|
Note: Large images and
tables on this page may necessitate printing in landscape mode.
Copyright
©2006 The McGraw-Hill Companies. All rights reserved.
Emergency
Medicine Atlas > Part 1. Regional
Anatomy > Chapter 12. Extremity Conditions >
|
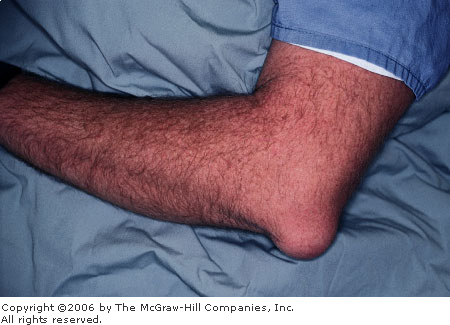
Cellulitis
Associated Clinical Features
Cellulitis is infection of the
skin or subcutaneous tissues from local invasion, traumatic wounds, or
hematogenous dissemination. The local inflammatory response is
characterized by erythema with poorly defined borders, edema, warmth,
pain, and limitation of movement (Fig. 12.1). Fever and constitutional
symptoms may be present and are commonly associated with bacteremia.
Trauma, lymphatic or venous stasis, immunodeficiency, and foreign bodies
are predisposing factors. There may be enlarged regional lymph nodes.
Organisms commonly causing cellulitis are group A beta hemolytic Streptococcus
and Staphylococcus aureus in nonintertriginous skin not associated
with an ulcer, gram-negative organisms in intertriginous skin and
ulcerations, and Haemophilus influenzae in children younger than 3
years. In immunocompromised hosts, Escherichia coli, Klebsiella
species, Enterobacter species, and Pseudomonas aeruginosa
may be the etiologic agents.
|
|
|

|
|
Cellulitis Cellulitis of the left leg characterized by
erythema and mild swelling. (Courtesy of Frank Birinyi, MD.)
|
|
Differential Diagnosis
Deep venous thrombosis of the
lower extremities, erythema nodosum, septic or inflammatory arthritis,
osteomyelitis, herpes zoster, allergic reactions, arthropod envenomation,
and burns are included in the differential diagnosis of cellulitis.
Emergency Department Treatment
and Disposition
Treatment of minor cases commonly
consists of immobilization, elevation, analgesia, and oral antibiotics
with reevaluation in 48 h. Admission and parenteral administration of
antibiotics may be necessary for immunocompromised or toxic-appearing
patients or those who do not initially respond to outpatient therapy.
Clinical Pearls
1. Aggressive treatment of
cellulitis with broad-spectrum parenteral antibiotics in
immunocompromised patients (e.g., diabetes mellitus) is warranted.
2. Fever is uncommon and often
associated with bacteremia.
3. Radiography for the presence
of foreign body or gas in the tissue should be considered.
4. Leading-edge aspirates are
of low yield but may be of help in a toxic-appearing patient.
5. The incidence of Haemophilus
influenzae cellulitis in children has decreased significantly with
HIB vaccination.
|
|
Felon
Associated Clinical Features
A felon is a pyogenic infection
of the distal pulp space often caused by staphylococci or streptococci. A
felon cannot decompress itself because the collection of pus is trapped
between septa that attach the skin to the distal phalanx. This condition
is characterized by severe pain, exquisite tenderness, and tense swelling
of the distal pulp with erythema (Fig. 12.2). There may be a visible
collection of pus or palpable fluctuance. Complications include deep
ischemic necrosis, osteomyelitis, septic arthritis, and septic
tenosynovitis.
|
|
|

|
|
Felon Note the area of purulence at the center of
the palmar pad in this thumb with a felon. There is also swelling and
erythema. (Courtesy of Daniel L. Savitt, MD.)
|
|
Differential Diagnosis
Hematoma following traumatic
injury, paronychia, and herpetic whitlow should be considered.
Emergency Department Treatment
and Disposition
Several incision and drainage
techniques are employed in the treatment of a felon, and there is
controversy surrounding which technique is the best to use. Incision and
drainage utilizing a midlateral approach along the nondominant side of
the finger or over the area of greatest fluctuance is commonly used to
drain a felon. An alternative technique is to make a longitudinal volar
incision directly through the finger pad into the pulp space and pus
collection. To ensure complete drainage of the abscess cavity, all
compartments should be entered. The packing of the abscess space is made
with a small, loose-fitting wick to facilitate drainage. Oral antibiotics
directed against gram-positive organisms should be used for 10 days and
the packing removed or replaced after 24 to 48 h.
Clinical Pearls
1. Do not extend the incision
proximal to the distal flexion crease.
2. Incisions should be made
dorsal to the neurovascular bundle; the pincer surfaces (radial aspects
of the index and long fingers and ulnar aspect of the thumb and small
finger) should be avoided when possible.
3. "Hockey stick" and
"fish mouth" incisions are associated with increased occurrence
of unnecessary sequelae and are not recommended.
4. If there is radiographic
evidence of osteomyelitis, bone debridement as well as antibiotic
coverage is required.
|
|
Dry Gangrene
Associated Clinical Features
Gangrene denotes tissue
that has lost its blood supply and is undergoing necrosis. The term dry
gangrene (Figs. 12.3, 12.4) is used for tissues undergoing sterile
ischemic coagulative necrosis, whereas wet gangrene is associated
with bacteria proteolytic decomposition. Streptococcus pyogenes is
often implicated in rapidly developing (6 h to 2 days) gangrene in
traumatic and surgical wounds. Clostridia, anaerobic streptococci, and
mixed aerobic and anaerobic flora can also be seen in wounds caused by
trauma, surgery, or diabetic ulcers.
|
|
|

|
|
Dry
Gangrene Dry gangrene of the
toes showing the areas of total tissue death, appearing as black and
lighter shades of discoloration of the skin demarcating areas of
impending gangrene. (Courtesy of Lawrence B. Stack, MD.)
|
|
|
|
|

|
|
Dry
Gangrene Dry gangrene of the
toes as a result of vascular disease. (Courtesy of Selim Suner, MD,
MS.)
|
|
Differential Diagnosis
Gas gangrene, frostbite,
cyanosis, traumatic ecchymosis, deep venous thrombosis (DVT), and
subungual hematoma are some conditions that should be included in the
differential diagnosis of gangrene.
Emergency Department Treatment
and Disposition
The treatment consists of
amputation, debridement, and antibiotic therapy as needed. Underlying
vascular pathology must be evaluated by arteriography and corrected
surgically. Hospitalization is usually required; patients who present
with systemic toxicity may require resuscitation in the ED.
Clinical Pearls
1. Obtain radiographs to help
rule out clostridial myonecrosis and osteomyelitis.
2. Soft-tissue infection may
complicate this condition.
|
|
Gas Gangrene (Myonecrosis)
Associated Clinical Features
Also called clostridial
myonecrosis, this infection causes rapid necrosis and liquefaction of
fascia, muscle, and tendon. The vast majority of cases involve Clostridium
perfringens, which produces a lethal necrotizing hemolytic alpha
exotoxin. Myonecrosis is classically associated with trauma and diabetes.
The inoculation of bacteria occurs either directly into the wound or by
hematogenous spread. There is edematous bronze or purple discoloration,
flaccid bullae with watery brown nonpurulent fluid (Fig. 12.5), and a
foul odor. The most important clinical presentation is pain due to edema
and the rapid production of gas in the infected tissue (Fig. 12.6). Pain
out of proportion to the appearance of the injury is classic. Low-grade
fever, which is an unreliable index of the severity of the infection, and
tachycardia out of proportion to the fever are often present.
|
|
|

|
|
Gas
Gangrene A gangrenous foot
with large bullae, areas of skin that are sloughing, and necrotic
skin. There is also significant swelling. (Courtesy of Selim Suner,
MD, MS.)
|
|
|
|
|

|
|
Gas
Gangrene Lateral view
radiograph of the foot seen in Fig. 12.5. In addition to the
swelling, there is air within the soft tissues, best seen in the
plantar portion of the foot. (Courtesy of Selim Suner, MD, MS.)
|
|
Crepitance and appearance of
gross pockets of air in the tissue may be appreciated but may not be
present early in the course of the illness. The incubation period for
clostridia ranges between 1 and 4 days, but it can be as early as 6 h.
Decreased tissue oxygen tension along with wound contamination are
required for the infection to progress. Factors favoring decreased tissue
oxygen tension include decreased blood supply, foreign body, tissue
necrosis, or wound bacteria, which consume oxygen.
Differential Diagnosis
Crepitant cellulitis, synergistic
necrotizing cellulitis, acute streptococcal hemolytic gangrene, and
streptococcal myositis are some conditions that may be mistaken for
clostridial myositis. Aspiration and Gram's stain showing gram-positive
rods and few leukocytes may help, but often surgical exploration of the
fascia and muscle is required to make the correct diagnosis.
Emergency Department Treatment
and Disposition
Aggressive resuscitation with
intravenous fluids is initiated, and consideration is given to packed red
blood cell transfusion. Broad-spectrum antibiotics in conjunction with
penicillin G, in the non-penicillin-allergic patient, is given in the ED.
Tetanus prophylaxis must not be overlooked. Surgical debridement or
amputation, the mainstays of therapy, must be initiated promptly.
Hyperbaric oxygen, in conjunction with surgical and antibiotic therapy,
has been suggested to have a synergistic effect in preventing the
progression of infection and production of toxin.
Clinical Pearls
1. Clostridial infection should
be considered in patients presenting with low-grade fever, tachycardia
out of proportion to the fever, and pain out of proportion to physical
findings.
2. Mortality is 80 to 90% if
untreated, 10 to 25% when treated appropriately.
3. Mixed gram-negative rods and
enterococci are found in nonclostridial gas gangrene, which is
exclusively seen in diabetics and carries a mortality of only 4% when
treated.
4. Gram's stain yielding
gram-positive bacilli with a relative lack of leukocytes can rapidly
confirm clinically suspected clostridial myonecrosis.
|
|
Necrotizing Fasciitis
Associated Clinical Features
This uncommon, severe infection
involves the subcutaneous soft tissues, including the superficial and
deep fascial layers, with early sparing of the skin and late involvement
of the muscle. It is most commonly seen in the lower extremities,
abdominal wall, perianal and groin area, and postoperative wounds but can
manifest in any body part. The infection is spread most commonly from a
site of trauma or surgical wound, abscess, decubitus ulcer, or intestinal
perforation. Alcohol, parenteral drug abuse, and diabetes mellitus are
predisposing factors. Omphalitis may progress to necrotizing fasciitis in
the newborn. Pain, tenderness, erythema, swelling, warmth, shiny skin,
lymphangitis, and lymphadenitis are early clinical findings. Later, there
is rapid progression with changes in skin color, formation of bullae with
clear pink or purple fluid (Fig. 12.7), and cutaneous necrosis (Fig.
12.8), within 48 h. The skin becomes anesthetic and subcutaneous gas may
be present. Systemic toxicity may be manifest by fever, dehydration,
leukocytosis, and frequently positive blood cultures. Fournier's gangrene
is a form of necrotizing fasciitis occurring in the groin and genitalia
(see Figs. 8.9, 8.10). It is rapidly progressive and is associated with a
high mortality rate, particularly in diabetics. The infection can pass
through Buck's fascia of the penis, dartos fascia of the scrotum and
penis, Colles' fascia of the perineum, and Scarpa's fascia of the
abdominal wall. Two groups of organisms are implicated in necrotizing
fasciitis. Type I includes anaerobic species (Bacteroides and Peptostreptococcus)
and type II group A streptococci alone or with Staphylococcus aureus.
|
|
|

|
|
Necrotizing
Fasciitis Large cutaneous
bullae are seen on the leg of this patient with necrotizing
fasciitis. Note the dark purple fluid in the bullae. (Courtesy of
Lawrence B. Stack, MD.)
|
|
|
|
|

|
|
Necrotizing
Fasciitis Necrotizing
fasciitis with cutaneous necrosis can be seen in the inner thigh of
this patient. (Courtesy of Lawrence B. Stack, MD.)
|
|
Differential Diagnosis
Cellulitis, osteomyelitis, gas
gangrene, streptococcal myonecrosis, infected vascular gangrene, and
trauma should all be considered.
Emergency Department Treatment
and Disposition
Prompt diagnosis is critical in
the treatment of this condition. If the diagnosis is made within 4 days
from the onset of symptoms, the mortality rate is reduced from 50 to 12%.
The initial treatment involves resuscitation with volume expansion. One
recommended initial antibiotic regimen includes a combination of
ampicillin, gentamicin, and clindamycin. Prompt surgical excision is
essential.
Clinical Pearls
1. Intravenous calcium
replacement may be necessary to reverse hypocalcemia from subcutaneous
fat necrosis.
2. Radiographs may be used to
detect subcutaneous gas that is not palpable.
3. Hemolysis and disseminated
intravascular coagulation (DIC) may be seen in association with
necrotizing fasciitis.
4. Necrotizing fasciitis does
not involve muscle, whereas gas gangrene has extensive muscle
involvement.
|
|
Crystal-Induced Synovitis (Gout and Pseudogout)
Associated Clinical Features
Gout is an inflammatory disease
characterized by deposition of sodium urate monohydrate crystals in
cartilage, subchondral bone, and periarticular structures. Gout is most
frequently associated with inborn errors of metabolism,
myeloproliferative disorders, leukemia, hemolytic anemia, glycogen
storage disease, hypertension, diabetes mellitus, obesity, heavy alcohol
consumption, and worsening renal function (gouty nephropathy). An acute
attack is characterized by sudden onset of monarticular arthritis, most
commonly in the metatarsophalangeal (MTP) joint of the great toe (named
after the bad-tempered virgin foot goddess "Podagra") (Fig.
12.9). While the great toe MTP is the most common site, gout can occur in
other joints (Figs. 12.10, 12.11). The deposits of crystals in the
tissues about the joint in gout produce a chronic inflammatory response
termed a tophus. Swelling, erythema, and tenderness are common.
|
|
|

|
|
Podagra Podagra denotes gouty inflammation of the
first MTP joint. Note the swelling and erythema of the left first
MTP. (Courtesy of Kevin J. Knoop, MD, MS.)
|
|
|
|
|

|
|
Gout Large tophi of gout located in and around the
right knee. (Courtesy of Daniel L. Savitt, MD.)
|
|
|
|
|

|
|
Gout The finger is an unusual site for gouty
arthritis. Examination of the synovial fluid confirmed the diagnosis.
(Courtesy of Alan B. Storrow, MD.)
|
|
In pseudogout, calcium
pyrophosphate dihydrate (rod- or rhombus-shaped, weakly birefringent)
crystals are deposited. Pseudogout is most frequently seen in association
with hyperparathyroidism, hemochromatosis, hypophosphatasia,
hypomagnesemia, myxedematous hypothyroidism, and ochronosis. Although any
joint may be involved, knees and wrists are the most common sites. After
joint deposition, the crystals are phagocytized by leukocytes that
release proteolytic enzymes. The acute presenting signs and symptoms are
identical with those of gout, but formation of tophi is not seen with
pseudogout. Fever, pain, and erythema are common to both entities.
Differential Diagnosis
Cellulitis and septic arthritis
must be excluded. In the cell count of the synovial fluid obtained from
an inflamed joint, 2,000 to 50,000 WBCs with polymophonuclear neutrophil
leukocyte (PMN) predominance is expected. Rheumatoid arthritis,
sarcoidosis, hyperparathyroidism, cellulitis, septic arthritis, and
traumatic injury may present much like crystalline-induced synovitis. The
diagnosis is made by seeing negatively birefringent urate crystals or rod
(or rhombus)-shaped, weakly birefringent calcium pyrophosphate dihydrate
crystals on polarized microscopy (see Figs. 21.6A, 21.6B, and 21.6C) with
negative Gram's stain and cultures. Punched out lesions on subchondral
bone may be seen on radiography in chronic tophaceous gout.
Chondrocalcinosis may be seen in pseudogout.
Emergency Department Treatment
and Disposition
Nonsteroidal anti-inflammatory
medications are used with excellent results in the acute setting (e.g.,
indomethacin, 50 mg PO tid if renal function is normal), along with joint
immobilization and rest. Colchicine is a reasonable alternative, but it
often has side effects such as nausea, vomiting, and diarrhea. It is also
associated with serious toxicity, including bone marrow suppression,
neuropathy, myopathy, and death (particularly when given intravenously).
Intramuscular injection of adrenocorticotropic hormone (ACTH, 40 to 80 U
IM or SC) or steroids may be used in patients with contraindications to
colchicine and nonsteroidal anti-inflammatory medications. Intraarticular
injection of steroids will alleviate symptoms rapidly without systemic
side effects. Allopurinol or probenecid are used in the chronic
management of gout and play no role in acute treatment.
Clinical Pearls
1. Most (90%) of patients with
crystalline-induced synovitis are male and older than 40 years.
2. Serum urate may be elevated
or normal during acute episode.
3. Polyarticular presentation
becomes increasingly more common with long-standing disease.
4. Acute gouty arthritis
attacks may be triggered by minor trauma, diuretic or salicylate use,
alcohol abuse, or dietary indiscretion.
|
|
Ingrown Toenail (Onychocryptosis)
Associated Clinical Features
This painful condition is the
result of impingement and puncture of the medial or lateral nail fold
epithelium by the nail plate. Tenderness and swelling of the nail fold is
followed by granulation tissue growth causing sharp pain, erythema, and
further swelling (Fig. 12.12). If not promptly treated, the granulation
tissue becomes epithelialized, preventing elevation of the nail above the
medial or lateral nail groove. Often there is secondary bacterial or
fungal infection.
|
|
|

|
|
Ingrown
Toenail An ingrown toenail on
the medial aspect of the left great toe. (Courtesy of Frank Birinyi,
MD.)
|
|
Differential Diagnosis
Paronychia, felon, and benign or
malignant mass should be considered in the differential diagnosis of an
ingrown toenail.
Emergency Department Treatment
and Disposition
Early: Elevation of the
nail out of nail fold and placement of gauze under nail to prevent
contact, in conjunction with warm soaks, is the initial mode of therapy. Late:
Surgical management involves removal of part of the nail and the inflamed
tissue and sometimes destruction of the involved nail matrix. In the ED,
the lateral portion of the affected nail is removed after digital block
followed by packing of the paronychial fold with petroleum gauze or other
nonadherent dressing. Dressing changes should be done daily, with
follow-up by a podiatrist until growth of the nail plate is complete. The
destruction of the nail matrix is required only in patients with
recurrent infected ingrown toenails and is not part of ED routine
management.
Clinical Pearls
1. Ingrown toenail is most
common in the great toe, is associated with tight-fitting footwear, and
may result from improper nail trimming (i.e., cutting the nail too
short).
2. Antibiotics are indicated
only if cellulitis is suspected, the patient is diabetic, or there is
significant peripheral vascular disease.
3. Use of antibiotics is not a
substitute for surgical excision and will result in only transient
improvement of symptoms.
|
|
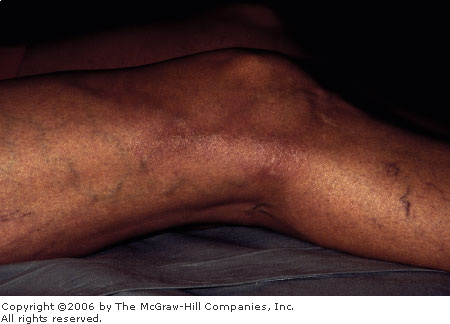
Lymphangitis
Associated Clinical Features
Inflammation of lymphatic
channels in the subcutaneous tissues is commonly caused by the spread of
local bacterial infection. Group A streptococcus is the most frequently
implicated agent. Lymphangitis is characterized by red linear streaks
(Figs. 12.13 and 12.14) extending from the site of infection (e.g.,
finger, toe) to regional lymph nodes (e.g., axilla, groin). The lymph
nodes are often enlarged and tender. There may be associated peripheral
edema of the involved extremity. Lymphangitis may develop within 24 to 48
h of the initial infection.
|
|
|

|
|
Lymphangitis Severe lymphangitis is seen in the lower
extremity. The red streak extends from the ankle to the groin and
follows lymphatic channels. In this case, the site of infection was
the great toe. (Courtesy of Liudvikas Jagminas, MD.)
|
|
|
|
|

|
|
Lymphangitis The lymphangitis extends from the wrist to the
upper arm. Lymphangitis in the upper extremity commonly arises from
nail biting. (Courtesy of Daniel L. Savitt, MD.)
|
|
Differential Diagnosis
Cellulitis, trauma, and
superficial thrombophlebitis are in the differential diagnosis of
lymphangitis.
Emergency Department Treatment
and Disposition
Rest, elevation, and
immobilization in addition to antibiotics are the mainstays of treatment.
Lymphangitis may be treated with oral antibiotics in afebrile patients
who are not immunocompromised. Coverage for Streptococcus and Staphylococcus
is appropriate. Toxic-appearing patients require admission for parenteral
antibiotics. Any patient sent home with oral antibiotics should be
followed up in 24 to 48 h. Patients who subsequently do not show
improvement require admission for parenteral antibiotic therapy.
Clinical Pearls
1. Consider Pasteurella
multocida with cat bites, Spirillum minus with rat bites, and Mycobacterium
marinum in association with swimming pools and aquaria.
2. Chronic lymphangitis may be
associated with mycotic, mycobacterial, and filarial infection.
3. In Africa and Southeast
Asia, filariasis (Wuchereria bancrofti) is the most common
etiologic agent.
|
|
Lymphedema
Associated Clinical Features
Lymphedema occurs from
obstruction of lymphatic channels and is associated with malignancy,
radiation, trauma, surgery, inflammation, infection, parasitic invasion,
paralysis, renal insufficiency, congestive heart failure, cirrhosis, and
malnutrition. Lymphedema is characterized by painless pitting edema (Fig.
12.15), fatigue, increase in limb size—particularly during the day,
and presence of lymph vesicles. The skin becomes thickened and brown in
the late stages.
|
|
|

|
|

|
|
Pitting
Edema Pitting edema is seen in
a woman with lymphedema of the lower extremities. Note how the
impression of the thumb remains on the foot. (Courtesy of Selim
Suner, MD, MS.)
|
|
Differential Diagnosis
Cellulitis, deep venous
thrombosis (DVT), lymphangitis, traumatic hematoma, right heart failure,
tuberculosis, and lymphogranuloma venereum should be considered when the
diagnosis of lymphedema is made. Subcutaneous dye injection, radiographic
lymphography, and radionuclide lymph clearance may be used to aid in the
diagnosis.
Emergency Department Treatment
and Disposition
Control of edema with elevation,
pneumatic compression boots and firm elastic stockings, maintenance of
healthy skin, and avoidance of cellulitis and lymphangitis are the
mainstays of symptomatic treatment. Treatment of the underlying disease
may be curative.
Clinical Pearls
1. Swelling usually starts
distally and progresses proximally.
2. The dorsum of the toes and
feet is always involved in lymphedema, unlike other causes of edema.
3. Careful examination for
right heart failure and screening for renal insufficiency should be
completed for all patients with lymphedema.
|
|
Olecranon and Prepatellar Bursitis
Associated Clinical Features
Bursitis is a reaction in a
fluid-filled synovial sac, commonly over the subacromial (Fig. 12.16),
prepatellar (Fig. 12.17), olecranon, or hip trochanteric bursa. It is
associated with repetitive motion, trauma, or infection. The fluid
collection may be bacterial (septic bursitis, Fig. 12.18), gouty, or,
most commonly, inflammatory. Bursitis is characterized by pain,
tenderness, and swelling. There may be erythema, warmth, and limited
range of motion. It is critical to differentiate septic from benign
inflammation as well as bursal from intraarticular involvement.
Typically, intraarticular arthritis is associated with pain on minor
range of motion, while bursitis discomfort occurs with the stretching of
the skin and synovial sac at the more extreme ranges of joint movement.
The prepatellar bursa is anterior to the infrapatellar tendon. Bursitis
in this area is often the result of repetitive kneeling
("housemaid's knee").
|
|
|
|
|
Olecranon
Bursitis Olecranon bursitis is
evident in this flexed elbow. (Courtesy of Selim Suner, MD, MS.)
|
|
|
|
|

|
|
Prepatellar
Bursitis Local bursal swelling
is evident over the left knee. (Courtesy of Kevin J. Knoop, MD, MS.)
|
|
|
|
|

|
|
Septic
Prepatellar Bursitis This
patient presented with obvious purulence of his right prepatellar
bursal sac. Aspiration confirmed septic bursitis. (Courtesy of Alan
B. Storrow, MD.)
|
|
Differential Diagnosis
Septic arthritis, crystal
synovitis, fracture, contusion, and traumatic effusion may mimic this
condition. Since bursitis does not involve the intraarticular space,
signs and symptoms should be isolated to the bursal area. When this
differentiation is difficult by history and examination, fluid aspiration
and analysis of the bursa or joint for cell count, Gram stain, protein,
glucose, and polarized microscopy (see "Crystal-Induced
Synovitis," above) may be helpful. Fluid with > 50,000 cells per
cubic millimeter, polymorphonuclear neutrophil predominance, increased
protein, reduced glucose, and a positive Gram's stain are associated with
bacterial infection.
Emergency Department Treatment
and Disposition
Rest, bulky compression
dressings, and nonsteroidal anti-inflammatory medications are used for
inflammatory bursitis. Bursal injection of local anesthetics (e.g., 2 to
3 mL of lidocaine or bupivacaine) mixed with corticosteroids (e.g., 1 mL
of betamethasone or methylprednisolone) can also be considered. Reducing
the volume of the inflammatory effusion by aspiration may provide
temporary relief, although the effusion has a propensity to recur. Septic
bursitis requires aspiration, gram-positive antibiotic coverage, and
consideration of open incision and drainage. Most patients can be treated
as outpatients with close follow-up.
In contrast, an intraarticular
infection requires aspiration, antibiotics, and admission for
consideration of open drainage. Aspiration and blood cultures prior to
antibiotic administration are helpful to guide therapy toward specific
organisms. Inflammatory arthritis may be treated with anti-inflammatories,
and intraarticular anesthetics and steroids may be considered.
Clinical Pearls
1. The most important
diagnostic issue is differentiation between bursitis and a septic joint.
2. Septic joint infections in
patients with cancer, who are taking corticosteroids, or who are
intravenous drug users may have lower synovial fluid leukocyte counts
(< 30,000/mm3) then usual (> 50,000/mm3).
3. Incision and drainage are
not recommended for routine inflammatory bursitis.
|
|
Palmar Space Infection
Associated Clinical Features
Palmar space infections occur
within the deep soft-tissue planes of the hand and involve the midpalmar
space, the web spaces (collar button abscess), and the thenar (Fig.
12.19) or hypothenar spaces. These infections commonly arise from callus,
fissures, puncture wounds to the palm, and rupture of flexor
tenosynovitis of the digits. The palm loses its concavity, and there is
dorsal swelling. In addition, tenderness, erythema, warmth, and
fluctuance are evident in the palm. A thenar space infection is
characterized by swelling over the thenar eminence and pain with
abduction of the thumb. With a midpalmar space infection, motion
is limited and painful for the middle and ring fingers. Hypothenar
space infections are extremely rare. A high morbidity is associated
with these infections.
|
|
|

|
|
Palmar
Space Infection Thenar space
infection following injury to the thumb. In this palmar view,
erythema and swelling in the right thenar area and abduction of the
thumb are evident. (Courtesy of Richard Zienowicz, MD.)
|
|
Differential Diagnosis
Cellulitis, local traumatic
injury, fractures, and soft tissue mass are included in the differential
diagnosis of palmar space infections.
Emergency Department Treatment
and Disposition
All deep space infections of the
hand should be managed by a hand surgeon. Prompt incision and drainage in
the operating room is necessary for the best outcome. Frequently, both
palmar and dorsal incisions are necessary. Loose packing and antibiotic
treatment follow surgery. Parenteral antibiotics against Staphylococcus
aureus as well as anaerobes should be started in the ED.
Clinical Pearls
1. Palmar space infections may
cause swelling on the dorsal hand.
2. In general, erythema,
fluctuance, or tenderness are seen on the palmar aspect with very little
seen dorsally.
|
|
Tenosynovitis
Associated Clinical Features
Tenosynovitis, an inflammation of
the tendon and the surrounding synovial sheath, is characterized by pain
and tenderness. Pyogenic flexor tenosynovitis is infection of the tendon
sheath from hematogenous origin, puncture wounds, or local extension.
Tenosynovitis is characterized by the four signs of Kanavel (described
for a finger flexor tendon): mild flexion contracture; fusiform swelling
along the volar finger surface; tenderness along the entire tendon
sheath, especially at the palmar surface of the metacarpophalangeal (MCP)
joint; and severe pain with passive extension (Fig. 12.20). Tenosynovitis
may be complicated by fibrosis and adhesions leading to stiffness, loss
of function, and tendon necrosis from destruction of the blood supply.
|
|
|

|
|
Tenosynovitis This patient presented with flexor
tenosynovitis of the index finger after a laceration at the level of
the palmar DIP joint. Note the fusiform swelling and redness
extending to the thenar eminence. (Courtesy of Selim Suner, MD, MS.)
|
|
Differential Diagnosis
Cellulitis, traumatic injury,
lymphangitis, osteomyelitis, septic arthritis, carpometacarpal arthritis,
and allergic reactions may mimic some of the signs and symptoms of
tenosynovitis.
Emergency Department Treatment
and Disposition
It is difficult to distinguish
infectious and noninfectious etiologies early in the course of this
illness. Early (24 to 48 h) management of tenosynovitis thought to be
noninfectious is accomplished with immobilization and nonsteroidal
anti-inflammatory medications. Parenteral antibiotics, rest,
immobilization, elevation, compressive dressing, and early consultation
with a hand surgeon for incision and drainage within 24 to 48 h are
mandated with pyogenic flexor tenosynovitis.
Clinical Pearls
1. Staphylococcus aureus
is the most common organism, but Streptococcus as well as
gram-negative and anaerobic organisms may also be responsible.
2. The most specific sign of
tenosynovitis is pain with passive extension of the digit.
3. The abductor pollicis longus
(APL), the extensor pollicis brevis (EPB), and the wrist are the most
common sites for tenosynovitis.
4. Finkelstein's test is used
to support the diagnosis of de Quervain's tenosynovitis (Fig. 12.21). The
patient is instructed to make a fist with the thumb tucked inside the
other fingers. The wrist is passively deviated to the ulnar side. Sharp
pain along the APL and EPB tendons denotes a positive Finkelstein's test
and is strong evidence of de Quervain's tenosynovitis.
|
|
|
|
|
Finkelstein's
Test Pain over the radial
styloid is elicited with ulnar deviation of the wrist as shown.
|
|
|
|
Thrombophlebitis
Associated Clinical Features
Thrombophlebitis is superficial
thrombosis and inflammation of veins or varicosities characterized by
redness, tenderness, and palpable, indurated, cordlike venous segments
(Fig. 12.22). Common causes of thrombophlebitis are intravenous catheter
insertion, irritant solutions through the intravenous line, and trauma.
There is little risk of embolism when this condition is associated with
varicose veins or superficial veins distal to the popliteal fossa;
however, pulmonary embolism can occur secondary to propagation of the
thrombus of more proximal veins into the deep venous system.
|
|
|
|
|
Thrombophlebitis This photograph shows thrombophlebitis of the
superficial veins in the leg. The thrombosed veins are erythematous,
close to the surface, and palpable. (Courtesy of Lawrence B. Stack,
MD.)
|
|
Differential Diagnosis
Septic superficial
thrombophlebitis (Fig. 12.23), lymphangitis, deep venous thrombosis
(DVT), and cellulitis should be included in the differential diagnosis of
thrombophlebitis. The patient must be evaluated for the possibility of
deep venous thrombosis if no underlying cause of superficial thrombosis
is elucidated.
|
|
|

|
|
Septic
Thrombophlebitis
Thrombophlebitis may be complicated by bacterial infection. Note the
purulence associated with the erythematous thrombosed veins.
(Courtesy of Lawrence B. Stack, MD.)
|
|
Emergency Department Treatment
and Disposition
Elevation with warm compresses,
rest, and analgesia is sufficient treatment for uncomplicated superficial
thrombophlebitis. Superficial thrombophlebitis and involvement of the
saphenofemoral or iliofemoral system requires admission to the hospital
with anticoagulation and treatment as a DVT. Also, admission to the
hospital is warranted if there is extensive involvement, septic signs,
progression of symptoms despite treatment, or severe inflammatory
reactions.
Clinical Pearls
1. Thrombophlebitis of the
greater saphenous vein may be confused with lymphangitis, since the
lymphatic drainage from the leg runs along the vein.
2. This condition is frequently
associated with malignancy—an association known as Trousseau's
syndrome.
3. Since lymphatic drainage
follows the greater saphenous vein, Doppler studies or venography may be
needed to distinguish superficial thrombophlebitis from lymphangitis in
this area.
|
|
Paronychia
Associated Clinical Features
Paronychia is the most common
infection seen in the hand and is characterized by infection and pus
accumulation along a lateral nail fold. Paronychia may spread to involve
the eponychium (Fig. 12.24) at the base of the nail and the opposite nail
fold if untreated. Staphylococcus aureus is the most frequently
implicated organism.
|
|
|

|
|
Paronychia A paronychia involving one lateral fold and
the eponychium. There is swelling, erythema, and tenderness on the dorsum
of the distal phalanx. (Courtesy of Frank Birinyi, MD.)
|
|
Differential Diagnosis
Felon, dactylitis, herpetic
whitlow, hydrofluoric acid burn, and traumatic injury should be
considered in making the diagnosis of paronychia.
Emergency Department Treatment
and Disposition
If paronychia is recognized
early, warm soaks with or without oral antibiotics may be sufficient.
After 2 to 3 days, there may be sufficient pus accumulation along the
eponychial fold to warrant incision and drainage. After digital block, a
longitudinal incision is made along the eponychial fold. If the affected
portion begins under the nail, removal of the proximal nail may be
necessary. Another technique is elevation of the infected eponychium and
lateral nail fold with a number 11 scalpel blade. Incisions should be
packed open with gauze (removed in 24 to 48 h). Oral antibiotics should
be prescribed, and the finger should be reevaluated in 2 to 3 days.
Clinical Pearls
1. Paronychia is typically
associated with nail biting, manicure trauma, and small foreign bodies.
2. Superinfection with fungal
agents may occur with immunocompromised patients or neglected paronychia.
3. Damage to the germinal
matrix during excision of the nail plate results in nail deformity.
4. It is important to distinguish
a paronychia from herpetic whitlow, where incision and drainage is
contraindicated.
|
|
Hypersensitivity Vasculitis
Associated Clinical Features
This patient presented with
discrete palpable purpuric lesions with central necrosis (Fig. 12.25)
surrounded by a rim of erythema. Biopsies of the lesions demonstrated
leukocytoclastic vasculitis consistent with hypersensitivity vasculitis.
|
|
|

|
|
Hypersensitivity
Vasculitis The palpable
purpura of a patient with hypersensitivity vasculitis secondary to
new use of a nonsteroidal anti-inflammatory medication. (Courtesy of
Lawrence B. Stack, MD.)
|
|
The eruption typically begins in
or is limited to the lower extremities. The palpable, nonblanching
purpura or petechiae are usually secondary to a primary vasculitis or an
embolic event which activates complement proteins. These proteins cause
small blood vessel wall segmental inflammation, necrosis, and fibrin
deposition, much as in Henoch-Schönlein purpura (HSP). Features typical
of this problem include self-limited palpable purpura, adult age, equal
sexual incidence, and lack of other examination or laboratory
abnormalities. There may be systemic involvement of the muscles, joints,
GI tract, or kidney as well as pruritus and pain. The duration can be
acute (especially drug-induced), subacute, or chronic.
Hypersensitivity vasculitis is
more likely if the patient has recently received a new drug, or one known
to cause purpura (Fig. 12.25). It can also be caused by sensitivity to
infectious antigens. The cause is idiopathic in approximately 40 to 60%
of patients.
Differential Diagnosis
The differential of purpura must
include infections (bacterial and viral), hematologic abnormalities
(e.g., thrombotic thrombocytopenic purpura, idiopathic thrombocytopenic
purpura, disseminated intravascular coagulation), collagen-vascular
diseases (e.g., systemic lupus erythematosus, rheumatoid arthritis,
Sjögren's syndrome), and neoplasm. The primary vasculitides—such as
HSP, polyarteritis nodosa, Wegener's granulomatosis, and temporal
arteritis—must also be considered.
The diagnostic criteria for
hypersensitivity vasculitis includes at least three of the following: age
>16 years, related medication, palpable purpura, maculopapular rash,
and appropriate biopsy.
Emergency Department Treatment
and Disposition
Since the differentiation of
hypersensitivity vasculitis with a vasculitis of bacterial origin is
often difficult, initial antibiotic therapy, blood cultures, and
admission are usually indicated. Multiple episodes, especially if
idiopathic, can occur. The suspected medication should be discontinued
immediately, and the use of steroids can be considered. Other treatment
modalities include the use of immunosuppressive medications and
plasmapheresis.
Clinical Pearls
1. Diagnosis of the primary
vasculitides is almost always made histopathologically.
2. There may be overlap between
the causes of purpura.
3. Self-limited or irreversible
damage may occur to the kidneys.
4. Synonyms for this entity
include necrotizing vasculitis and allergic vasculitis.
|
|
Subclavian Vein Thrombosis
Associated Clinical Features
Thrombosis of the subclavian vein
(Paget–Von Schroetter syndrome) is an uncommon condition usually of
iatrogenic origin. It may also be seen in young patients following
exercise and results from compression injury to the subclavian or
axillary vein from a narrow thoracic outlet (effort thrombosis). Symptoms
of pain, discomfort, and tightness or swelling in the arm are manifest
within a day of the thrombosis (Fig. 12.26). Pitting edema develops in
the fingers, hand, and forearm. There is no arterial insufficiency, and
the pulses are palpable. There is a 15% risk of developing pulmonary
embolism from thrombosis of veins in the upper extremity; however, large
or fatal emboli from this source are very rare. Ascending venography is
the gold standard for diagnosis. Duplex scan, impedance plethysmography, and
Doppler studies are also used, but their accuracy has not been studied in
the upper extremity.
|
|
|

|
|
Subclavian
Vein Thrombosis Left
subclavian vein thrombosis is manifest in this patient by swelling of
the left upper extremity. (Courtesy of Frank Birinyi, MD.)
|
|
Differential Diagnosis
Superior vena cava syndrome,
trauma to the upper extremity, congestive heart failure, angioedema, and
lymphatic obstruction must be considered in the differential diagnosis.
Emergency Department Treatment
and Disposition
Treatment consists of elevation,
local heat, analgesia, and anticoagulation with intravenous heparin for
patients presenting with long-term thrombosis. Patients should be
admitted to the hospital. In cases of acute thrombosis (within 5 days of
symptom onset), the treatment is thrombolysis with direct catheter
infusion of urokinase or streptokinase. Surgical thrombectomy has also
been employed. Operative correction of anatomic abnormalities should be
accomplished to prevent long-term morbidity.
Clinical Pearls
1. Swelling of the neck and
face signifies thrombosis of the superior vena cava.
2. The superficial veins in the
upper extremity are often distended and do not collapse when the arm is
elevated.
3. There is a greater incidence
of subclavian vein thrombosis in men and in the right arm.
4. There may be late sequelae
related to the thrombus, such as pain, recurrent swelling, and early
fatigue of the upper extremity.
5. Balloon angioplasty has been
used to correct stenosis of the subclavian vein.
|
|
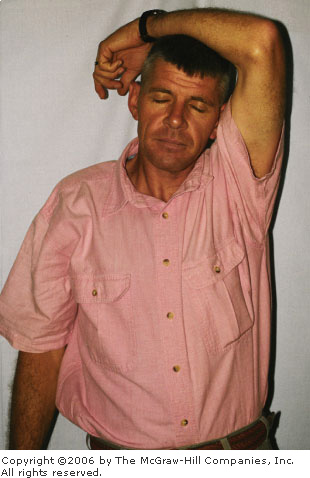
Cervical Radiculopathy
Associated Clinical Features
Cervical radiculopathy is often
caused by compression of a nerve root by a laterally bulging or herniated
intervertebral disk. Osteoarthritis and spondylosis may also cause
radiculopathy in the cervical spine. Pain results from injury to the
nerve roots and nerves innervating the dura, ligaments, facet joints, and
bone. Common clinical features associated with cervical radiculopathy
include pain, paresthesia, and root signs (sensory loss, lower motor
neuron muscle weakness, impaired reflexes, and trophic changes). The pain
is sharp and stabbing and worse with cough, and it radiates over the
shoulder down the arm. There is often numbness and tingling following a
dermatomal distribution. Root signs may be found corresponding to
anatomic distribution of nerves (e.g., triceps muscle weakness, pinprick
deficit along the middle finger, and atrophy with loss of triceps jerk
associated with C-7 radiculopathy). Magnetic resonance imaging (MRI) and
computed tomography (CT) myelography are the commonly used modalities to
distinguish cervical radiculopathy from disk and bone disease. Electromyelography
studies may also be helpful in ruling out other disease processes.
Differential Diagnosis
Trauma, myelopathy, plexopathy,
neurofibromatosis, metastatic tumor infiltration of nerve roots,
neoplasm, shingles, and central cord syndrome should be considered in the
differential diagnosis of cervical radiculopathy.
Emergency Department Treatment
and Disposition
The mainstay of ED treatment is
pain control and referral to an orthopedic surgeon or neurosurgeon. Since
prolonged nerve root compression can lead to permanent neurologic
deficits, immediate referral is necessary for progressive neurologic
signs. Patients with intractable pain, progressive weakness in the upper
extremities, and myelopathy should be admitted to the hospital.
Clinical Pearls
1. Most radiculopathies
resulting from cervical disk disease is seen in the 30 to 60 year age
group and in the C-5 to C-7 region.
2. Risk factors for cervical
radiculopathy include heavy lifting, cigarette smoking, frequent diving
from a board, and prior trauma to the neck.
3. Patients with acute cervical
radiculopathy may present with their upper extremity supported by their
head to counteract the cervical root distraction caused by the weight of
their dependent extremity (Fig. 12.27).
|
|
|
|
|
Cervical
Radiculopathy This is the
classic position of relief for cervical radicular pain. This patient
presented with severe pain in the neck with radiation to the
extremity. The only way the patient was able to get relief was by
holding his arm over his head in the position shown. This patient has
a C5–C6 herniated nucleus pulposus. (Courtesy of Kevin J.
Knoop, MD, MS.)
|
|
|
|
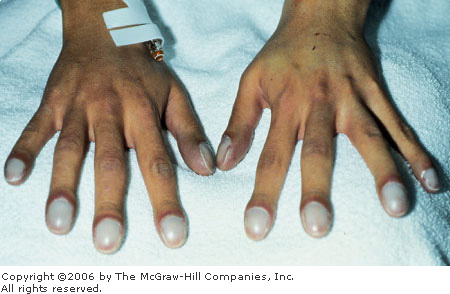
Digital Clubbing
Associated Clinical Features
Digital clubbing results from
increased soft tissue density at the tips of the fingers, particularly on
the dorsum. Associated with the increased tissue mass is enhanced blood
flow, excessive curvature of the fingernails, and hyperemic and swollen
skin folds around the fingernail (Fig. 12.28). Clubbing may also be seen
in the toes. The mechanism underlying clubbing is not known, but it is
postulated that the end result is dilatation of the distal digital blood
vessels with soft tissue hypertrophy. Clubbing may be hereditary,
idiopathic, or acquired and is associated with multiple medical
conditions including carcinoma, intrathoracic sepsis, bacterial
endocarditis, cyanotic congenital heart disease, esophageal disorders,
cirrhosis, inflammatory bowel disease, pulmonary disorders, atrial
myxoma, repeated pregnancies, and pachydermoperiostosis. The incidence of
clubbing with each of these conditions is variable. Digital clubbing may
be reversible in certain disease processes.
|
|
|
|
|
Clubbing Marked digital clubbing can be seen in this
patient. Note the hyperemia in the skin folds around the nail.
(Courtesy of Alan B. Storrow, MD.)
|
|
Differential Diagnosis
Hypertrophic osteoarthropathy,
infection, and trauma should be considered in the differential diagnosis
of clubbing.
Emergency Department Treatment
and Disposition
Treatment of the underlying
condition is indicated. The disposition depends on the underlying
diagnosis and condition of the patient.
Clinical Pearls
1. Bone radiographs can be used
to diagnose hypertrophic osteoarthropathy. Subperiosteal formation of
bone is seen in the distal diaphyses of long bones.
2. Patients rarely recognize
clubbing in their own fingers even if the condition is marked.
|
|
Phlegmasia Dolens
Associated Clinical Features
Phlegmasia alba dolens (painful
white leg, or milk leg) is caused by extensive thrombosis of the
iliofemoral veins and characterized by pitting edema of the entire lower
extremity, tenderness in the inguinal area, and a pale extremity due to
reflex spasm of the femoral artery. Phlegmasia cerulea dolens (painful
blue leg, Fig. 12.29) arises from thrombosis of the veins in the lower
extremity including the perforating and collateral veins resulting in a
cool, painful, swollen, tense, and cyanotic lower extremity, occasionally
with bullae formation. Compartment syndrome and gangrene may follow.
|
|
|

|
|
Phlegmasia
Dolens Phlegmasia cerulea
dolens of the left lower extremity. Note the bluish discoloration and
swelling. (Courtesy of Daniel L. Savitt, MD.)
|
|
Differential Diagnosis
Arterial insufficiency or
thrombosis, aortic dissection, abdominal aortic aneurysm, deep venous
thrombosis, cellulitis, and lymphedema may mimic these conditions.
Doppler ultrasound, impedance plethysmography, and venography (most
accurate for determining extent) are used in the diagnosis.
Emergency Department Treatment
and Disposition
Systemic anticoagulation with
intravenous heparin is indicated for this condition. If there is no improvement
in 12 to 24 h, then iliofemoral venous thrombosis should be suspected.
The role of intravenous thrombolytic therapy is controversial.
Clinical Pearls
1. Pregnancy is one risk factor
for phlegmasia alba dolens.
2. Forty-four percent of
patients with phlegmasia cerulea dolens have an underlying malignancy.
3. Phlegmasia dolens is seen in
fewer than 10% of patients with venous thrombosis.
4. Hypotension may result from
venous pooling of blood in the lower extremity and diminished venous
return to the heart.
5. Petechiae on the skin of the
lower extremity may be present.
|
|
Porphyria Cutanea Tarda
Associated Clinical Features
Porphyrias are problems
associated with enzymatic defects in heme biosynthesis. Porphyria cutanea
tarda (PCT) presents as a condition of fragile skin and vesicles found on
the dorsum of the hands, especially after trauma. The classic symptoms
are easily traumatized skin, leading to blisters in sun-exposed areas,
erosions, milia, and hypertrichosis (Fig. 12.30). It may be induced by
ethanol, estrogens, oral contraceptives, iron overload, and certain
environmental exposures. The typical bullae and erosions may also occur
in other areas, especially the feet and nose. In contrast to other
porphyrias, PCT is not associated with life-threatening respiratory
failure, abdominal pain, or peripheral autonomic neuropathies.
Confirmation of the diagnosis requires 24-h urine testing for various
porphyrins.
|
|
|

|
|
Porphyria
Cutanea Tarda Blisters and
erosions of porphyria cutanea tarda. (Courtesy of Selim Suner, MD,
MS.)
|
|
Differential Diagnosis
Other forms of porphyria, other
bullous diseases, systemic lupus erythematosus (SLE), sarcoidosis, and
Sjögren's syndrome must be considered.
Emergency Department Treatment
and Disposition
Laboratory examination may begin
in the ED with blood chemistries, porphyrin studies, and consideration of
appropriate biopsies. Treatment includes discontinuation of any drugs
that might initiate PCT. Phlebotomy and the use of chloroquine can be
considered.
Clinical Pearls
1. PCT is the most common type
of porphyria.
2. Examination of the urine may
reveal orange-red fluorescence with a Wood's lamp.
3. This condition is sometimes
termed fragile skin.
|
|
Dupuytren's Contracture
Associated Clinical Features
Dupuytren's contracture results
from shortening and fibrotic changes of the subcutaneous tissues of the
palm and longitudinal bands of the palmar aponeurosis. It may begin as a
nodule and then progress to contracture of a finger or fingers (Fig.
12.31). Usually, this is noted at the metacarpophalangeal (MCP) joint,
but the proximal interphalangeal (PIP) or distal interphalangeal (DIP)
joint, may be involved.
|
|
|

|
|
Dupuytren's
Contracture This chronic
problem is seen at the most common site: the ring finger. (Courtesy
of Alan B. Storrow, MD.)
|
|
Emergency Department Treatment
and Disposition
The only effective treatment is
surgery. Recurrence and development of a contracture in other areas may
occur.
Clinical Pearls
1. The flexor tendons are not involved.
2. The ring and small fingers
are the most commonly involved.
|
|
Deep Venous Thrombosis
Associated Clinical Features
Thrombosis in the venous system
results from a disruption of normal hemostasis. As described by Virchow,
blood vessel endothelial injury, coagulopathy, and venous stasis
contribute to formation of clots in the venous system. Deep venous
thrombosis (DVT) is often encountered in patients with intrinsic
coagulopathy or impaired fibrinolysis or those who have had recent
(within 3 months) surgery or trauma. Other associated conditions include
immobilization (e.g., long car or plane trips, bed rest for more than 3
days), increased estrogen (pregnancy, oral contraceptive pills, with
tobacco smoking), cancer, a history of prior DVT, inflammatory disease
processes, or coronary artery disease. Intravenous catheters are also a
major cause of DVT, particularly in the upper extremity.
It is clinically difficult to
tell superficial thrombophlebitis from DVT without diagnostic studies.
Unilateral swelling and tenderness, classically in the calf and thigh,
characterize DVT (Fig. 12.32). Associated erythema, redness and warmth
may lead to a misdiagnosis of cellulitis. Homans' sign—pain
elicited with dorsiflexion of the foot—is not reliable. Even though
venography is considered to be the gold standard test, venous Doppler
ultrasonography is commonly used as the test of choice. Venography is
painful, uses a dye load, and itself may cause DVT. Magnetic resonance
imaging (MRI) is highly sensitive and specific but is costly and not
readily available.
|
|
|

|
|
Deep
Venous Thrombosis This patient
has some classic findings of left lower extremity DVT: swelling,
erythema, pain, and tenderness. (Courtesy of Kevin J. Knoop, MD, MS.)
|
|
Differential Diagnosis
Cellulitis is an important
differential diagnosis. Fracture, lymphedema, heart failure, compartment
syndrome, myositis, arthritis, and superficial phlebitis should also be
considered when DVT is diagnosed. A Baker's cyst is a herniation of the
synovial membrane through the posterior knee capsule. While the acute
clinical presentation is swelling behind the knee, rupture of a Baker's
cyst may present with unilateral swelling similar to DVT (Fig. 12.33).
|
|
|

|
|
Ruptured
Baker's Cyst Comparison of
this patient's ankles reveals circumferential swelling around the
right side. MRI revealed a ruptured Baker's cyst in the right
popliteal fossa. Such a presentation may mimic acute lower extremity
DVT. (Courtesy of Lawrence B. Stack, MD.)
|
|
Emergency Department Treatment
and Disposition
Classic treatment of DVT has been
heparin anticoagulation and admission for warfarin loading. With the
development of low-molecular-weight heparins (LMWH), one may consider a
subgroup for LMWH administration and outpatient treatment. Careful risk
stratification, preexisting protocols, and close medical follow-up are
necessary for successful outpatient treatment. Thrombolysis should be
reserved for severe cases, where the viability of the extremity is
threatened. Although DVT in the calf and superficial veins of the lower
extremity do not typically embolize, these thrombi can propagate into the
deep venous system and may eventually lead to emboli. Serial diagnostic
studies are performed to follow the course of untreated DVT of the distal
calf.
Clinical Pearls
1. Weight-based heparin is 80
U/kg followed by 18 U/kg/h.
2. Patients with unexplained
DVT should be screened for occult malignancy.
3. Measurement of the calf or
Homans' sign should not be used in isolation to rule out DVT.
4. Patients with an unclear
diagnosis of cellulitis should have an objective study to rule out DVT.
|
|
Arsenic Poisoning
Associated Clinical Features
Inorganic arsenic compounds as
well as sodium and potassium arsenite and arsenate are found in insecticides
and wood preservatives as well as in glass manufacturing. Arsine gas is
produced with metal refining, galvanizing, etching, lead plating, and in
the silicone microchip industry. Acute arsenic poisoning, the most common
cause of acute heavy metal poisoning, is encountered in accidental
ingestion, industrial accidents, suicide, and homicide attempts. Low-dose
exposure in industry or from contaminated water and food products may
lead to chronic poisoning. Arsenic poisoning produces a syndrome involving
the skin, hair, nails, GI system, bone marrow, liver, peripheral and
central nervous systems, and kidneys. Acute symptoms of arsenic poisoning
include violent gastroenteritis, hypotension, prolonged QT interval,
seizures, and coma. Other symptoms such as hair loss (Fig. 12.34),
raindrop hyperpigmentation, characteristic Mees' lines on the nails (Fig.
12.35), anemia and leukopenia, jaundice, subacute sensorimotor
polyneuropathy, paralysis, hematuria, and renal failure are
characteristic of chronic arsenic poisoning. Arsine gas exposure results
in hemolysis and secondary renal failure. Arsenic binds with tissue
sulfhydryl groups, causes direct capillary injury, has direct toxic
effects on large organs, and causes uncoupling of oxidative
phosphorylation.
|
|
|

|
|
Arsenic
Poisoning The patchy hair loss
seen in this photograph is from chronic arsenic poisoning. (Courtesy
of Selim Suner, MD, MS.)
|
|
|
|
|

|
|
Arsenic
Poisoning Characteristic Mees'
lines of chronic arsenic poisoning. Note the transverse white lines
on all the nails of both hands. Mees' lines are often seen in
conjunction with polyneuropathy of arsenic poisoning. (Courtesy of
Robert Hoffman, MD.)
|
|
Differential Diagnosis
Similar symptoms may be seen with
other heavy metal ingestions including thallium toxicity, food-borne
toxins, bacterial diarrhea, renal failure, malaria, psoriasis, and
Hodgkin's disease.
Emergency Department Treatment
and Disposition
In the setting of acute arsenic
poisoning, the first priority is to institute advanced life support
measures to stabilize vital signs. Acute ingestion commonly requires
resuscitation with intravenous fluids. Attention is directed to hydration
status, cardiac monitoring, and gathering routine laboratory data.
Standard gastric decontamination techniques, including gastric lavage and
administration of activated charcoal, have been recommended. Although
activated charcoal adsorbs arsenic poorly, it may be effective against
coingestions. Toxicologic consultation should be obtained to determine
the choice of chelating agents, which include dimercaprol (BAL),
dimercaptosuccinic acid (DMSA), and D-penicillamine.
Hemodialysis is indicated in the setting of renal failure. Diagnosis is
based on clinical findings and 24-h urine arsenic level greater than 100
mg. CBC, liver function tests, electrolytes, BUN, creatinine, and
urinalysis may be helpful in the diagnosis. The level of care is
determined by the presentation, but most patients require admission and
observation for a minimum of 24 h. A 24-h urine collection should be
initiated on all admitted patients.
Clinical Pearls
1. Consider the diagnosis of
acute arsenic poisoning in any patient with unexplained hypotension
accompanied or preceded by severe gastroenteritis.
2. Consider the diagnosis of
chronic arsenic poisoning in any patient with a peripheral neuropathy,
typical skin or hair manifestations, or recurrent gastroenteritis.
3. Remote arsenic exposure can
be elucidated by obtaining levels in scalp and pubic hair.
4. There is a garlic odor on
the breath or skin with arsenic poisoning. 5-Arsenic is absorbed through
the skin, lungs, and GI tract and it crosses the placenta.
|
|