with the patient in a nonweight-bearing
position. Swelling is also apparent over the site of the tendon injury.
(Courtesy of Kevin J. Knoop, MD, MS.)
|
|
|
|
|

|
|
Thompson's
Test This illustration
demonstrates the Thompson's test, where compression of the
gastrocnemius-soleus complex normally produces plantarflexion of the
foot (1). If the tendon is completely ruptured, this will not occur
(2).
|
|
Differential Diagnosis
Partial Achilles tendon tear,
plantaris tendon rupture, ankle sprain, Achilles tendinitis, and partial
gastrocnemius muscle rupture have been confused with an Achilles tendon
rupture.
Emergency Department Treatment
and Disposition
Treatment is either operative or
conservative. In either case, the extremity is immobilized without weight
bearing for 6 weeks, followed by 6 weeks of partial weight bearing. ED
treatment consists of elevation, analgesia, ice, and immobilization with
a posterior splint. Orthopedic consultation should be obtained so that a
plan of treatment can be chosen. These patients can be discharged home
with close orthopedic follow-up or can be admitted for acute repair.
Partial tears are generally treated conservatively.
Clinical Pearls
1. Advantages to surgical
repair are increased strength and mobility and a decreased rate of
rerupture.
2. Approximately 25% of these
injuries are initially misdiagnosed as ankle sprains.
3. These patients maintain the
ability to plantarflex the foot in a non-weight-bearing position owing to
the action of the tibialis posterior, toe flexor, and peroneal muscles.
4. Palpation of the tendon
alone may not detect rupture, as the tendon sheath is often intact.
|
|
Ankle Dislocation
Associated Clinical Features
Ankle dislocations require forces
of great magnitude. Posterior and lateral dislocations are the most
common, but the ankle can also dislocate medially, superiorly, or
anteriorly (Figs. 11.68, 11.69, 11.70). A posteriorly dislocated ankle is
locked in plantarflexion with the anterior tibia easily palpable. The
foot has a shortened appearance, with the ankle very edematous. Anterior
dislocations present with the foot dorsiflexed and elongated. Lateral
dislocations present with the entire foot displaced laterally. Ankle
dislocations are commonly associated with malleolar fractures.
|
|
|

|
|
Posterior
Ankle Dislocation A posterior
ankle dislocation is pictured. Radiographs showed an associated
fracture. (Courtesy of Mark Madenwald, MD.)
|
|
|
|
|
|
|
Ankle
Dislocations This illustration
depicts different types of ankle dislocations. Arrows denote
direction of the injury force. (Adapted with permission from Simon R:
Emergency Orthopedics: The Extremities. New York: Appleton
& Lange, 1987, p. 402.)
|
|
|
|
|

|
|
Lateral
Ankle Dislocation The foot is
laterally displaced in this patient with a lateral ankle dislocation.
A radiograph revealed fracture of the distal fibula. (Courtesy of
Cathleen M. Vossler, MD.)
|
|
Differential Diagnosis
Fractures of the tibia, fibula,
or talus, as well as ankle sprains, are all commonly mistaken for an
ankle dislocation on initial examination. A subtalar foot dislocation
(Fig. 11.71) resembles ankle dislocation.
|
|
|

|
|
Subtalar
Dislocation This patient
landed on his foot while playing basketball. Neurovascular status was
intact, and the ankle was promptly reduced after x-ray showed no
associated fracture. (Courtesy of Kevin J. Knoop, MD, MS.)
|
|
Emergency Department Treatment
and Disposition
Routine radiographs should be
obtained to identify any fractures. Reduction should occur before
radiography if circulatory compromise exists. To reduce the ankle, gentle
traction is applied to the foot, in an opposite direction of the force
that caused the injury. Neurovascular status should be checked before and
after any attempts at reduction or immobilization. Reduction usually
requires conscious sedation, a Bier block, or general anesthesia.
Patients should be placed in a posterior splint with immediate referral
to an orthopedic surgeon for hospitalization.
Clinical Pearls
1. These injuries are commonly
associated with malleolar fractures and often require open reduction and
internal fixation.
2. Fifty percent of ankle
dislocations are open and require surgical debridement.
3. There is an increased
incidence of avascular necrosis following ankle dislocation.
|
|
Calcaneus Fracture
Associated Clinical Features
The calcaneus is the most
frequently fractured tarsal bone. Injuries are associated with falls from
a height or twisting mechanisms. There are two types: intra- and extraarticular.
Intraarticular fractures generally result from an axial load. These
patients have severe heel pain in association with soft tissue swelling
and ecchymosis of the pericalcaneal tissues extending to the arch. Heel
contour can be distorted. Extraarticular fractures are less common and
may occur secondary to twisting or avulsive muscle forces. They are
divided anatomically into the following types: anterior process,
tuberosity (beak or avulsion), medial process, sustentaculum tali, and
body.
Differential Diagnosis
Lisfranc's fracture, midfoot or
forefoot fracture, and ankle sprain must be considered.
Emergency Department Treatment
and Disposition
Differentiate extraarticular (25
to 35%) fractures, which have a good prognosis, from intraarticular (70
to 75%) fractures. Oblique radiographs and computed tomography (CT) scans
can be used to rule out involvement of the subtalar joint. With
intraarticular fractures, a lateral foot radiograph reveals a reduction
in Bohler's angle (Figs. 11.72, 11.73), the posterior angle formed by
intersection of a line from posterior to middle facet and a line from
anterior to middle facet. Bohler's angle is normally between 28 and 40
degrees, with an average of 30 to 35. Angles of less than 28 degrees, or
more than 5 degrees less than the uninjured side, suggest a fracture.
Intraarticular fractures require urgent orthopedic consultation, since
open reduction and internal fixation are usually necessary.
|
|
|
|
|
Bohler's
Angle Bohler's angle is formed
by the intersection of lines drawn tangentially to the anterior (A)
and posterior (B) elements of the superior surface of the calcaneus
(C). A normal angle is between 28 and 40 degrees. Angles of less than
28 degrees are suggestive of a calcaneal fracture.
|
|
|
|
|

|
|
Calcaneal
Fracture This patient fell
from a ladder and struck his heel. A cortical step-off is seen on the
inferior aspect of the calcaneus. Bohler's angle has been calculated
at approximately 22 degrees. (Courtesy of Alan B. Storrow, MD.)
|
|
Nondisplaced extraarticular
fractures not involving the subtalar joint generally heal well with bulky
compressive dressings, rest, ice, elevation, and non-weight bearing for
the first 6 weeks. However, some may require open reduction; therefore
orthopedic referral is necessary.
Clinical Pearls
1. Calcaneal fracture warrants
a diligent search for associated injuries. 20% of calcaneal fractures are
associated with spinal fractures, 7% have contralateral calcaneal
fractures, and 10% are associated with compartment syndromes. The
subtalar joint is disrupted in 50% of cases. A high index of suspicion
for thoracic aortic rupture and renal vascular pedicle disruption must be
maintained when calcaneal fractures are seen.
2. Minimally displaced
fractures of the anterior process are easily missed and should be
suspected in a patient who does not recover appropriately from a lateral
ankle sprain. If the fragment is small or diagnosis is delayed, this
fragment can simply be excised.
3. CT scanning is the optimal
imaging technique.
|
|
Ankle Sprain
Associated Clinical Features
Ankle sprains are extremely
common problems in the ED. Classification of these injuries based on
physical examination and radiography helps guide management and
definitive treatment.
The most common mechanism is an
inversion stress that injures, in order, the joint capsule, anterior
talofibular ligament, calcaneofibular ligament, and posterior talofibular
ligament. Since the medial deltoid ligament is quite strong and elastic,
serious eversion injuries usually result in avulsion of the medial
malleolus or fracture of the lateral malleolus.
A first-degree sprain is defined
by a stretch injury, or microscopic damage, to ligaments resulting in
pain, tenderness, minimal swelling, and maintenance of the ability to
bear weight. A second-degree sprain is defined by a partial tear of the
ligamentous structures resulting in pain, swelling (Fig. 11.74), local
hemorrhage (Fig. 11.75), and moderate degree of functional loss. A
third-degree sprain is a complete tear of the ligament or ligaments and
presents with positive stress testing, significant swelling, and an
inability to bear weight.
|
|
|

|
|
Ankle
Sprain Comparison view of a
patient with a second-degree left lateral ankle sprain. Note the
swelling and asymmetry of the affected area. (Courtesy of Kevin J.
Knoop, MD, MS.)
|
|
|
|
|

|
|
Ankle
Sprain Note the dependent
ecchymosis and swelling in this patient with a second-degree left
lateral ankle sprain. (Courtesy of Lawrence B. Stack, MD.)
|
|
Differential Diagnosis
Malleolar and fifth metatarsal
fractures can be confused with ankle sprains prior to radiographs. Any
patient with joint pain should have an infectious etiology considered.
Emergency Department Treatment
and Disposition
First-degree injuries are treated
with ice packs, elevation, woven elastic (Ace) wrap, and early
mobilization. For patients with mild second-degree sprains,
immobilization for 72 h followed by use of an ankle support has been
advocated. More serious second-degree and all third-degree sprains should
receive immobilization, ice, and elevation and be referred to
orthopedics. In younger patients, surgery is an option, although clear
recommendations are lacking.
Clinical Pearls
1. Ankle injuries are the most
common orthopedic problem in emergency medicine.
2. Complications of ankle
sprains include instability, persistent pain, recurrent sprains, and
peroneal tendon dislocation.
3. Published guidelines known
as the Ottawa Ankle Rules were designed to limit unnecessary radiographs
by clinical scoring.
4. The most common eversion
injury is a fracture of the lateral malleolus. Since inversion injuries
also produce lateral problems, the most common injuries to the ankle
involve the lateral side.
5. Both malleoli, the proximal
fibula, and the fifth metatarsal should be examined for injury in
evaluating a patient with an ankle sprain.
|
|
Fractures of the Fifth Metatarsal Base
Associated Clinical Features
Patients complain of pain,
swelling, decreased range of motion, and tenderness over the lateral
aspect of the foot (Fig. 11.76). Fractures of the fifth metatarsal base
have been generically referred to as Jones fractures. However, the
fractures can be divided into three types, depending on their anatomic
location. Treatment is determined by this division.
|
|
|

|
|
Jones
Fracture This patient
sustained an injury of the fifth metatarsal and presented with pain
and swelling over this site. His radiograph revealed a fracture.
(Courtesy of Cathleen M. Vossler, MD.)
|
|
The classic Jones fracture is a transverse fracture
of the fifth metatarsal diaphysis (Figs. 11.77, 11.78). It occurs when a
force is applied to a plantarflexed and inverted foot. It is also
referred to as a stress fracture of the proximal shaft and is usually due
to repetitive stress injury. Patients often have prodromal symptoms.
|
|
|
|
|
Fifth
Metatarsal Base Fractures This
illustration depicts an avulsion fracture (A) and a classic Jones
fracture (B).
|
|
|
|
|

|
|
Jones
Fracture Radiograph with
typical appearance for a diaphyseal fracture of the fifth metatarsal
base. (Courtesy of Alan B. Storrow, MD.)
|
|
A fracture at the metaphyseal–diaphyseal
junction has been termed a pseudo-Jones fracture. It is always an acute
injury.
The last type is an avulsion
fracture of the fifth metatarsal base caused by sudden inversion of the
foot (Figs. 11.77, 11.79). The avulsion injury is caused by traction on
the lateral cord of the plantar aponeurosis.
|
|
|

|
|
Fifth
Metatarsal Avulsion Fracture
Radiograph illustrating an avulsion-type fracture of the fifth
metatarsal base, sometimes referred to as a ballet dancer's fracture
(see Fig. 11.77). (Courtesy of Alan B. Storrow, MD.)
|
|
Differential Diagnosis
Care must be taken to avoid
confusing the two sesamoid bones in this area with a fracture. The more
common of the two, the os peroneum (present in approximately 15%), lies
within the peroneus longus tendon. More rare is the os vesalianum, which
lies in the peroneus brevis tendon. Both have smooth, rounded surfaces
and usually occur bilaterally. The apophysis of the fifth metatarsal base
can also be mistaken for a fracture. It usually fuses by 16 years of age,
although some fail to fuse.
Other entities to consider
include ankle sprain, other metatarsal fractures, and foot dislocations.
Emergency Department Treatment
and Disposition
A Jones fracture should be
splinted and referred to orthopedics for definitive repair. It may heal
slowly and cause permanent pain and disability. Surgical treatment is
sometimes recommended, particularly since the stress involved with these
fractures usually occurs in the sporting activities of young patients.
A pseudo-Jones fracture usually
heals without complication, although more slowly than the avulsion
fracture. Referral to orthopedics for a walking or non-weight-bearing
cast, according to local preference, is indicated.
The avulsion fracture usually
heals rapidly and seldom leads to permanent disability. Most orthopedic
physicians treat these patients symptomatically with a short leg walking
cast or hard-sole shoe for 2 to 3 weeks. Surgery is rarely indicated.
Clinical Pearls
1. It is important to
differentiate between the different types of fractures of the fifth
metatarsal base; treatment and disposition are dictated by these
categories.
2. The original description of
these fractures was by Sir Robert Jones, who personally sustained an
injury while dancing. The avulsion fracture is sometimes referred to as
the ballet dancer's fracture.
3. The classic Jones fracture
has a high incidence of delayed healing and nonunion.
|
|
Lisfranc's Fracture-Dislocation
Associated Clinical Features
This is the most commonly
misdiagnosed foot injury. The Lisfranc joint (tarsometatarsal joint)
connects the midfoot and forefoot. It is defined by the articulation of
the bases of the first three metatarsals with the cuneiforms and the
fourth and fifth metatarsals with the cuboid. Lisfranc's ligament anchors
the second metatarsal base to the medial cuneiform. Although disruption
of the Lisfranc joint is typically associated with high-energy
mechanisms—such as falls, vehicle crashes, and direct crush
injuries—they also occur with lower-intensity mechanisms. Although
the clinical presentation is variable, severe midfoot pain and the inability
to bear weight are usually present (Fig. 11.80). Radiographs may reveal
displacement of the metatarsals in one direction (homolateral) or a
split, usually between the first and second metatarsals (divergent)
(Figs. 11.81, 11.82).
|
|
|
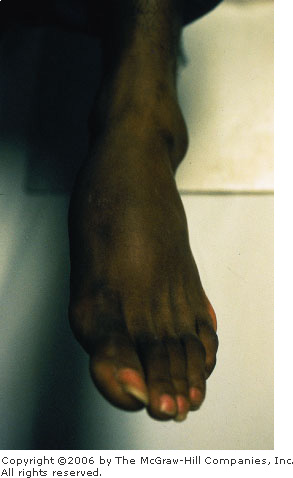
|
|
Lisfranc
Fracture-Dislocation This
patient presented with extreme midfoot pain and swelling. (Courtesy
of Kevin J. Knoop, MD, MS.)
|
|
|
|
|
|
|
Lisfranc
Fracture-Dislocations
Homolateral (left) and divergent (right) Lisfranc
fracture-dislocations.
|
|
|
|
|

|
|
Lisfranc
Fracture-Dislocation A
divergent Lisfranc fracture-dislocation. Note the disruption of the
alignment of the second metatarsal and the middle cuneiform.
Sometimes these injuries are not as apparent and comparison
radiographs are necessary. (Courtesy of Alan B. Storrow, MD.)
|
|
Differential Diagnosis
Metatarsal fracture, navicular
fracture, and contusion should be considered.
Emergency Department Treatment
and Disposition
Meticulous evaluation of foot
radiographs is key to diagnosis. The medial aspect of the first three
metatarsals should align with the medial borders of the first three
cuneiforms. The metatarsals should be aligned dorsally with their
respective tarsal bones on the lateral view. The medial aspect of the
fourth metatarsal should align with the medial cuboid. A disruption of
these anatomic relationships is suggestive of a Lisfranc injury. Also
suggestive are fractures or dislocations of the cuneiform or navicular
and widening of the spaces between the first and second and second and
third metatarsals. Lisfranc injuries warrant orthopedic evaluation in the
ED. Closed reduction can be attempted using finger traps on the toes and
placing traction on the hindfoot. Postreduction displacement of more than
2 mm or a tarsometatarsal angle of greater than 15 degrees requires
surgical fixation. Tenderness over the Lisfranc complex with normal
radiographs can reflect a strain of the complex. Stress (weight-bearing)
radiographs may unmask joint instability. Lisfranc sprains should be
placed in a short-leg walking cast. Potential complications include
compartment syndrome, chronic pain, loss of the metatarsal arch, reflex
sympathetic dystrophy, and biomechanical difficulties.
Clinical Pearls
1. Early recognition of
Lisfranc fracture-dislocations is facilitated by assessing for the normal
bony alignment on x-ray and by searching for frequently associated
fractures.
2. Fractures of the second
metatarsal base are considered pathognomonic of a Lisfranc injury.
|
|
Electrical Injury
Associated Clinical Features
Electricity may cause harm by
heat generated through tissue resistance or directly by the current on
cells. Skin, nerves, vessels, and muscles usually sustain the greatest
damage. Many factors affect the severity of injury: type of current (DC
or AC), current intensity, contact duration, tissue resistance, and
current pathway through the body. Those at high risk for electrical
injury are toddlers, those who perform risk-taking behavior, and people
who work with electricity.
When electricity is deposited in
the tissues, it may cause a host of injuries: contact burns (entry and
exit—Fig. 11.83), thermal heating, arc burns, prolonged muscular
tetany, or blunt trauma. Sudden death (asystole, respiratory arrest,
ventricular fibrillation), myocardial damage, cerebral edema,
neuropathies, disseminated intravascular coagulation, myoglobinuria,
compartment syndrome, and various metabolic disorders have been
described.
|
|
|

|
|
Electrical
Injury This electrical worker
grabbed a high-voltage power line with his hand and sustained an
electrical injury. Exit wounds may occur where the patient is
grounded, often through the feet when standing. Since this is a
transthoracic injury, particular attention should be paid to cardiac
monitoring. (Courtesy of Alan B. Storrow, MD.)
|
|
High-voltage DC or AC current
typically causes a single violent muscular contraction that throws the
victim from the source. As a result, blunt trauma and blast injuries may
occur. Low-voltage AC currents (as from a household outlet) typically
cause muscular tetany, forcing the victim to continue contact with the
source.
Differential Diagnosis
Stroke, toxic ingestion,
envenomation, myocardial infarction, assault, and seizures may mimic
electrical injury.
Emergency Department Treatment
and Disposition
After initial stabilization,
consider cervical spine immobilization, oxygen administration, cardiac
monitoring, and intravenous crystalloid infusion. A Foley catheter will
help monitor urine output and is especially important if rhabdomyolysis
is suspected.
Diagnostic testing to consider
includes: ECG, CBC, urinalysis, CPK, CPK-MB, electrolytes, BUN,
creatinine, and coagulation profile. Radiographic assessment is important
for those with a suspicion of trauma.
Severe or high-risk injuries
should be admitted to a burn or trauma center with surgical consultation.
Patients with minor, brief, low-intensity exposures, with a normal ECG,
normal urinalysis, and no significant burns or trauma may be considered
for discharge after 6 to 8 h of observation.
Clinical Pearls
1. The low resistance of water
makes its association with electricity particularly dangerous.
2. High-risk features include
high-voltage exposure (>600 V), deep burns, neurologic injury,
dysrhythmias, an abnormal electrocardiogram, evidence of rhabdomyolysis,
suicidal intent, or significant associated trauma.
|
|