|
Note: Large images and
tables on this page may necessitate printing in landscape mode.
Copyright
©2006 The McGraw-Hill Companies. All rights reserved.
Emergency
Medicine Atlas > Part 1. Regional
Anatomy > Chapter 13. Cutaneous Conditions >
|
Erythema Multiforme
Associated Clinical Features
Considered a hypersensitivity
syndrome, erythema multiforme (EM) presents with characteristic target or
iris-shaped papules and vesicobullous plaques (Fig. 13.1). These lesions
are frequently cutaneous manifestations of a drug reaction, viral
infection, Mycoplasma, or malignancy. These plaques are usually
symmetric, pruritic, and painful, often involving the mucous membranes
and extremities, including the palms and soles. The milder form of the
disease has minimal mucosal involvement, no bullae, and no systemic
symptoms. Fever, malaise, extensive mucosal involvement, and other
constitutional symptoms are noted in the severe form of EM, known as
Stevens-Johnson syndrome (see next diagnosis).
|
|
|

|
|
Erythema
Multiforme Note the symmetric
distribution of the target macules. (Courtesy of Michael Redman,
PA-C.)
|
|
Differential Diagnosis
The maculopapular presentation
may be confused with urticaria or fixed drug eruption, whereas the oral
vesicobullous plaques resemble herpetic gingivostomatitis. However, the
cutaneous target lesions and their symmetry are typical of EM.
Emergency Department Treatment
and Disposition
Elimination of any possible
etiology (idiopathic cause noted approximately 50%) and supportive
measures to allay the burning and itching are basic to treating this
disorder. Milder forms of the disease usually resolve spontaneously
within 2 to 3 weeks. Corticosteroids are reserved for the severest
presentations. EM minor can be treated on an outpatient basis. However, patients
with significant systemic illness and additional eruptions involving the
mucosal surfaces (Stevens-Johnson syndrome) may require admission and
supportive care.
Clinical Pearls
1. Symmetrically distributed
target lesions on the extensor surfaces of the extremities and a lack of
significant systemic manifestations are classified as EM minor.
2. Drug-associated EM usually
begins within 2 to 3 weeks of initiating therapy. Sulfonamides and
penicillins are most often the culprits.
3. Many clinicians treat
idiopathic cases empirically with a trial of acyclovir therapy owing to
the high incidence of subclinical herpes simplex infection as the cause
of the EM.
|
|
Stevens-Johnson Syndrome (EM Major)
Associated Clinical Features
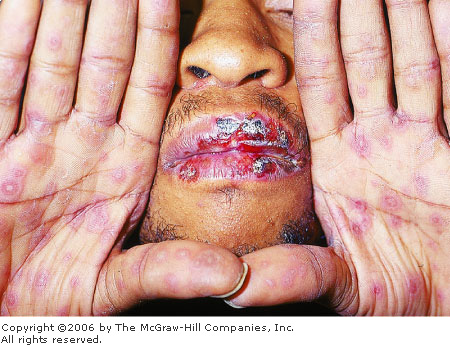
Stevens-Johnson syndrome is a severe,
rarely fatal variety of erythema multiforme. An abrupt onset of
constitutional symptoms precedes the hemorrhagic bullae found on multiple
mucosal surfaces and the edematous, erythematous cutaneous plaques (Fig.
13.2). The bullae erode, producing stomatitis, conjunctivitis,
vulvovaginitis, or balanitis. Patients appear extremely ill and may
develop pneumonia, arthritis, seizures, coma, and hepatic dysfunction.
Death, when it occurs, is usually due to overwhelming sepsis.
|
|
|
|
|
Stevens-Johnson
Syndrome Note the target
lesions on the hands of this patient, as well as the mucosal
involvement on the lips. (Courtesy of Alan B. Storrow, MD.)
|
|
Differential Diagnosis
Meningococcemia must be
considered in the differential diagnosis. The severe involvement of
mucous membranes is characteristic of Stevens-Johnson syndrome.
Emergency Department Treatment
and Disposition
Patients presenting with
significant evidence of toxicity should be admitted to the hospital.
Supportive measures and selective use of systemic corticosteroids are the
cornerstone of therapy.
Clinical Pearls
1. Stevens-Johnson syndrome is
self-limited and usually resolves in approximately 1 month.
2. Sulfonamides, penicillins,
and anticonvulsants are common causes of Stevens-Johnson syndrome.
|
|
Toxic Epidermal Necrolysis
Associated Clinical Features
Toxic epidermal necrolysis (TEN)
is characterized by the formation of erythematous (scalded) skin followed
by widespread bullae (Fig. 13.3), usually a cutaneous manifestation of a
drug reaction. The epidermis eventually becomes necrotic, leading to
extensive exfoliation and exposure of the raw dermis (Fig. 13.4). A prodrome
of fever, fatigue, myalgias, and skin tenderness occurs in the majority
of patients. The mortality rate approaches 25%, with death usually due to
sepsis or gram-negative pneumonia. TEN is generally considered to be the
most severe form of erythema multiforme.
|
|
|

|
|
Toxic
Epidermal Necrolysis Note the
widespread erythematous bullae and epidermal exfoliation. (Courtesy
of James J. Nordlund, MD.)
|
|
|
|
|

|
|
Toxic
Epidermal Necrolysis The
initial bullae have coalesced, leading to extensive exfoliation of
the epidermis. (Courtesy of Keith Batts, MD.)
|
|
Differential Diagnosis
Early in its course, TEN may
resemble scarlet fever, toxic shock syndrome, or erythema multiforme. In
children, staphylococcal scalded-skin syndrome closely mimics TEN;
however, it involves only the superficial epidermis without extension to
the dermis.
Emergency Department Treatment
and Disposition
Supportive care includes
debridement of necrotic tissue, pain control, aggressive hydration,
appropriate antibiotic therapy, and covering exposed dermis, even with
cadaver allografts, to avoid infection and reduce pain. These patients
are best managed in burn treatment centers.
Clinical Pearls
1. Slight pressure causing the
skin to slide laterally and separate from the dermis is a positive
Nikolsky's sign.
2. The initial bullae coalesce,
leading to exfoliation of the entire epidermis.
|
|
Necrotizing (Leukocytoclastic) Vasculitis
Associated Clinical Features
Necrotizing vasculitis is a
hypersensitivity vasculitis in adults associated with infectious agents,
connective tissue diseases, malignancy, and drugs. Symptoms may be
confined to the skin in the form of symmetric petechiae and palpable
purpura over the distal third of the extremities. Systemic vascular
involvement occurs in the kidneys (glomerulonephritis), muscles, joints,
gastrointestinal tract (abdominal pain and bleeding), and peripheral
nerves (neuritis). Henoch-Schönlein purpura (HSP) (Fig. 13.5) is the
classic example of vasculitis in children, consisting of a clinical triad
of palpable purpura, arthritis, and abdominal pain. It is usually a
benign, self-limited disease that occurs in children most commonly after
a bacterial or viral infection.
|
|
|

|
|
Henoch-Schönlein
Purpura Note the classic acral
distribution of HSP. It is immunoglobulin A (IgA)–mediated and
most commonly occurs in children after a streptococcal or viral infection.
(Courtesy of Kevin J. Knoop, MD, MS.)
|
|
Differential Diagnosis
Idiopathic thrombocytopenic
purpura (ITP), disseminated intravascular coagulation (DIC),
meningococcemia, gonococcemia, Rocky Mountain spotted fever,
staphylococcal septicemia, and embolic endocarditis must all be
considered in the differential diagnosis; however, patients with septic
vasculitis are generally more severely ill, with rapidly progressive
symptoms. Also, the purpura of septic vasculitis tend to be fewer in
number, asymmetric, and distal in location. Biopsy of the purpura is
helpful in distinguishing necrotizing vasculitis from septic vasculitis,
DIC, and embolic endocarditis.
Emergency Department Treatment
and Disposition
A majority of cases are
self-limited and require only rest, elevation, and analgesics. Severe
cases with systemic manifestations may require admission for supportive
care, corticosteroids, and cytotoxic immunosuppressive therapy.
Antibiotics should be utilized if the vasculitis follows an infection.
Clinical Pearls
1. The petechiae and purpura of
necrotizing vasculitis are usually localized to the lower third of the
extremities.
2. A patient presenting with
purpura and the signs and symptoms of serum sickness should lead the
examiner to consider necrotizing vasculitis.
|
|
Rocky Mountain Spotted Fever
Associated Clinical Features
Rickettsia rickettsii is
transmitted by the bite of an infected tick. Fever, rigors, headache,
myalgias, and weakness occur 7 to 10 days after inoculation. The
initially blanching macular eruption begins at approximately 4 days on
the distal extremities and somewhat later on the palms and soles (Fig.
13.6). It soon becomes petechial as it spreads centrally to involve the
trunk and abdomen. However, it can also present without obvious cutaneous
manifestations.
|
|
|

|
|
Rocky
Mountain Spotted Fever These
erythematous macular lesions will evolve into a petechial rash that
will spread centrally. (Courtesy of Daniel Noltkamper, MD.)
|
|
Differential Diagnosis
Viral exanthems, drug eruptions,
necrotizing vasculitis, purpuric bacteremia, and meningococcemia may all
resemble this potentially fatal illness.
Emergency Department Treatment
and Disposition
Doxycycline or chloramphenicol is
required for this potentially fatal illness. Doxycycline is the drug of
choice, yet it should be avoided in pregnant or lactating women and
children younger than 8 years of age. Mildly ill patients may be treated
with oral antibiotics on an outpatient basis as long as close follow-up
can be arranged. More severely ill patients should be admitted because
their care can be complicated by circulatory collapse and coma.
Approximately 20% of untreated patients will die; overall mortality is 3
to 7%.
Clinical Pearls
1. Palmar and plantar petechiae
in a severely ill patient should be treated as Rocky Mountain spotted
fever until proved otherwise.
2. Most cases occur between
April and October, with the highest incidence occurring in the Southeast
and South-Central states.
|
|
Disseminated Gonococcus
Associated Clinical Features
Disseminated gonococcus (GC) is a
systemic infection, with septic vasculitis following the hematogenous
dissemination of the organism Neisseria gonorrhoeae. The spectrum of
disease varies from skin lesions alone to skin lesions with tenosynovitis
or septic arthritis. The initial lesion is an erythematous macule that
evolves into a necrotic, purpuric vesicopustule (Fig. 13.7). These
purpura are few in number, asymmetric, and predominantly distal in
location.
|
|
|

|
|
Disseminated
Gonococcus A classic
presentation of the asymmetric purpuric rash, vesicopustule, and
polyarthritis in the hands of an individual with disseminated GC.
(Courtesy of Glaxo Wellcome Pharmaceuticals.)
|
|
Differential Diagnosis
The purpura may resemble
meningococcemia, staphylococcal septicemia, necrotizing vasculitis, or
endocarditis with emboli. Infectious arthritis or tenosynovitis must be
considered when the patient presents with joint complaints. It is
important to obtain Gram's stain of the contents of the vesicopustule, as
well as all other body sites and fluids.
Emergency Department Treatment
and Disposition
Therapy consists of intravenous
or intramuscular ceftriaxone or cefotaxime until symptoms either improve
or resolve, followed by an additional 7 days of orally administered
ciprofloxacin or cefuroxime. Hospitalization is recommended for
noncompliant patients or cases noted to have an associated septic
arthritis.
Clinical Pearls
1. The most common symptom of
disseminated GC is arthralgia of one or more joints, primarily involving
the hands or knees.
2. Skin lesions develop in up
to 70% of cases and will resolve within 4 days regardless of antibiotics.
3. Less than one-third of
patients will have urethritis.
4. The purpura of septic
vasculitis (of whatever bacterial etiology) tend to be fewer in number,
asymmetric, and distal in location.
|
|
Infective Endocarditis
Associated Clinical Features
Infective endocarditis is an
illness characterized by fever, valve destruction, and peripheral
embolization manifested by rare, usually distal purpura. Streptococcus
viridans is the most common causative organism. Janeway lesions (Fig.
13.8) occur in 5% of cases and consist of nontender, small, erythematous
macules on the palms or soles. Osler's nodes (Fig. 13.9) occur in 10% of
cases and consist of transient, tender, purplish nodules on the pulp of
the fingers and toes. Splinter hemorrhages are black, linear
discolorations beneath the nail plate (Fig. 13.10). They are present in
20% of cases and are more suggestive of subacute bacterial endocarditis
(SBE) if present at the proximal or middle nail plate. Murmurs, retinal
hemorrhages, septic arthritis, and significant embolic episodes such as
pulmonary embolism or stroke may also be present.
|
|
|

|
|
Janeway
Lesions Peripheral
embolization to the sole, resulting in a cluster of erythematous
macules known as Janeway lesions. (Courtesy of the Department of
Dermatology, Wilford Hall USAF Medical Center and Brooke Army Medical
Center, San Antonio, TX.)
|
|
|
|
|

|
|
Osler's
Nodes Subcutaneous, purplish,
tender nodules in the pulp of the fingers known as Osler's nodes.
(Courtesy of the Armed Forces Institute of Pathology, Bethesda, MD.)
|
|
|
|
|

|
|
Splinter
Hemorrhages Note the splinter
hemorrhages along the distal aspect of the nail plate, due to emboli
from subacute bacterial endocarditis. (Courtesy of the Armed Forces
Institute of Pathology, Bethesda, MD.)
|
|
Differential Diagnosis
Meningococcemia, gonococcemia,
staphylococcal septicemia, and necrotizing vasculitis must all be
considered in the differential diagnosis. Echocardiography can aid in the
diagnosis.
Emergency Department Treatment
and Disposition
Antibiotics must be appropriate
for the infectious agent; however, therapy is often required before the
diagnosis is confirmed or the infecting organism is known. All toxic
patients require admission, as do all febrile patients who have
prosthetic valves or who are intravenous drug abusers. These patients
should receive gentamicin with nafcillin or vancomycin empirically
pending the blood culture results. Patients with rheumatic or congenital
valve abnormalities may receive streptomycin with penicillin or
vancomycin.
Clinical Pearls
1. Janeway lesions, Osler's
nodes, and splinter hemorrhages in a febrile patient with a murmur are
virtually diagnostic of infective endocarditis.
2. Rheumatic heart disease is
the most common predisposing factor, with the mitral valve being the most
common site of damage.
3. Congenital heart disease,
intravenous drug abuse, and prosthetic heart valves are additional
predisposing factors to the development of infective endocarditis.
|
|
Idiopathic Thrombocytopenic Purpura
Associated Clinical Features
Idiopathic thrombocytopenic
purpura (ITP) occurs as the result of platelet injury and destruction.
Pinpoint, red, nonblanching petechiae or nonpalpable purpura and
ecchymoses are found on the skin (Fig. 13.11) and mucous membranes,
either spontaneously (platelets <10,000/mm3) or at the site
of minimal trauma (platelets <40,000/mm3). Melena,
hematochezia, menorrhagia, and severe intracranial hemorrhages may also
occur in conjunction with the purpura. The acute form affects children 1
to 2 weeks after a viral illness; the chronic form occurs most often in
adults, with women outnumbering men 3:1, and may present with an
associated splenomegaly.
|
|
|

|
|
Idiopathic
Thrombocytopenic Purpura This
thrombocytopenic patient with splenomegaly has pinpoint,
nonblanching, nonpalpable petechiae. (Courtesy of the Department of
Dermatology, Wilford Hall USAF Medical Center and Brooke Army Medical
Center, San Antonio, TX.)
|
|
Differential Diagnosis
Nonhemorrhagic vascular
dilatations like telangiectasia or true petechiae and purpura, as found
in scurvy or posttraumatic purpura, must be differentiated from this
potentially debilitating illness. Assessment of the platelet count aids
in making the diagnosis.
Emergency Department Treatment
and Disposition
Hospitalization at the time of
diagnosis is recommended because the differential diagnosis is extensive
and the bleeding risks are significant. Platelets are transfused only if
there is life-threatening bleeding or the total count is <10,000/mm3.
Immunosuppressive drugs, steroids, and intravenous immunoglobulin are of
benefit in the acute cases; splenectomy is utilized in chronic cases.
Clinical Pearls
1. Petechiae and purpura in a
thrombocytopenic patient with splenomegaly make the diagnosis.
2. The acute form of ITP has an
excellent prognosis (90% spontaneous remission), whereas the course of
chronic ITP is one of varying severity with little hope of remission.
|
|
Thrombotic Thrombocytopenic Purpura (TTP)
Associated Clinical Features
The diagnosis of thrombotic
thrombocytopenic purpura (TTP) is characterized by the following pentad
of symptoms:
1. Microangiopathic hemolytic
anemia, with characteristic schistocytes on the peripheral blood smear
and a reticulocytosis.
2. Thrombocytopenia with
platelet counts ranging from 5000 to 100,000/ L (Fig.
13.12). L (Fig.
13.12).
3. Renal abnormalities
including renal insufficiency, azotemia, proteinuria, or hematuria.
4. Fever.
5. Neurologic abnormalities
including headache, confusion, cranial nerve palsies, seizures, or coma.
|
|
|

|
|
Thrombic
Thrombocytopenic Purpura
Bleeding at initial presentation is seen in about 30 to 40% of
patients with TTP. (Courtesy of James J. Nordlund, MD.)
|
|
The disease affects women more
than men and can affect any age group, but it occurs most commonly in
ages 10 to 60.
Differential Diagnosis
Hemolytic uremic syndrome (HUS),
disseminated intravascular coagulation, and the pregnancy-associated
HELLP (Hemolysis, Elevated Liver enzymes, Low Platelet count) syndrome
can all present like TTP. HUS and TTP appear to be closely related and
may represent variants of a single disease.
Emergency Department Treatment
and Disposition
The cornerstone of therapy is
plasma exchange transfusion. Some patients can be treated with plasma
infusions alone. It is thought that the transfusions provide a missing
substrate and the exchange may remove some unknown toxic substance.
Prednisone and antiplatelet therapy with aspirin may be helpful. Patients
recalcitrant to standard therapy may be treated with immunosuppressives
(vincristine, azathioprine, cyclophosphamide) and even splenectomy. All
patients should be admitted.
Clinical Pearls
1. Platelet transfusions should
be avoided unless there is life-threatening hemorrhage; they can worsen
the thrombotic process.
2. Typically TTP is acute and
fulminant, but it can become a chronic, relapsing form.
3. Hemoglobin less than 6 g/dL,
platelet count less than 20,000, elevated indirect bilirubin and LDH, and
a negative Coombs test are typically found.
|
|
Livedo Reticularis
Associated Clinical Features
Livedo reticularis presents as a
macular, reticulated (lace-like) patch of nonpalpable cutaneous vasodilatation
(Fig. 13.13) in response to a variety of vascular occlusive processes.
This pattern predominates in the peripheral or acral areas and may or may
not be associated with purpura. In time, the overlying epidermis and
dermis may infarct and form ulcerations or develop palpable dermal
papules or nodules. Livedo reticularis is usually representative of a
severe underlying systemic disease. Inflammatory vascular diseases
(livedo vasculitis, polyarteritis nodosa, lupus erythematosus), septic
emboli (meningococcemia), tumors (pheochromocytoma), and systemic
illnesses associated with mechanical vessel blockage (anticardiolipin
antibody syndrome, polycythemia vera, sickle cell anemia, cholesterol
embolus) are a few diseases associated with or responsible for livedo
reticularis. It can also occur independent of any disease association.
|
|
|

|
|
Livedo
Reticularis Note the
reticulated (lace-like) blanching erythema symmetrically distributed
over the lower extremities. (Courtesy of James J. Nordlund, MD.)
|
|
Differential Diagnosis
The most important consideration
in making this diagnosis is to rule out an associated vascular occlusion
of whatever etiology.
Emergency Department Treatment
and Disposition
The treatment of livedo
reticularis is treatment of the underlying disorder and avoiding exposure
to cold.
Clinical Pearls
1. Livedo vasculitis is an
inflammatory vascular disease usually found symmetrically on the ankles
and dorsum of the feet. It consists of painful stellate-shaped
ulcerations surrounded by an erythematous livedo pattern.
2. Cholesterol emboli usually
occur after an intraarterial procedure. Pain often precedes the livedo
pattern of purpura on the distal extremities.
3. Patients with
anticardiolipin antibody syndrome have extensive livedo reticularis and
recurrent arterial and venous thromboses involving multiple organ
systems.
|
|
Herpes Zoster
Associated Clinical Features
Herpes zoster is a dermatomal,
unilateral reactivation of the varicella zoster virus. Pain, tenderness,
and dysesthesias may present 4 to 5 days prior to an eruption composed of
umbilicated, grouped vesicles on an erythematous, edematous base (Fig.
13.14). The vesicles may become purulent or hemorrhagic. Nerve
involvement may actually occur without cutaneous involvement. Ophthalmic
zoster involves the nasociliary branch of the fifth cranial nerve and
presents with vesicles on the nose and cornea (Hutchinson's sign).
Ramsay-Hunt syndrome is a herpes zoster infection of the geniculate
ganglion that presents with decreased hearing, facial palsy, and vesicles
on the tympanic membrane, pinna, and ear canal.
|
|
|

|
|
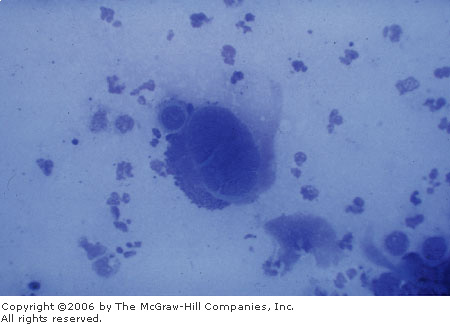
Herpes
Zoster This eruption consists
of a dermatomal distribution of umbilicated vesicles on an
erythematous base. Note the occasional cluster of hemorrhagic
vesicles. Tzank smear is positive. (Courtesy of the Department of
Dermatology, Wilford Hall USAF Medical Center and Brooke Army Medical
Center, San Antonio, TX.)
|
|
Differential Diagnosis
The most likely differential
diagnosis is herpes simplex infection, which is usually recurrent. Herpes
zoster recurs in fewer than 5% of immunocompetent patients. The eruption
may resemble contact dermatitis, localized cellulitis, or grouped insect
bites. The prodromal pain must be differentiated from potential pleural,
cardiac, or abdominal origin. Tzank smear of the floor of a vesicle
demonstrating multinucleated giant cells makes the diagnosis of a herpes
family infection (Fig. 13.15). Cultures may be necessary to distinguish
herpes zoster forms.
|
|
|
|
|
Herpes
Zoster A Tzank smear of both
the roof and floor of a herpetic vesicle demonstrating a
multinucleated giant cell. (Courtesy of the Department of
Dermatology, Wilford Hall USAF Medical Center and Brooke Army Medical
Center, San Antonio, TX.)
|
|
Emergency Department Treatment
and Disposition
Uncomplicated cases of herpes
zoster can be managed with supportive care, especially pain control.
Admission to the hospital for intravenous acyclovir is usually reserved
for complicated cases involving multiple dermatomal distribution or the
ophthalmic branch of the trigeminal nerve, disseminated disease, or
immunocompromised patients. Acyclovir or famciclovir hasten the healing
and decreases the pain if started within 72 h of appearance of the
vesicles. These agents have also been shown to reduce the duration of
postherpetic neuralgia. Prednisone may also prove useful. Herpes zoster
keratitis requires immediate ophthalmologic consultation to avoid any
potential vision loss.
Clinical Pearls
1. Dermatomally grouped,
umbilicated vesicles on an erythematous base are diagnostic of herpes
zoster.
2. The thorax is the most
common area involved, followed by the face (trigeminal nerve).
3. The nonimmune or
immunocompromised should avoid lesional contact from prodrome until
reepithelialization, since the crusts can contain the varicella zoster
virus.
4. Typically, an infected
patient may transmit chickenpox to a nonimmune individual.
5. Zoster during pregnancy
seems to have no deleterious effects on the mother or baby.
|
|
Herpetic Whitlow
Associated Clinical Features
Herpetic whitlow is a painful
herpes simplex infection of the distal finger characterized by edema,
erythema, vesicles, and/or pustules grouped on an erythematous base (Fig.
13.16). Fever, lymphangitis, and regional adenopathy often accompany the
lesion.
|
|
|

|
|
Herpetic
Whitlow Note the cluster of
vesicles on an erythematous base located at the distal finger. Tzank
smear is positive. (Courtesy of Lawrence B. Stack, MD.)
|
|
Differential Diagnosis
Paronychia, felon, and contact
dermatitis must be differentiated from this contagious illness. A Tzank
smear of the floor of the vesicle demonstrating multinucleated giant
cells makes the diagnosis.
Emergency Department Treatment
and Disposition
Acyclovir in addition to
analgesics and antipyretics are useful. To be most effective, acyclovir
must be started within 72 h of the appearance of the eruption. Topical
antibiotic ointments help prevent secondary infection and may speed
healing.
Clinical Pearls
1. Grouped, umbilicated
vesicles on an erythematous base are diagnostic of a herpes family
infection.
2. Wear protective gloves;
herpetic whitlow is an occupational hazard in the medical and dental
professions.
|
|
Erysipelas
Associated Clinical Features
Erysipelas is a group A
streptococcal cellulitis involving the skin to the level of the dermis.
The plaque is typically erythematous, edematous, and painful, with an
elevated, well-demarcated border (Fig. 13.17). The associated edema tends
to make the plaque appear shiny. Erysipelas frequently occurs on the face
and lower extremities.
|
|
|

|
|
Erysipelas Note the well-demarcated, edematous,
erythematous, shiny plaque. (Courtesy of the Department of
Dermatology, Wilford Hall USAF Medical Center and Brooke Army Medical
Center, San Antonio, TX.)
|
|
Differential Diagnosis
Other significant
illnesses—such as deep venous thrombosis, thrombophlebitis, and
necrotizing fasciitis—must be ruled out.
Emergency Department Treatment
and Disposition
All infections require rest,
elevation, heat, and antibiotics. Mild presentations may be treated on an
outpatient basis with oral dicloxacillin or erythromycin in
penicillin-allergic patients. More severe illness or toxicity requires
hospitalization and intravenous antibiotics.
Clinical Pearls
1. The well-demarcated, tender,
shiny, erythematous plaque is diagnostic of erysipelas.
2. This same shiny, erythematous
plaque on the face of a febrile child may be caused by Haemophilus
influenzae, necessitating intravenous chloramphenicol or a
cephalosporin.
3. Lymphatic streaking is more
common in erysipelas than cellulitis.
|
|
Hot Tub Folliculitis
Associated Clinical Features
Hot tub folliculitis is a
pruritic, follicular, pustular eruption confined to the hair follicle and
is secondary to a cutaneous infection with Pseudomonas aeruginosa
(Fig. 13.18). Headache, sore throat, earache, and fever may accompany the
pustules, which usually localize to the trunk and proximal extremities.
|
|
|

|
|
Hot
Tub Folliculitis Note the
pustules localized to the hair follicles of the trunk and proximal
extremity. (Courtesy of Jeffrey S. Gibson, MD.)
|
|
Differential Diagnosis
Other forms of folliculitis
(including those caused by Staphylococcus aureus), acne, and
miliaria rubra are usually considered in the differential diagnosis.
Emergency Department Treatment
and Disposition
The folliculitis usually
involutes in 7 to 10 days without treatment. Acetic acid compresses and
local wound cleansing may speed recovery. In addition, the hot tub or
source of exposure must be decontaminated to avoid reexposure.
Clinical Pearls
1. Pruritic pustules confined
to the hair follicles of the trunk and proximal extremities is diagnostic
of folliculitis.
2. This most commonly occurs in
individuals who use hot tubs, whirlpools, or saunas.
3. This may also result from
contact with chemicals (exfoliative beauty aids) or repetitive physical
trauma (friction from tight clothing).
|
|
Ecthyma Gangrenosum
Associated Clinical Features
Ecthyma gangrenosum is a Pseudomonas
aeruginosa infection that usually occurs in the septic,
immunocompromised, or neutropenic patient. The initially erythematous
macules develop bullae or pustules (Fig. 13.19) surrounded by violaceous
halos. The pustules become hemorrhagic and rupture, forming painless
ulcers with necrotic, black centers.
|
|
|

|
|
Ecthyma
Gangrenosum A typical
hemorrhagic bulla of ecthyma gangrenosum secondary to pseudomonal
sepsis. (Courtesy of James Mensching, MD.)
|
|
Differential Diagnosis
Necrotizing vasculitis, fixed
drug eruptions, pyoderma gangrenosum, and brown recluse spider bites must
all be considered in the differential diagnosis.
Emergency Department Treatment
and Disposition
These patients are usually septic
and immunocompromised. Admission is usually required for the patient to
receive antipseudomonal antibiotics and general supportive care.
Clinical Pearls
1. Consider ecthyma gangrenosum
when examining a septic patient who presents with bullae or pustules that
rupture and form painless, necrotic ulcers.
2. It is important to consider
underlying immunodeficiency when making this diagnosis.
|
|
Pityriasis Rosea
Associated Clinical Features
Pityriasis rosea is a mild
inflammatory, exanthematous, papulosquamous eruption. The pathognomonic
finding is an oval salmon-colored papule with a central collarette of
scale. It primarily occurs on the trunk with the long axis of the oval
papule following the lines of cleavage in a Christmas tree–like
distribution (Fig. 13.20). A herald patch, consisting of a much larger
plaque with central clearing and scales, frequently precedes the
exanthematous phase by 1 to 2 weeks (Fig. 13.21). The eruption usually
lasts 4 to 6 weeks and is frequently pruritic.
|
|
|

|
|
Pityriasis
Rosea An exanthematous,
papulosquamous eruption, with the long axis of the oval papules
following the lines of cleavage in a Christmas tree–like
eruption. (Courtesy of James J. Nordlund, MD.)
|
|
|
|
|

|
|
Herald
Patch A herald patch precedes
the exanthematous phase: a larger, oval, salmon-colored patch with a
central collarette of scale. (Courtesy of the Department of
Dermatology, Wilford Hall USAF Medical Center and Brooke Army Medical
Center, San Antonio, TX.)
|
|
Differential Diagnosis
This must be differentiated from
the secondary lesions of syphilis, tinea versicolor, and some drug
eruptions.
Emergency Department Treatment
and Disposition
Symptomatic treatment is usually
all that can be offered to the patient. Antihistamines may alleviate the
associated pruritus. Ultraviolet light has also been used with some
success.
Clinical Pearls
1. A salmon-colored papule with
central scale, negative KOH examination for hyphae, and negative
serologic testing for syphilis makes the diagnosis of pityriasis rosea.
2. It frequently appears in
very atypical form in dark-skinned individuals (acral, face, and genital
location).
|
|
Secondary Syphilis
Associated Clinical Features
The initial papules of secondary
syphilis are usually asymptomatic, although they may be painful or
pruritic; they appear 2 to 10 weeks after the primary chancre. Headache,
sore throat, fever, arthralgias, myalgias, and a generalized
lymphadenopathy may also be present. These exanthematous papules are
symmetric and nondestructive, usually forming a pityriasis
rosea–like pattern on the trunk, palms, and soles (Figs. 13.22,
13.23). Later lesions are firm, pigmented papules with a coppery tint and
adherent scales (Fig. 13.24). Macerated papules may form on the mucous
membranes; "motheaten" alopecia may occur on the scalp; and
condylomata lata may occur in the intertriginous areas.
|
|
|

|
|
Secondary
Syphilis These eruptive,
scaly, copper-colored papules on the foot may be the initial
presentation of secondary syphilis. They are usually symmetric,
asymptomatic, and nondestructive. (Courtesy of the Department of
Dermatology, Wilford Hall USAF Medical Center and Brooke Army Medical
Center, San Antonio, TX.)
|
|
|
|
|

|
|
Secondary
Syphilis These firm,
pigmented, erythematous papules are characteristic of secondary
syphilis. (Courtesy of Lynn Utecht, MD.)
|
|
|
|
|

|
|
Secondary
Syphilis These firm, pigmented
papules with a coppery tint and adherent scale are characteristic.
(Courtesy of the Department of Dermatology, Wilford Hall USAF Medical
Center and Brooke Army Medical Center, San Antonio, TX.)
|
|
Differential Diagnosis
Syphilis is "the great
imitator." It may resemble psoriasis, drug eruptions, pityriasis
rosea, viral exanthems, tinea corporis, tinea versicolor, and condyloma
acuminata. A positive serologic test for syphilis makes the diagnosis.
Emergency Department Treatment
and Disposition
Penicillin is the agent of choice
for treatment, with tetracycline or erythromycin used in cases of
penicillin allergy. A Jarisch-Herxheimer reaction may occur several hours
after treatment with antibiotics, correlating with the clearance of
spirochetes from the bloodstream. This reaction lasts approximately 24 h,
yet it may be more threatening than the disease itself. Increasing fever,
rigors, myalgias, headache, tachycardia, hypotension, and a drop in the
leukocyte and platelet count may be encountered. Fluid resuscitation to
maintain the blood pressure and supportive care may be needed.
Clinical Pearls
1. Scaly palmar and plantar
papules are strongly suggestive of secondary syphilis, the incidence of
which is rising.
2. These scaling red-brown
papules appear 2 to 10 weeks after the spontaneous resolution of the
initial painless chancre.
3. The latent stage follows the
resolution of the papules; it is characterized by a positive serology and
an absence of signs and symptoms.
4. Tertiary syphilis occurs in
untreated or poorly treated patients and may manifest itself as general
paresis, tabes dorsalis, optic atrophy, and aortitis with aneurysms.
5. It is important to consider
the prozone phenomenon (falsely negative agglutination in undiluted
serum) in an AIDS patient with presumed syphilis in whom the serologic
test is negative.
|
|
Erythema Chronicum Migrans (ECM)
Associated Clinical Features
Borrelia burgdorferi is
the tick-borne spirochete responsible for Lyme borreliosis, and erythema
chronicum migrans (ECM) is the pathognomonic rash of Lyme disease
occuring early in the infection. The initial prodromal symptoms of fever,
myalgias, arthralgias, and headache are followed by a macule or papule
progressing to a plaque at the site of the bite. This plaque expands its
red, raised border as it clears centrally, leading to an annular
appearance (Fig. 13.25). The plaque may burn and is rarely pruritic. On
average, there are 9 days between the time of the bite and the appearance
of the rash.
|
|
|

|
|
Erythema
Chronicum Migrans (ECM) This
pathognomonic eruption of Lyme disease forms at the site of the tick
bite. The initial papule forms into a slowly enlarging oval area of
erythema while clearing centrally. (Courtesy of Timothy Hinman, MD.)
|
|
Differential Diagnosis
This annular plaque may resemble
a fixed drug eruption, tinea corporis, urticaria, or the herald patch of
pityriasis rosea. The multiple secondary annular papules and plaques that
may rarely form can resemble secondary syphilis. However, the
Lyme-related eruption spares the palms and soles.
Emergency Department Treatment
and Disposition
The duration of antibiotic
treatment (10 to 30 days) depends on the severity of the symptoms.
Tetracycline or doxycycline are the drugs of choice. Pregnant or
lactating females and children younger than 8 years of age should be
treated with penicillin or amoxicillin. Erythromycin is a suitable
alternative. Patients with minimal symptoms may be treated on an
outpatient basis. Those patients with significant toxicity and
complications require admission, supportive care, and parenteral
antibiotics.
Clinical Pearls
1. An annular plaque arising at
the site of a tick bite in a patient with systemic symptoms should be
treated as Lyme disease until proved otherwise.
2. Stage I of Lyme disease
consists of constitutional symptoms and the characteristic rash of ECM.
3. Stage II of Lyme disease
consists of neurologic (aseptic meningitis, encephalitis, bilateral
Bell's palsy) and cardiac (myocarditis, conduction blocks)
manifestations.
4. Stage III of Lyme disease
consists of an asymmetric, episodic, oligoarticular arthritis.
|
|
Tinea Corporis, Faciale, and Manus
Associated Clinical Features
Tinea corporis includes all
dermatophyte infections excluding the scalp, face, hands, feet, and
groin. The dermatophytosis is pruritic and consists of well circumscribed
scaly plaque with a slightly elevated border and central clearing (Fig.
13.26). This annular configuration is most commonly found on the trunk
and neck. Skin scrapings viewed with a KOH preparation exhibit septate
hyphae.
|
|
|

|
|
Tinea
Corporis This dermatophytosis
is known as ringworm, a well-defined, pruritic, scaly plaque with a
raised border and central clearing (annular). KOH preparation is
positive. (Courtesy of the Department of Dermatology, Wilford Hall
USAF Medical Center and Brooke Army Medical Center, San Antonio, TX.)
|
|
Tinea faciale is a dermatophyte infection of the
facial skin. It commonly appears as a well circumscribed erythematous
patch (Fig. 13.27). Tinea manus is a dermatophyte infection of the hands
(Fig. 13.28).
|
|
|

|
|
Tinea
Faciale Note the sharply
marginated, polycyclic, scaly plaque with central clearing localized
to the face. KOH preparation is positive. (Courtesy of the Department
of Dermatology, Wilford Hall USAF Medical Center and Brooke Army
Medical Center, San Antonio, TX.)
|
|
|
|
|

|
|
Tinea
Manus This dermatophytosis is
usually unilateral when it involves the hands. Note the diffuse
hyperkeratosis of the left hand as well as involvement of both feet
(tinea pedis). (Courtesy of James J. Nordlund, MD.)
|
|
Differential Diagnosis
Pityriasis rosea, secondary
syphilis, psoriasis, seborrheic dermatitis, and tinea versicolor are all
usually considered in the differential diagnosis. A KOH examination of
the scale demonstrating hyphae confirms the diagnosis.
Emergency Department Treatment
and Disposition
Small, localized plaques may be
treated with a topical antifungal cream. Extensive or resistant infection
requires systemic griseofulvin or ketoconazole. It is important to treat
for 2 weeks beyond the point of clinical cure to ensure successful
eradication of the fungus.
Clinical Pearls
1. The scale is usually located
at the leading edge of erythema and provides the best yield for scraping
as part of the KOH examination.
2. The recurrence rate is high,
especially for tinea manus.
|
|
Tinea Cruris
Associated Clinical Features
Tinea cruris, or "jock itch,"
is a pruritic dermatophytosis of the intertriginous areas, usually
excluding the penis and scrotum. The scaly, erythematous plaque spreads
peripherally, with central clearing (Fig. 13.29). The borders of the
plaque are well defined.
|
|
|

|
|
Tinea
Cruris This dermatophytosis is
commonly called "jock itch." Note the erythematous, scaly
plaque with its well-defined border. It characteristically does not
involve the scrotum or penis. KOH preparation is positive. (Courtesy
of James J. Nordlund, MD.)
|
|
Differential Diagnosis
Erythrasma, Candida albicans,
seborrheic dermatitis, and psoriasis are usually considered in the differential
diagnosis. A KOH examination of the scale demonstrating hyphae confirms
the diagnosis.
Emergency Department Treatment
and Disposition
Initial treatment consists of
topical antifungal medications. Griseofulvin or ketoconazole are reserved
for resistant cases. It is important to treat for 1 week beyond the point
of clinical cure to ensure successful eradication of the fungus.
Decreasing the amount of perspiration by using topical powders may help
prevent recurrences.
Clinical Pearls
1. A less well defined,
pruritic, intertriginous plaque that typically involves the scrotum is
usually erythrasma. It is caused by Nocarelia minutissimus and is
treated with topical erythromycin.
2. Warmth and moisture are
predisposing factors.
|
|
Tinea Pedis
Associated Clinical Features
Tinea pedis, or "athlete's
foot," is a pruritic dermatophytosis. It consists of erythema and
scaling of the sole (see Fig. 13.28), maceration, occasional
vesiculation, and fissure formation between and under the toes (Fig.
13.30). These pruritic, painful fissures may become secondarily infected
with gram-negative organisms. Frequently the toenails are also affected.
|
|
|

|
|
Tinea
Pedis A pruritic, scaling
hyperkeratotic rash involving the soles of the feet and extending to
the interdigital spaces is pathognomonic for tinea pedis. (Courtesy
of James J. Nordlund, MD.)
|
|
Differential Diagnosis
Foot eczema, psoriasis, and
Reiter's syndrome are considered in the differential diagnosis. A KOH
examination of the scale demonstrating hyphae confirms the diagnosis.
Emergency Department Treatment
and Disposition
Topical antifungal creams are the
initial treatment of choice. Antibiotics may be used to treat secondary
infection. Griseofulvin, then ketoconazole, are used for chronic or
resistant cases. It is important to treat for 1 week beyond the point of
clinical cure to ensure successful eradication of the fungus.
Clinical Pearls
1. If it scales, scrape it and
look for hyphae.
2. Macerated areas may become
secondarily infected by bacteria.
|
|
Tinea Capitis
Associated Clinical Features
Tinea capitis is scalp ringworm,
or a dermatophytosis of the scalp. It presents as a pruritic,
erythematous, scaly plaque with broken or missing hairs frequently
referred to as "gray patch" or "black dot" ringworm
(Fig. 13.31). This may develop into a kerion. A kerion is a delayed-type
hypersensitivity reaction to the fungus, where the initial erythematous,
scaly plaque becomes boggy with inflamed, purulent nodules and plaques
(Fig. 13.32). The hair follicle is frequently destroyed by the
inflammatory process in a kerion, leading to a scarring alopecia.
|
|
|

|
|
Tinea
Capitis This dermatophytosis
is characterized by a pruritic, circular area of hair loss covered by
adherent scales. KOH preparation is positive. (Courtesy of the
Department of Dermatology, Wilford Hall USAF Medical Center and
Brooke Army Medical Center, San Antonio, TX.)
|
|
|
|
|

|
|
Kerion This collection of boggy, inflamed, purulent
nodules and papules is the result of a delayed-type hypersensitivity
reaction to the fungus. Scarring alopecia will follow as a result of
the actual destruction of the hair follicle. (Courtesy of the
Department of Dermatology, Wilford Hall USAF Medical Center and
Brooke Army Medical Center, San Antonio, TX.)
|
|
Differential Diagnosis
Various inflammatory follicular
conditions—such as folliculitis, impetigo, psoriasis, alopecia
areata, and seborrheic dermatitis—may resemble tinea capitis. The
diagnosis is made by a KOH examination of a scraping of the area,
revealing hyphae and spores.
Emergency Department Treatment
Disposition
Systemic griseofulvin is usually
required for several weeks to treat tinea capitis successfully. Systemic
antibiotics and corticosteroids are usually added when treating a kerion.
Selenium sulfide lotion used as a shampoo may actually decrease the
duration of the infection. It is important to treat for 2 weeks beyond
the point of clinical cure to ensure successful eradication of the
fungus. Ketoconazole is reserved for resistant cases.
Clinical Pearls
1. Tinea capitis is a disease
of childhood; it is rare in immunocompetent adults.
2. It is epidemic in many
African American communities.
3. The KOH scrape is aided by
using a disposable urethral brush or similar device.
|
|
Onychomycosis
Associated Clinical Features
Onychomycosis is an invasion of
the nails by any fungus. Four clinical subtypes are noted. Distal
subungual presents as discolorations of the free edge of the nail
with hyperkeratosis leading to a subungual accumulation of friable
keratinaceous debris (Fig. 13.33). White superficial consists of
sharply outlined white areas on the nail plate which leave the surface
friable. Proximal subungual presents as discolorations which start
proximally at the nail fold. Candidal onychomycosis encompasses
the entire nail plate, leaving the surface rough and friable.
|
|
|

|
|
Onychomycosis Note that multiple nail beds have been invaded
by the fungus, leading to chronic hyperkeratosis and subungual
accumulation of friable keratinaceous debris. (Courtesy of the
Department of Dermatology, Wilford Hall USAF Medical Center and
Brooke Army Medical Center, San Antonio, TX.)
|
|
Differential Diagnosis
Psoriasis and various other nail
dystrophies, such as distal onycholysis caused by excessive water
exposure or drugs, must be differentiated from this fungal infection.
Pseudomonal nail infection is characterized by the subungual accumulation
of green debris. A KOH examination of the keratinaceous debris
demonstrating hyphae confirms onychomycosis.
Emergency Department Treatment
and Disposition
The most common treatment
consists of oral griseofulvin, fluconazole, lucenazole, or terbinafine.
Candidal infections require oral ketoconazole. Toenail onychomycosis is
very difficult to eradicate.
Clinical Pearls
1. All that causes the nail
plate to separate from the nail bed is not necessarily fungus.
2. Distal subungual is the most
common type of onychomycosis.
|
|
Tinea Versicolor
Associated Clinical Features
Tinea versicolor is a chronic,
superficial fungal infection that involves the trunk and extremities with
little or no involvement of the face. The fungus is part of normal skin
flora. Finely scaling brown macules are present in fair-skinned patients
(Fig. 13.34), whereas scaly hypopigmented macules are often noted in the
dark-skinned (Fig. 13.35). These sharply demarcated macules are
intermittently pruritic.
|
|
|

|
|
Tinea
Versicolor This chronic
superficial fungal infection leads to the formation of multiple
well-defined, scaly brown macules on the trunk and extremities.
(Courtesy of the Department of Dermatology, Wilford Hall USAF Medical
Center and Brooke Army Medical Center, San Antonio, TX.)
|
|
|
|
|

|
|
Tinea
Versicolor An example of
hypopigmented areas on dark skin. (Courtesy of James J. Nordlund,
MD.)
|
|
Differential Diagnosis
Pityriasis rosea, secondary
syphilis, and some drug eruptions must all be considered in the
differential diagnosis. A KOH examination of a scraping of the area
revealing hyphae and spores makes the diagnosis (see Fig. 21.16).
Emergency Department Treatment
and Disposition
Treatment consists of short
applications of selenium sulfide lotion, topical antifungal creams, or
topical ketoconazole. Resistant cases require oral ketoconazole.
Ultraviolet exposure is required to regain any lost pigment.
Clinical Pearls
1. Tinea versicolor is more
common in adolescents and young adults.
2. Clinically active areas or
areas colonized with the fungus may be identified by orange fluorescence
noted on Wood's light examination.
|
|
Basal Cell Carcinoma
Associated Clinical Features
Basal cell carcinoma is a
malignancy of the basal cell layer of the epidermis, presenting as a
translucent, pearly papule with central ulceration and rolled borders
with fine superficial telangiectasias (Fig. 13.36). It is most frequently
located on the head, neck, and upper trunk. The patient frequently notes
easy bleeding of the papule with poor to nonhealing. There are several
variants of basal cell carcinomas. Pigmented basal cell carcinoma consists
of a brownish-black, firm nodule with irregular surface and central
ulceration (Fig. 13.37). Superficial multicentric basal cell carcinoma is
psoriasiform in nature, consisting of a flat, erythematous, scaly
translucent plaque without central ulceration or raised border (Fig.
13.38).
|
|
|

|
|
Basal
Cell Carcinoma Nodular basal
cell carcinoma consists of a firm, centrally ulcerated (rodent ulcer)
nodule with a raised, rolled, pearly, telangiectatic border.
(Courtesy of the Department of Dermatology, Wilford Hall USAF Medical
Center and Brooke Army Medical Center, San Antonio, TX.)
|
|
|
|
|
|
|
Pigmented
Basal Cell Carcinoma This
pigmented basal cell carcinoma consists of a firm, translucent,
brownish-black ulcerated nodule with an irregular surface and
asymmetry of its border. (Courtesy of the Department of Dermatology,
Wilford Hall USAF Medical Center and Brooke Army Medical Center, San
Antonio, TX.)
|
|
|
|
|

|
|
Basal
Cell Carcinoma A superficial
multicentric basal cell carcinoma is frequently psoriasiform in
nature. Note the flat, erythematous, scaly plaque with its elevated,
irregular border. (Courtesy of the Department of Dermatology, Wilford
Hall USAF Medical Center and Brooke Army Medical Center, San Antonio,
TX.)
|
|
Differential Diagnosis
Pigmented basal cell carcinoma
resembles nodular melanoma. Superficial multicentric basal cell carcinoma
resembles psoriasis, tinea corporis, and squamous cell carcinoma in situ.
Emergency Department Treatment
and Disposition
Excisional surgery, cryosurgery,
or electrosurgery are recommended forms of treatment. If there is a
potential for disfigurement, radiation therapy is usually instituted
instead of surgery. Prompt dermatologic consultation must be arranged
when evaluating any suspicious lesion. Up to half of patients will
develop a recurrence.
Clinical Pearls
1. Basal cell carcinoma is the
most common form of skin cancer.
2. This malignancy forms in the
epidermis that has developing hair follicles; therefore, it is not found
on the vermilion border of the lips or the genital mucosal membranes.
3. The pearly, rolled,
telangiectatic border with central ulceration is diagnostic of basal cell
carcinoma.
4. Despite being locally
invasive, basal cell carcinoma does not metastasize.
|
|
Squamous Cell Carcinoma
Associated Clinical Features
Squamous cell carcinoma varies
from erythematous, hyperkeratotic, sharply demarcated plaques to
elevated, ulcerative nodules (Fig. 13.39). It may be sun-induced or
related to ionizing radiation or industrial carcinogens. Invasive
squamous cell carcinoma is characterized by a discrete elevated plaque or
nodule with thick keratotic scale and ulceration.
|
|
|

|
|
Squamous
Cell Carcinoma Note the single
erythematous, scaly plaque on the dorsal aspect of this sun-exposed
hand. (Courtesy of the Department of Dermatology, Wilford Hall USAF
Medical Center and Brooke Army Medical Center, San Antonio, TX.)
|
|
Differential Diagnosis
Squamous cell carcinoma must be
differentiated from a benign lesion such as tinea corporis, psoriasis,
impetigo, wart, seborrheic keratosis, or keratoacanthoma (Fig. 13.40).
|
|
|

|
|
Keratoacanthoma This rapidly evolving neoplasm consists of an
erythematous nodule with a hyperkeratotic core. It most closely
resembles a squamous cell carcinoma although it is a benign
epithelial neoplasm. Biopsy serves to differentiate these two
conditions. (Courtesy of the Department of Dermatology, Wilford Hall
USAF Medical Center and Brooke Army Medical Center, San Antonio, TX.)
|
|
Emergency Department Treatment
and Disposition
Excisional surgery is required,
with radiation therapy utilized in potentially disfiguring cases. All
suspicious lesions require prompt dermatologic consultation.
Clinical Pearls
1. Squamous cell carcinoma is
the second most common type of skin cancer.
2. This malignancy develops
more commonly in fair-skinned people with a significant history of sun
exposure.
3. Most lesions are found on
the lips or other sun-exposed areas.
4. A rapidly evolving (2 to 4
weeks) nodule or plaque with a dense hyperkeratotic core is a
keratoacanthoma. It is closely related to squamous cell carcinoma and frequently
occurs at a site of trauma. Treatment is the same.
5. Risk of metastasis is
related to size, location, and histology.
|
|
Melanoma
Associated Clinical Features
Melanoma is a malignancy
involving the melanocytes of the epidermis. Asymmetry, an irregular
border, a mottled display of color, a diameter greater than 5 to 6 mm,
and an elevation or distortion of the surface are five signs that a
lesion may be a melanoma (Fig. 13.41). Melanoma may or may not occur in
sun-exposed areas.
|
|
|

|
|
Melanoma Note the asymmetry, irregular border, and
focal hyperpigmentation in this melanoma. (Courtesy of the Department
of Dermatology, Wilford Hall USAF Medical Center and Brooke Army
Medical Center, San Antonio, TX.)
|
|
Differential Diagnosis
Lentigo maligna is characterized
by a single, flat, freckle-like macule with an irregular border, usually
on the face (Fig. 13.42). This melanoma in situ is often confused with a
solar lentigo or a seborrheic keratosis and has about a 5% risk of being
malignant. Superficially spreading melanoma is the most common form of
melanoma. It usually presents as a brown macule with irregular borders and
variegation in color. Nodular melanoma usually starts as a papule which
becomes an elevated nodule with irregular borders and variegation in
color (Fig. 13.43). It must be differentiated from a hemangioma,
angiokeratoma, or pigmented basal cell carcinoma. Acral lentiginous
melanomas, which are agressive and metastasize easily, are often mistaken
for plantar warts or subungual hematomas; they are flat, pigmented,
irregularly bordered macules of the palms, soles, and subungual areas
(Fig. 13.44).
|
|
|

|
|
Lentigo
Maligna Melanoma This
long-lived melanoma in situ has now invaded the dermis, forming a
black nodule classified as lentigo maligna melanoma. (Courtesy of the
Department of Dermatology, Wilford Hall USAF Medical Center and
Brooke Army Medical Center, San Antonio, TX.)
|
|
|
|
|

|
|
Nodular
Melanoma This melanoma has
progressed to an exophytic tumor, which was deeply invasive
histopathologically. (Courtesy of the Department of Dermatology,
Wilford Hall USAF Medical Center and Brooke Army Medical Center, San
Antonio, TX.)
|
|
|
|
|

|
|
Acral
Lentiginous Melanoma The
finding of a pigmented, irregularly bordered macule involving the
proximal nail fold is called Hutchinson's sign. It represents
melanoma of the nail matrix and is therefore classified as an acral
lentiginous melanoma. (Courtesy of the Department of Dermatology,
Wilford Hall USAF Medical Center and Brooke Army Medical Center, San
Antonio, TX.)
|
|
Emergency Department Treatment
and Disposition
A melanoma must be surgically
excised with adequate margins. Prompt dermatologic consultation is
required of all suspicious lesions, because the prognosis of melanoma
correlates directly with early detection and treatment.
Clinical Pearls
1. Prognosis of melanoma is
most dependent on the depth of invasion, therefore, early detection and
treatment are essential.
2. Only 20% of melanomas arise
from preexisting moles, so the appearance of a new mole, especially after
the age of 30, is particularly significant.
3. Most benign moles have
symmetry, one color, and are less than 7 mm in diameter.
|
|
Pyogenic Granuloma
Associated Clinical Features
Pyogenic granuloma is
characterized by a solitary, violaceous, pedunculated or sessile vascular
nodule which usually forms at the site of cutaneous injury (Fig. 13.45).
The well demarcated nodule consists of exuberant granulation tissue
("proud flesh") which may be erosive and encrusted. Pyogenic
granuloma commonly occurs on the digits and is particularly common in
pregnancy.
|
|
|

|
|
Pyogenic
Granuloma This solitary,
violaceous, pedunculated, vascular nodule formed at the site of an
injury. Note that the nodule is well demarcated by a thin rim of
epidermis. (Courtesy of the Department of Dermatology, Wilford Hall
USAF Medical Center and Brooke Army Medical Center, San Antonio, TX.)
|
|
Differential Diagnosis
This benign vascular neoplasm
resembles a hemangioma; however, it must be differentiated from
amelanotic melanoma, squamous cell carcinoma, and metastatic renal cell
carcinoma.
Emergency Department Treatment
and Disposition
Since this neoplasm usually does
not resolve spontaneously, it may be shaved off with electrodessication
of the base.
Clinical Pearls
1. A fine collarette of scale
surrounding an exophytic vascular neoplasm is diagnostic.
2. The lesion may exhibit
recurrent bleeding episodes.
3. Nearly 25 to 33% of these
benign lesions follow some form of minor trauma.
|
|
Fixed Drug Eruption
Associated Clinical Features
A fixed drug eruption is a
cutaneous reaction to an ingested drug, usually an over-the-counter
laxative, barbiturate, tetracycline, or sulfa drug. The reaction occurs
at the identical site with repeated exposure to the same drug, usually on
the genital skin or proximal extremity. It presents as a round, pruritic,
erythematous, sharply demarcated plaque that may evolve into a painful
bulla with secondary erosion (Fig. 13.46). Residual hyperpigmentation
frequently follows healing.
|
|
|

|
|
Fixed
Drug Eruption This red to
violaceous, pruritic, sharply demarcated patch is a cutaneous
reaction to a drug. Repeated exposure will cause a similar reaction
in the same location. (Courtesy of the Department of Dermatology,
Wilford Hall USAF Medical Center and Brooke Army Medical Center, San
Antonio, TX.)
|
|
Differential Diagnosis
Early cellulitis, erythema
multiforme, arthropod assault, and genital herpes are usually considered
in the differential diagnosis.
Emergency Department Treatment
and Disposition
The etiology must be identified
and removed before the plaque will resolve. Symptomatic treatment
includes antihistamines and analgesics.
Clinical Pearls
1. The identical recurrence of
a painful, pruritic, well-demarcated violaceous plaque makes the
diagnosis.
2. This reaction occurs with
repeated exposure to the same drug.
3. Some patients have a
refractory period following exposure.
|
|
Exanthematous Drug Eruptions
Associated Clinical Features
Exanthematous drug eruptions are
an adverse hypersensitivity reaction to a drug. This symmetric, pruritic,
morbilliform, blanching, erythematous eruption is the most frequent of
cutaneous drug eruptions (Fig. 13.47). The initially pruritic macules or
papules usually become confluent and may progress to an exfoliative
dermatitis.
|
|
|

|
|
Exanthematous
Drug Eruption This symmetric,
morbilliform, blanching eruption may eventually become confluent,
leading to an exfoliative dermatitis. (Courtesy of GlaxoWellcome
Pharmaceuticals.)
|
|
Differential Diagnosis
Viral exanthem, secondary
syphilis, atypical pityriasis rosea, and scarlet fever must all be
considered in the differential diagnosis. A serologic test for syphilis,
antistreptolysin O titer, and a good history are usually sufficient to
make the diagnosis. Severe drug eruptions may be accompanied by
eosinophilia, lymphadenopathy, and liver function abnormalities.
Emergency Department Treatment
and Disposition
The eruption may resolve despite
the drug's continued use. The drug should be discontinued if considered
to be the cause of the rash. It may take as long as 2 weeks for the eruption
to fade after discontinuation of the causative drug. Symptomatic
management includes antihistamines and topical corticosteroids.
Clinical Pearls
1. Drug eruptions are usually
symmetric and pruritic as opposed to viral eruptions, which are usually
asymmetric and asymptomatic.
2. Mononucleosis patients
taking amoxicillin or AIDS patients taking sulfa drugs frequently
experience this reaction.
|
|
Erythema Nodosum
Associated Clinical Features
Erythema nodosum is a delayed
hypersensitivity reaction, usually to certain drugs, infections, or
systemic illnesses. This panniculitis (inflammation of the fat) consists
of painful, nonulcerated, poorly marginated nodules with overlying
erythematous, warm, shiny skin. (Fig. 13.48). The lower legs are the most
common site; the face is rarely involved. Fever, malaise, and arthralgias
often accompany the cutaneous manifestations.
|
|
|

|
|
Erythema
Nodosum These multiple painful
nodules with overlying erythematous, warm and shiny skin were
associated with coccidioidomycosis and are typical of erythema
nodosum. (Courtesy of GlaxoWellcome Pharmaceuticals.)
|
|
Differential Diagnosis
Erythema induratum, syphilitic
gummas, and nodular vasculitis are considered in the differential
diagnosis.
Emergency Department Treatment
and Disposition
Identify and treat the underlying
etiology. Oral contraceptives, sulfa drugs, tuberculosis, sarcoidosis, fungal
infections, and inflammatory bowel disease are common predisposing
factors. Symptomatic treatment includes nonsteroidal anti-inflamatory
drugs (NSAIDs), bed rest, and compressive dressings.
Clinical Pearls
1. Erythema nodosum most
commonly presents in young women secondary to oral contraceptives or
sulfa drugs.
2. Its appearance in
association with systemic fungal infections (coccidioidomycosis)
indicates a likely recovery from the disease.
|
|
Urticaria and Angioedema
Associated Clinical Features
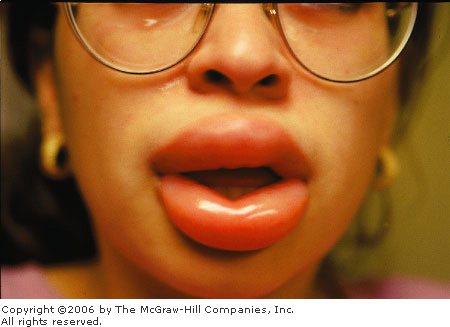
Urticaria, a vascular reaction
localized to the skin, is composed of transient, erythematous, edematous,
pruritic papules or plaquelike wheals (Figs. 13.49, 13.50). It tends to
favor the covered areas (back, chest, buttocks). Angioedema comprises
thicker plaques that result from fluid shift into the dermis and
subcutaneous tissues. It generally affects the distensible tissues (lips,
eyelids, earlobes, Fig. 13.51) and is usually nonpruritic. There are
countless causes of urticaria; the most common being food, medications,
and underlying infection. Cholinergic urticaria involves micropapular
lesions induced by exercise or heat. Dermatographism presents as linear
hives at the site of skin stroking. Cold urticaria (Fig. 13.52) can be
diagnosed with the ice cube test, and solar urticaria occurs in areas
exposed to sunlight. Urticaria may also occur as a result of exposure to
pressure, heat, and water. Hereditary angioedema is an autosomal dominant
disorder with systemic manifestations secondary to edema of the subcutaneous
and mucosal tissues of the respiratory and gastrointestinal tract in
addition to the face and extremities. Mortality rates approach 30%,
usually from airway obstruction. There is also an acquired form of
angioedema secondary to an underlying malignancy, usually
lymphoreticular. The use of angiotensin converting enzyme (ACE)
inhibitors is a frequent cause of angioedema.
|
|
|

|
|
Urticaria Note the edematous papules and wheals covering
the skin of the neck. (Courtesy of Alan B. Storrow, MD.)
|
|
|
|
|

|
|
Urticaria Note the classic raised plaques on the lower
extremity of this patient with urticaria. (Courtesy of James J.
Nordlund, MD.)
|
|
|
|
|
|
|
Angioedema Prominent lip involvement in a young woman
with ACE inhibitor–induced angioedema. (Courtesy of Alan B.
Storrow, MD.)
|
|
|
|
|

|
|
Cold
Urticaria Plaque formation
after placement of an ice cube on the skin confirms cold urticaria.
(Courtesy of James J. Nordlund, MD.)
|
|
Differential Diagnosis
Bacterial or viral exanthems,
erythema multiforme, and drug eruptions must be considered in the
differential diagnosis of urticaria. Edema of any etiology (congestive
heart failure, glomerulonephritis, chronic liver disease) must be
differentiated from the soft tissue swelling associated with angioedema.
Emergency Department Treatment
and Disposition
This involves the identification
and elimination of any potential etiology. Antihistamines can be
effective for urticaria, often requiring both H1 and H2
blockers and steroids for stubborn cases. Life-threatening attacks of
hereditary angioedema do not respond well to antihistamines, epinephrine,
or steroids. Admission for supportive care and active airway management
is the mainstay of treatment. Danazol may be utilized for prophylactic
management.
Clinical Pearls
1. Both urticaria and
angioedema are acute and evanescent.
2. Urticaria is pruritic and
responsive to antihistamines, epinephrine, and steroids.
3. Angioedema is only rarely
pruritic and minimally responsive to epinephrine; it may require danazol
for long-term treatment.
4. Doxepin may be considered
for refractory cases due to its potent H1 and H2
blocking effect.
|
|
Dyshidrotic Eczema (Pompholyx)
Associated Clinical Features
Dyshidrotic eczema is a
papulovesicular plaque involving the epidermis of the fingers, palms, and
soles. The dermatosis initially consists of pruritic, deep-seated
vesicles grouped in clusters (Fig. 13.53). Scaling and painful fissure
formation are late complications, as is secondary bacterial infection.
Spontaneous remissions and recurrent attacks are usually the rule. The
bullous form is called pompholyx.
|
|
|

|
|
Dyshidrotic
Eczema Note the cluster of
deep-seated vesicles along the sides of the fingers. Scaling and
painful fissure formation may also occur. No overlying erythema is
present. (Courtesy of the Department of Dermatology, Wilford Hall
USAF Medical Center and Brooke Army Medical Center, San Antonio, TX.)
|
|
Differential Diagnosis
Acute contact dermatitis must be
considered in the differential diagnosis of the acute eruption. Psoriasis
and dermatophytosis are considered in the differential diagnosis of the chronic
eruption.
Emergency Department Treatment
and Disposition
Burow's wet dressings should be
utilized during the early vesicular stage. High-potency topical steroids
are used in all stages of the eruption. Systemic corticosteroids should
be avoided except for the most severe cases. Antihistamines treat the
pruritus. Dicloxacillin or erythromycin are used to treat secondary
bacterial infections. Minimal exposure to water and generous emolliation
also hasten healing.
Clinical Pearls
1. Deep-seated, tapioca-like
vesicles on the sides of the digits, followed by scaling and fissure
formation, are typically seen in this disease.
2. Dyshidrotic eczema is
frequently associated with psychosocial stressors.
3. The "id reaction,"
due to fungal infections and drug eruptions, may have similar clinical
presentations.
|
|
Atopic Dermatitis
Associated Clinical Features
Atopic dermatitis is a broadly
defined pruritic inflammation of the epidermis and dermis, with
approximately 60% of the cases occurring during the first year of life.
The characteristic pattern is erythema, papules, and lichenified plaques
with excoriation and exudation of wet crusts (Fig. 13.54). Its
distribution is the face (sparing of the mouth), the antecubital and
popliteal fossae, and the dorsal surfaces of the forearms, hands, and
feet. This is generally considered a lifelong condition with gradual
improvement toward adulthood.
|
|
|

|
|
Atopic
Dermatitis Lichenfied plaques,
erosions, and fissures are characteristic of atopic dermatitis.
(Courtesy of James J. Nordlund, MD.)
|
|
Differential Diagnosis
Nummular eczema, allergic contact
dermatitis, impetigo, dermatophytosis, and psoriasis are usually
considered in the differential diagnosis. A KOH examination of the scale
rules out dermatophytosis. A biopsy may help differentiate this condition
from nummular eczema and contact dermatitis.
Emergency Department Treatment
and Disposition
Antihistamines treat the
pruritus. Unscented emollients prevent xerosis (dry skin). Topical
corticosteroids treat the underlying inflammation. Systemic
corticosteroids should be avoided except for the most severe cases. Since
these patients are frequently colonized with Staphylococcus aureus,
antistaphylococcal antibiotics are also used during flares of the
condition.
Clinical Pearls
1. Scaly plaques on the
flexural surface with excoriation and exudation of crusts is diagnostic
of atopic dermatitis.
2. Asthma and allergic rhinitis
may develop as the atopic dermatitis improves.
|
|
Nummular Eczema
Associated Clinical Features
Nummular eczema is a pruritic,
eczematous dermatitis consisting of closely grouped vesicles that
coalesce into coin-shaped, erythematous plaques with poorly defined
borders (Fig. 13.55). These plaques may become encrusted or dry and
scaly. They are usually found on the trunk and extremities (especially
the hand) of a middle-aged or elderly patient.
|
|
|

|
|
Nummular
Eczema An example of multiple
erythematous, coin-shaped plaques with fine scales, representative of
this pruritic, eczematous dermatitis. (Courtesy of the Department of
Dermatology, Wilford Hall USAF Medical Center and Brooke Army Medical
Center, San Antonio, TX.)
|
|
Differential Diagnosis
Allergic contact dermatitis,
impetigo, dermatophytosis, and psoriasis must all be considered in the
differential diagnosis. If it scales, scrape it and look for hyphae to
differentiate a dermatophytosis. A biopsy may help differentiate contact
dermatitis from nummular eczema.
Emergency Department Treatment
and Disposition
Antihistamines treat the pruritus.
Unscented emollients prevent xerosis. Topical corticosteroids treat the
underlying inflammation. Systemic corticosteroids should be avoided
except for the most severe cases.
Clinical Pearls
1. Coin-shaped, pruritic,
eczematous plaques not responsive to antibiotics are diagnostic of
nummular eczema.
2. Recurrences tend to appear
in previously involved sites.
|
|
Allergic Contact Dermatitis
Associated Clinical Features
Allergic contact dermatitis is an
acute or chronic delayed-type hypersensitivity reaction caused by contact
exposure to a variety of agents. The acute form is characterized by
multiple, closely grouped vesicles with exudative erosions and crust
formation on a well defined erythematous, edematous base (Fig. 13.56).
Subacute contact dermatitis consists of dry, scaly patches with areas of
desquamation, whereas the chronic form consists of hyperkeratosis and
pigmentation. All forms of allergic contact dermatitis are pruritic.
|
|
|

|
|
Contact
Dermatitis Note that the
erythematous, edematous base of the eruption corresponds to the
posterior surface of the watch. Superimposed on the erythematous base
are multiple vesicles with exudate and crust. (Courtesy of the
Department of Dermatology, Wilford Hall USAF Medical Center and
Brooke Army Medical Center, San Antonio, TX.)
|
|
Differential Diagnosis
Atopic dermatitis, nummular
eczema, impetigo, and dermatophytosis are included in the differential
diagnosis. If it scales, scrape it and look for hyphae to differentiate a
dermatophytosis. A positive patch test is diagnostic of an allergic
contact dermatitis. Contact exposure of the skin to the allergen leading
to erythema and vesicle formation is considered a positive test.
Emergency Department Treatment
and Disposition
Identify and remove any potential
allergen. Antihistamines relieve the pruritus. Topical corticosteroids
treat the underlying inflammation. Systemic corticosteroids should be
avoided except for the most severe cases.
Clinical Pearls
1. Well-defined, pruritic areas
of erythema superimposed on exudative vesicles and a recent history of
exposure to a specific allergen are diagnostic of allergic contact dermatitis.
2. Poison ivy and oak are the
most common causes of allergic contact dermatitis.
3. In treating dermatitis with
topical ointments, worsening may signify an allergic reaction to the
medication.
|
|
Phytophotodermatitis and Drug-Induced Photosensitivity
Associated Clinical Features
Phytophotodermatitis is a
pruritic, linear dermatitis that occurs when skin exposed to certain
plants becomes exposed to sunlight. Bizarre patterns of pruritic erythema
convert into vesicles and bullae that undergo involution, leaving behind
a residual intense hyperpigmentation (Fig. 13.57).
|
|
|

|
|
Phytophotodermatitis This linear, photodistributed, eczematous
plaque resulted from contact with a plant-derived photosensitizer
(lime juice). This frequently resolves with hyperpigmentation.
(Courtesy of the Department of Dermatology, Wilford Hall USAF Medical
Center and Brooke Army Medical Center, San Antonio, TX.)
|
|
Drug-induced photosensitivity is an adverse skin
reaction due to simultaneous exposure to certain drugs and ultraviolet
radiation. The rash is erythematous and edematous, much like sunburn
(Fig. 13.58).
|
|
|

|
|
Drug-Induced
Photosensitivity Erythematous
reaction to ultraviolet radiation associated with carbamazepine use.
(Courtesy of the Department of Dermatology, Naval Medical Center,
Portsmouth, VA.)
|
|
Differential Diagnosis
Rhus dermatitis is most often
mistaken for this eruption. Photosensitivity can be caused by other
diseases.
Emergency Department Treatment
and Disposition
Symptomatic treatment includes
wet dressings, antihistamines, calamine lotion, and corticosteroid
creams. For drug-induced photosensitivity, the offending drug should be
discontinued. Counsel patients about the use of sunscreens and sun
avoidance to prevent recurrences.
Clinical Pearls
1. Linearly distributed,
pruritic vesicles in a photodistribution with a history of plant exposure
make the diagnosis.
2. The distribution of the rash
is limited to sun-exposed areas.
3. Common drugs causing
drug-induced photosensitivity are carbamazepine, amiodarone, doxycycline,
furosemide, phenothiazines, and sulfonamides.
|
|
Pemphigus Vulgaris
Associated Clinical Features
Pemphigus vulgaris is a bullous
autoimmune disease of the skin and mucous membranes caused by IgG
autoantibodies. Previously, mortality was high, but now it only occurs in
10% of cases, usually secondary to steroid complications. This disease
typically affects middle-aged adults. Vesicles and bullae arise on the
skin of the scalp, chest, umbilicus, and intertriginous areas (Fig.
13.59).
|
|
|

|
|
Pemphigus
Vulgaris Classic
vesiculobullous lesions of pemphigus vulgaris throughout the chest
and abdomen. (Courtesy of James J. Nordlund, MD.)
|
|
Differential Diagnosis
Pemphigus vulgaris must be
distinguished from all other bullous diseases by a skin biopsy.
Emergency Department Treatment
and Disposition
High-dose steroids are the
mainstay of therapy. Other immunosuppressives—such as azathioprine,
methotrexate, and cyclophosphamide—can be helpful. Plasmapheresis
is used in cases resistant to standard treatment.
Clinical Pearls
1. Nikolsky's sign can be
seen—dislodging of the epidermis with lateral finger pressure on
the edge of the bulla.
2. Ulcers and erosions of the
oral mucosa are the presenting sign in up to 90% of patients.
|
|
Vitiligo
Associated Clinical Features
Vitiligo is an acquired loss of
pigmentation that commonly involves the backs of the hands, the face, and
body folds (Fig. 13.60). There is a positive family history in 30% of the
cases. Initially the disease is limited, but it then slowly progresses
over years. Vitiligo is secondary to absence of epidermal melanocytes,
which may be due to an autoimmune phenomenon against melanocytes.
Approximately half of these cases begin in patients less than 20 years of
age.
|
|
|

|
|
Vitiligo Note the hypopigmented areas characteristic of
vitiligo. (Courtesy of James J. Nordlund, MD.)
|
|
Differential Diagnosis
Vitiligo must be differentiated
from tinea versicolor (which has scale and a positive KOH scraping), postinflammatory
hypopigmentation, leprosy, and pityriasis alba.
Emergency Department Treatment
and Disposition
Vitiligo requires referral to a
dermatologist for PUVA (psoralen plus ultraviolet A), topical therapy, or
skin grafting. The best results from therapy occur on the face and neck.
Clinical Pearls
1. Vitiligo occurs at sites of
trauma (Koebner's phenomenon).
2. Wood's lamp examination
helps identify hypopigmented areas in patients with light complexions.
3. Tinea versicolor has a scale
and positive KOH prep.
|
|
Scabies and Norwegian Scabies
Associated Clinical Features
Transmission of scabies occurs
after direct skin contact with an infected individual and possibly from
clothing and bedding infested with the mite. The female mite burrows into
the individual's skin and deposits two to three eggs daily. Fecal pellets
(scybala) are also deposited in the burrow and may be responsible for the
localized pruritus. Nocturnal pruritus is characteristic of scabies. The
pink-white, slightly elevated burrows (Fig. 13.61) are typically found in
the web spaces of the hands and feet, penis, buttocks, scrotum, and
extensor surfaces of the elbows and knees. Norwegian scabies (Fig. 13.62)
tends to cause asymptomatic crusting—rather than the typical
inflammatory papules and vesicles—as well as nail dystrophy and
keratosis.
|
|
|

|
|
Scabies A burrow on the heel of a pediatric patient with
scabies. (Courtesy of Briana Hill, MD.)
|
|
|
|
|

|
|
Norwegian
Scabies Gray scales and
crusting consistent with Norwegian scabies. In these patients, many
thousands (versus a few dozen) mites are present. (Courtesy of Lynn
Utecht, MD.)
|
|
Differential Diagnosis
Infestation by lice, eczema, and
insect bites can be confused with scabies.
Emergency Department Management
and Disposition
Topical permethrin or lindane are
commonly used to treat scabies. Each of these products should be applied
thoroughly and then, after 8 to 12 h washed from the skin. Lindane should
be avoided during infancy and pregnancy because of reports of infant
neurotoxicity following systemic absorption through the skin.
Clinical Pearls
1. Ivermectin given as a single
200-mg/kg dose or a 5% sulfur ointment can also be used for treatment.
2. Oral antipruritic therapy
and analgesics will help alleviate discomfort.
3. Intimate contacts and all
family members in the same household should be treated.
|
|
Cutaneous Larva Migrans
Associated Clinical Features
Cutaneous larva migrans (CLM)
presents as a serpiginous, red, raised, wavy rash that is approximately 3
mm wide (Fig. 13.63). The lacy rash is moderately to severely pruritic as
a result of larval secretion of proteolytic enzymes. Infection is most
frequent in warmer climates and occurs when the ova of adult hookworms
penetrate the skin of a person walking in contaminated soil. Symptoms
begin days to weeks after infestation. The nematodes prefer to infect
cats or dogs; humans are infected accidentally. The goal of the larva is
to eventually penetrate the intestines of its prey. However, owing to
physiologic limitations in humans, penetration deeper than the basal
layer of the epidermis is prevented.
|
|
|

|
|
Cutaneous
Larva Migrans Note the
elevated tracks caused by migration of the larva through the
epidermis. (Courtesy of the Department of Dermatology, National Naval
Medical Center, Bethesda, MD.)
|
|
Differential Diagnosis
The appearance of CLM and its
associated pruritus can resemble an allergic reaction, but the lacy
border usually distinguishes it.
Emergency Department Treatment
and Disposition
Topical application of
thiabendazole is the treatment of choice. It is applied two or three
times per day for a total of 5 days. Thiabendazole is also available in
an oral form; however, it is less effective. Albendazole is an
alternative. Symptoms should improve in 48 h. Untreated CLM will usually
resolve in 2 to 8 weeks.
Clinical Pearls
1. Löffler's syndrome can occur
in patients with severe CLM infestation. In this condition, larval
invasion of the bloodstream is manifest as a patchy infiltrate of the
lung and eosinophilia of the blood and sputum.
2. The larval track represents
an allergic reaction; the larva itself stays slightly ahead of the track.
3. Freezing the skin with ethyl
chloride is a simple, effective treatment used in endemic areas.
|
|
Uremic Frost
Associated Clinical Features
Uremic frost is a classic
manifestation of chronic renal failure; it is rarely seen today. It
develops as a result of accumulation of urea in sweat. In advanced
uremia, the accumulation of urea in sweat may reach such a critical level
that, upon its evaporation, a fine white powder is left on the skin
surface (Fig. 13.64). Associated hyperkalemia may also be present owing
to renal failure.
|
|
|
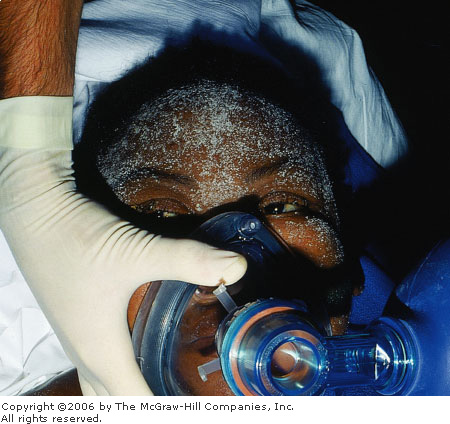
|
|
Uremic
Frost Note the fine white
powder on the skin of this patient with end-stage renal disease.
(Courtesy of Richard C. Levy, MD.)
|
|
Differential Diagnosis
Dried sweat from a patient with
cystic fibrosis forms fern-like crystals that may resemble this
condition. In an individual without known renal disease, uremic frost may
be mistaken for a dermatologic problem or chemical exposure. However, in
a patient with known end-stage renal disease, the differential of a white
precipitate on the skin surface is limited.
Emergency Department Management
and Disposition
Treatment of the underlying
condition that resulted in the patient's uremia may prevent further
accumulation of uremic frost. Typically, urgent dialysis is indicated.
Clinical Pearls
1. Although rare today, this
condition may be seen in patients without adequate air conditioning who
are poorly controlled on dialysis.
2. For patients presenting with
altered mental status, attention to the airway, oxygenation, and rapid
assessment and treatment of associated metabolic disorders such as
hyperkalemia are indicated.
|
|
Bacillus Anthracis (Anthrax)
Associated Clinical Features
Anthrax is usually a disease of
herbivores; humans are infected when they come into contact with infected
animals or contaminated animal products. Recently, anthrax has received
increased international attention as a potential biological warfare
agent. There are three distinct clinical manifestations of anthrax.
Cutaneous anthrax accounts for
about 95% of human cases. After direct contact on exposed skin, the
infection begins as a pruritic papule. It enlarges into an ulcer
surrounded by vesicles in 1 to 2 days and then eventually becomes a
characteristic black, necrotic central eschar surrounded by nonpitting
edema (Fig. 13.65). Systemic manifestations (fever, hypotension,
tachycardia) may accompany cutaneous involvement.
|
|
|
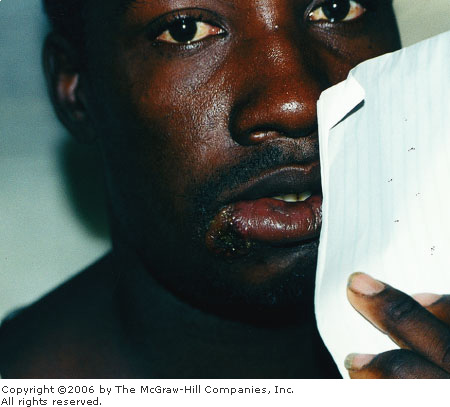
|
|
Anthrax Note the early ulcer of cutaneous anthrax on
the right of the lower lip. (Courtesy of Thea James, MD.)
|
|
Respiratory anthrax (woolsorters'
disease) occurs after exposure to anthrax spores and presents as an upper
respiratory infection. Within 1 to 4 days, the disease progresses to
severe respiratory distress, hypoxia and hypotension. Death uniformly
occurs within 24 h after the onset of the fulminant phases of the
infection.
Gastrointestinal anthrax is rare
and occurs 3 to 7 days after exposure to contaminated animal meat.
Initially it presents as a nonspecific gastroenteritis with fever,
vomiting, diarrhea, and malaise. The disease then progresses to
hematemesis, bloody diarrhea, sepsis and shock. Death usually occurs 2 to
5 days after symptom onset.
Differential Diagnosis
Cutaneous anthrax resembles
staphylococcal infection, tularemia, and plague. Inhalation and
gastrointestinal anthrax may initially be similar to a viral upper
respiratory infection or gastroenteritis, respectively.
Emergency Department Treatment
and Disposition
Admission is indicated for
patients with anthrax. Intravenous penicillin is the primary treatment
for all forms. Ciprofloxacin or doxycycline are alternatives. Oral
ciprofloxacin is recommended for postexposure prophylaxis.
Clinical Pearls
1. Gastrointestinal and
inhalation anthrax are almost uniformly fatal, even with antibiotic
therapy.
2. Human killed vaccine is
available and recommended for mill workers and veterinarians at high risk
for exposure.
3. The virulence of anthrax is
derived from its edema toxin, lethal toxin, and capsular material.
4. A classic pathologic finding
for inhalation anthrax is hemorrhagic mediastinitis; this may be
manifested on chest radiography as a widened mediastinum.
5. Decontamination of suspected
anthrax spore exposure consists of removal of exposed clothing (place in
a sealed plastic bag) and washing of the exposed area with soap and
water.
|
|
Acknowledgments
The author acknowledges
Christopher R. Sartori, MD, and Michael B. Brooks, MD, for portions of
this chapter written for the first edition of this book.
|
|