|
Note: Large images and
tables on this page may necessitate printing in landscape mode.
Copyright
©2006 The McGraw-Hill Companies. All rights reserved.
Emergency
Medicine Atlas > Chapter 14. Pediatric
Conditions > Newborn Conditions >
|
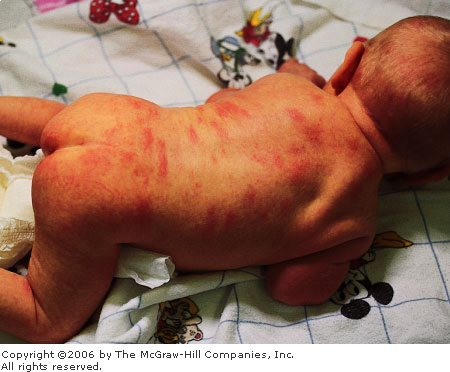
Erythema Toxicum
Associated Clinical Features
This benign, self-limited
eruption of unknown etiology in newborns is characterized by small,
erythematous macules 2 to 3 cm in diameter (Fig. 14.1) with 1- to 3-mm
firm pale yellow or white papules or pustules in the center. This rash
usually presents within the first 2 to 3 days of life. Each individual
lesion usually disappears within 4 or 5 days. New lesions may occur
during the first 2 weeks of life. Wright-stained slide preparations of
the scraping from the center of the lesion demonstrate numerous
eosinophils.
|
|
|
|
|
Erythema
Toxicum Newborn infant with
diffuse macular rash of erythema toxicum. (Courtesy of Kevin J.
Knoop, MD, MS.)
|
|
Differential Diagnosis
Transient neonatal pustular
melanosis, newborn milia, miliaria, herpes simplex, and impetigo of the
newborn should be considered.
Emergency Department Treatment
and Disposition
As this condition is
self-limiting, no therapy is indicated in the setting of a well-appearing
newborn with normal activity and appetite. In cases where impetigo, Candida,
or herpes infections are suspected, a smear from the center of the lesion
and culture may be necessary to make a final diagnosis.
Clinical Pearl
1. Erythema toxicum is the most
common rash of the newborn (up to 50% of full terms). The lesions may be
present anywhere on the body but tend to spare the palms and soles.
|
|
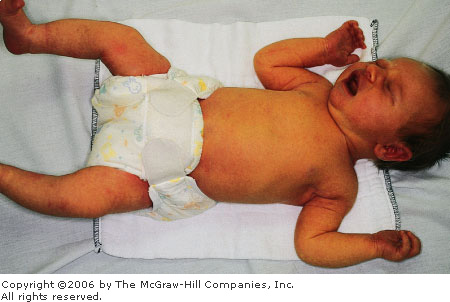
Salmon Patches (Nevus Simplex)
Associated Clinical Features
Nevus simplex (salmon patches) is
the most common vascular lesion in infancy, present in about 40% of
newborns. It is described as a slightly red, flat, macular lesion on the
nape of the neck, the glabella, forehead, or upper eyelids (Figs. 14.2
and 14.3). In general, the eyelid lesions fade within a year and the
glabellar within 5 to 6 years. The lesions on the neck often persist.
|
|
|

|
|
Salmon
Patches Newborn with
characteristic salmon patches over his face. (Courtesy of Anne W.
Lucky, MD.)
|
|
|
|
|

|
|
Salmon
Patches Child with patch over
lower back consistent with salmon patches. (Courtesy of Anne W.
Lucky, MD.
|
|
Differential Diagnosis
Nevus flammeus (port-wine stain)
can have a similar appearance.
Emergency Department Treatment
and Disposition
Parental education and
reassurance can be helpful, but no treatment is indicated.
Clinical Pearls
1. In general, flat, vascular
birthmarks tend to persist through life. Raised vascular birthmarks
usually disappear with time.
2. When this lesion is seen on
the nape of the neck, it is frequently referred to as a stork bite.
|
|
Neonatal Jaundice
Associated Clinical Features
Physiologic jaundice (Fig. 14.4)
is observed in 25 to 50% of term newborns. Most cases are self-limited
and generally without sequelae. The physiologic (<12 mg/dL) jaundice
of the newborn usually peaks between the second and fourth day. In
preterm infants, this peak occurs later. Physiologic jaundice is believed
to be due to a combination of factors including an increase of bilirubin
production following a breakdown of fetal red blood cells associated with
a temporary decrease in conjugation of these by-products by the immature
newborn liver. Risk factors for unconjugated hyperbilirubinemia include
maternal diabetes, prematurity, drugs, polycythemia, traumatic delivery
with cutaneous bruising or hematoma, and breast-feeding. Most infants with
jaundice have no disease, but a careful history and organized approach is
necessary to identify pathologic causes when these patients present to
the ED. Kernicterus is a condition resulting from a severe form of
unconjugated hyperbilirubinemia and is associated with mental
retardation, deafness, seizures, choreoathetosis, and a multitude of
other irreversible neurologic abnormalities.
|
|
|
|
|
Neonatal
Jaundice Newborn with
yellowish hue to skin consistent with jaundice. (Courtesy of Kevin J.
Knoop, MD, MS.)
|
|
Differential Diagnosis
Jaundice within the first 24 h of
life is usually associated with sepsis, erythroblastosis fetalis, and
bleeding disorders or hemorrhage (traumatic delivery with cutaneous
bleeding or hematomas). Physiologic jaundice first appears on the second
or third day. Any patient presenting with jaundice after the third day of
life should be carefully evaluated for the possibility of sepsis.
Late-onset jaundice could be suggestive of septicemia, breast milk
jaundice, galactosemia, hemolytic anemias, drug-induced
hyperbilirubinemia, pyloric stenosis or duodenal atresia, Crigler-Najjar
syndrome, or Gilbert's disease.
Emergency Department Treatment
and Disposition
Initial laboratory workup should
include blood type and Coombs' test, complete blood count with smear for
red cell morphology and reticulocyte count, and indirect and direct
bilirubin. Other studies may be ordered according to the clinical
presentation and history. Initial management should ensure adequate
hydration and treatment of the underlying condition. Acidosis should be
corrected, since bilirubin precipitates in acid media. In cases of physiologic
jaundice, the level of serum bilirubin at which to start phototherapy is
not clearly defined. The traditional approach is to initiate phototherapy
to maintain bilirubin level below 20 mg/dL. Exchange transfusion is
considered if the serum level remains elevated (22 to 28 mg/dL) despite
appropriate phototherapy.
Clinical Pearls
1. Physiologic jaundice in the
presence of a good hemoglobin level is orange in color. It is often
visible when the bilirubin level exceeds 8 mg/dL. Jaundice associated
with anemia is usually lemon in color.
2. Bilirubin levels should be
modified for prematurity, sepsis, low birth weight, and other risk
factors when phototherapy or exchange transfusion is considered.
|
|
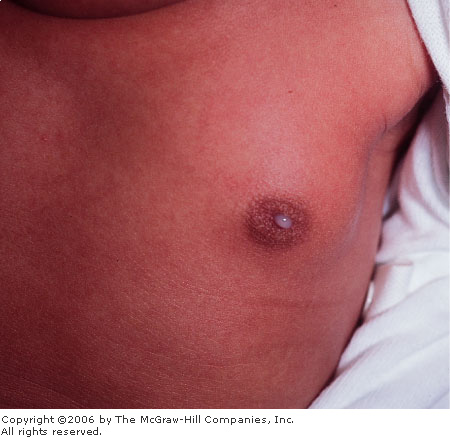
Neonatal Milk Production (Witch's Milk)
Associated Clinical Features
Because of transplacental
hormonal effects (maternal estrogens and possibly endogenous prolactin),
both sexes are equally liable to develop enlarged breasts. This
phenomenon occurs with or without galactorrhea in 60% of normal newborns.
After the first 48 h, the hypertrophied breasts may become engorged, and
a form of lactation occurs (Fig. 14.5). The engorgement and edema begin
to subside after the second week of life. The hypertrophy and
galactorrhea may persist up to 6 months in girls. These infants are
occasionally predisposed to infections (mastitis or abscess).
|
|
|
|
|
Witch's
Milk Milky fluid draining from
the nipple in a newborn. (Courtesy of Michael J. Nowicki, MD.)
|
|
Differential Diagnosis
Early mastitis with purulent
discharge may resemble normal neonatal milk production.
Emergency Department Treatment
and Disposition
Treatment is not necessary; reassurance
for parents is very important.
Clinical Pearl
1. Newborns with hypertrophied
mammary tissue and evidence of clear colostrum-like secretion in the
absence of erythema, tenderness, and/or fluctuation usually do not
present with neonatal mastitis.
|
|
Neonatal Mastitis
Associated Clinical Features
Neonatal mastitis is most common
in full-term females, particularly in their second or third week of life.
Clinically it manifests as swelling, induration, and tenderness of the
affected breast with or without erythema or warmth (Fig. 14.6). In some
cases purulent discharge may be obtained from the nipple. Bacteremia and
fever are rare. This infection is usually caused by Staphylococcus
aureus, coliform bacteria, or group B streptococcus. If treatment is
delayed, mastitis may progress rapidly with involvement of subcutaneous
tissues and subsequent toxicity and systemic findings.
|
|
|

|
|
Neonatal
Mastitis Neonate with
left-sided breast swelling, erythema, and purulent discharge.
(Courtesy of Raymond C. Baker, MD.)
|
|
Differential Diagnosis
In the initial stages, neonatal
mastitis may mimic mammary tissue hypertrophy owing to maternal passive
hormonal stimulation. Minor trauma, cutaneous infections, and duct
blockage may precede this infection.
Emergency Department Treatment
and Disposition
Institution of treatment is
important to avoid cellulitic spread and breast tissue damage. In cases
of mild cellulitis and no fluctuation, culture of nipple discharge and
antibiotic coverage (semisynthetic penicillin or first-generation
cephalosporins) completes the treatment. Adjustment of coverage may be
done once results of cultures or Gram's stain are available, especially
in the presence of gram-negative bacilli. If no organism is seen
initially, semisynthetic penicillin and an aminoglycoside or cefotaxime
should be used. In case of toxicity or subcutaneous spreading, a complete
sepsis workup should be performed, and hospitalization is usually
indicated. In cases of palpable fluctuation, prompt surgical incision and
drainage should be performed by a surgeon to avoid further damage of the
mammary tissue. Recovery is usually in 5 to 7 days.
Clinical Pearl
1. Consider mastitis in the
neonate with edema, induration, and tenderness of the breast tissue.
Erythema and fluctuation to palpation ensue if treatment is delayed.
|
|
Umbilical Cord Granuloma
Associated Clinical Features
Umbilical cord granuloma develops
in response to a mild infection at the base of the umbilical cord caused
by saprophytic organisms. Usually parents describe a persistent discharge
from the base of the cord. The granuloma is soft, pink, and vascular
(Fig. 14.7) and is the result of persistence of exuberant granulation
tissue.
|
|
|

|
|
Umbilical
Cord Granuloma Newborn infant
with umbilical cord demonstrating granuloma on base of umbilical
cord. (Courtesy of Michael J. Nowicki, MD.)
|
|
Differential Diagnosis
An umbilical polyp is a rare
anomaly resulting from the persistence of the omphalomesenteric duct
(Figs. 14.8, 14.9) or the urachus and may have a similar appearance. This
polyp is usually firm and resistant, with a mucoid secretion. Omphalitis,
an infection secondary to gram-negative organisms, should be considered.
|
|
|

|
|
Omphalomesenteric
Duct This red mass resembling
a granuloma was found to be an omphalomesenteric duct. (Courtesy of
Kevin J. Knoop, MD, MS.)
|
|
|
|
|

|
|
Fistulogram A fistulogram confirms the diagnosis of
persistent omphalomesenteric duct. (Courtesy of Kevin J. Knoop, MD,
MS.)
|
|
Emergency Department Treatment
and Disposition
Cleaning and drying of the
umbilical cord base with alcohol several times a day may prevent
granuloma formation. Cauterization of the granuloma with silver nitrate
is the treatment of choice. It is important to protect the surrounding skin
to avoid chemical burns produced by the excess of silver nitrate.
Clinical Pearls
1. Commonly the only sign of
granuloma formation is the presence of nonpurulent discharge noted in the
diaper area in contact with the umbilicus.
2. Omphalitis presents with
redness on the abdominal wall and often with a purulent discharge from
the umbilicus.
|
|
Hypertrophic Pyloric Stenosis (HPS)
Associated Clinical Features
HPS is characterized by
postprandial, nonbilious vomiting due to hypertrophy and hyperplasia of the
pyloric musculature, producing gastric outlet obstruction. It is usually
diagnosed in infants from birth to 5 months, most commonly at 2 to 8
weeks of life. The vomiting progresses to forceful and is described as
projectile (although this pattern is not always present). There is a
familial incidence, and white males are more frequently affected. During
the physical examination, peristaltic waves may be observed traveling
from the left upper to right upper quadrants (Fig. 14.10). The
hypertrophy and hyperplasia of the antral and pyloric musculature
produces the "olive" to palpation (best palpated after emptying
the stomach with a nasogastric tube). Because of persistent vomiting,
hypochloremic alkalosis with various degrees of dehydration and failure
to thrive may occur when this is not diagnosed early. The finding of the
pyloric olive is pathognomonic. Ultrasound and fluoroscopy are useful
diagnostic tools to confirm the diagnosis when the olive is not evident.
|
|
|

|
|

|
|

|
|
Gastric
Wave of Hypertrophic Stenosis
A gastric wave can be seen traversing the abdomen in this series of
photographs of a patient with HPS. (Courtesy of Kevin J. Knoop, MD,
MS.)
|
|
Differential Diagnosis
Intestinal obstruction, atresia,
malrotation with volvulus, hiatal hernia, gastroenteritis, adrenogenital
syndrome, increased intracranial pressure, esophagitis, sepsis,
gastroesophageal reflux, and poor feeding technique should be considered.
Emergency Department Treatment
and Disposition
Once the diagnosis is considered,
treatment includes correction of fluids and electrolyte imbalance
followed by surgical referral for curative pylorotomy. Patients benefit
from a nasogastric tube on low intermittent suction.
Clinical Pearls
1. Any infant in the first 2
months of life who presents with postprandial vomiting, some evidence of
failure to gain weight, easy refeeding, hunger after vomiting, and
infrequent bowel movements should be carefully evaluated to rule out the
possibility of HPS.
2. Clinical suspicion can be
heightened with serial examinations and observation of the child after
oral fluid challenges for persistent projectile vomiting.
3. Correction of any
electrolyte imbalance should occur prior to surgery.
|
|
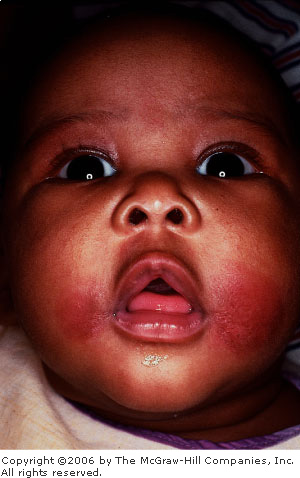
Erythema Infectiosum (Fifth Disease)
Associated Clinical Features
Erythema infectiosum is a viral
infection caused by parvovirus B19. It is characterized by an eruption
that presents initially as an erythematous malar blush followed by an
erythematous maculopapular eruption on the extensor surfaces of
extremities that evolves into a reticulated, lacy, mottled appearance
(Fig. 14.11). It may present with low-grade fever, malaise, general
aches, arthritis, or arthralgias.
|
|
|

|
|
Fifth
Disease Toddler with the
classic slapped-cheek appearance of fifth disease caused by
parvovirus B19. Also note the lacy reticular macular rash on the
shoulder and upper extremity. (Courtesy of Anne W. Lucky, MD.)
|
|
Differential Diagnosis
Morbilliform eruptions may be
caused by viruses such as measles, rubella, roseola, and infectious
mononucleosis. Bacterial infections (i.e., scarlet fever), drug
reactions, and other skin conditions such as guttate psoriasis, papular
urticaria, and erythema multiforme are included in the differential.
Emergency Department Treatment
and Disposition
There is no specific treatment.
Once the rash appears, the patient is no longer contagious. It is
important to educate the patient and family about the possible risk of
B19 virus as a cause of hydrops fetalis or fetal deaths early in
pregnancy and the issue of an aplastic crisis in patients with
hematologic problems such as sickle cell disease, hereditary
spherocytosis, other hemolytic anemias, or immunosuppressed host.
Clinical Pearl
1. Classically this infection
begins with the intense redness of both cheeks ("slapped-cheek
appearance"). Although the eruption tends to disappear within 5 days
of the initial presentation, recrudescences may occur with exercise,
overheating, and sunburns as a result of cutaneous vasodilatation.
|
|
Roseola Infantum (Exanthem Subitum)
Associated Clinical Features
The typical presentation of
roseola infantum is that of a child with a 2- or 3-day history of fever
and irritability. This is followed by rapid defervescence and the
appearance of an erythematous morbilliform eruption (Fig. 14.12). It has
been associated with various viral agents such as parvovirus, echovirus,
and other enteroviruses. Most recently it has been associated with
herpesvirus 6.
|
|
|

|
|
Roseola
Infantum (Exanthem Subitum)
Toddler with maculopapular eruption of roseola. (Courtesy of Raymond
C. Baker, MD.)
|
|
Differential Diagnosis
Morbilliform eruptions may be
caused by common viruses such as measles, rubella, parvovirus B19, or
infectious mononucleosis. Bacterial infections (e.g., scarlet fever),
drug reactions, and other skin conditions such as guttate psoriasis,
papular urticaria, and erythema multiforme may be included in the
differential.
Emergency Department Treatment
and Disposition
As with most viral infections,
only supportive therapy is necessary. Special attention should be paid in
maintaining fluid intake, fever control for the patient's comfort, and
parental education about the benign, self-limiting characteristics of
this illness.
Clinical Pearls
1. The presence of mild eyelid
edema with posterior cervical adenopathy in the febrile child without a
source may be early indicators for the diagnosis of roseola. Once the
fever ends and the rash appears, the diagnosis is clinically confirmed.
2. Rashes during the febrile
course of an illness are not roseola.
|
|
Impetigo
Associated Clinical Features
Impetigo is a bacterial infection
of the skin produced by Streptococcus pyogenes and Staphylococcus
aureus. It begins as small vesicles or pustules with very thin roofs
that rupture easily with the release of a cloudy fluid and the subsequent
formation of a honey-colored crust (Figs. 14.13, 14.14). Often the
lesions spread rapidly and coalesce to form larger ones.
|
|
|

|
|
Impetigo Young girl with crusting impetiginous lesions
on her chin. (Courtesy of Michael J. Nowicki, MD.)
|
|
|
|
|

|
|
Bullous
Impetigo A child with
impetiginous lesions on the face. Note the formation of bullae.
(Courtesy of Anne W. Lucky, MD.)
|
|
Differential Diagnosis
Second-degree burns, cutaneous
diphtheria, herpes simplex infections, nummular dermatitis, and kerion
may present with crusts and be confused with impetigo.
Emergency Department Treatment
and Disposition
Since these lesions are
contagious, good hand washing and personal hygiene should be discussed
with the patient and family. Antibiotic coverage should be directed
against the organisms mentioned above. Effective oral agents include
erythromycin, first-generation cephalosporins, cloxacillin, or
amoxicillin with clavulanic acid. Topical agents such as mupirocin
ointment have proved to be as effective as oral antibiotics.
Clinical Pearls
1. A red, weeping surface and
the presence of moist, thin vesicles with honey-colored crusts makes the
diagnosis of impetigo.
2. Inflicted cigarette burns
may resemble the lesions of impetigo.
|
|
Kerion
Associated Clinical Features
A kerion consists of inflammatory
boggy nodules with pustules caused by an exaggerated host delayed
hypersensitivity response to infections with either Microsporum canis
or Trichophyton tonsurans. These lesions usually remain localized
to one area (Fig. 14.15). It appears 2 to 8 weeks after the initial
fungal infection and resolves over 4 to 6 weeks. If untreated, scarring
and hair loss may occur.
|
|
|

|
|
Kerion Occipital boggy swelling with hair loss
consistent with kerion. (Courtesy of Anne W. Lucky, MD.)
|
|
Differential Diagnosis
Bacterial pyoderma is commonly
mistaken for kerion but yields a purulent discharge when aspirated. The
diagnosis should be made on clinical appearance.
Emergency Department Treatment
and Disposition
Topical agents have no role in
the treatment of tinea capitis or kerion. Griseofulvin for 4 to 6 weeks
is the treatment of choice. Ketoconazole has also been used. Viable
spores can be eradicated by adding selenium sulfide shampoo (2.5%) to
this therapy. In cases of severe inflammatory reaction, prednisone
combined with griseofulvin ensures a rapid resolution of the infection
and immunogenic reaction. Incision should be avoided to prevent scar
tissue.
Clinical Pearl
1. If a kerion happens to be
aspirated or incised, only serosanguineous fluid is obtained.
|
|
Varicella (Chickenpox)
Associated Clinical Features
Chickenpox results from a primary
infection with varicella virus and is characterized by a generalized
pruritic vesicular rash (Fig. 14.16), fever, and mild systemic symptoms.
The skin lesions have an abrupt onset, develop in crops, and evolve from
papules to vesicles (rarely bullae) and finally to crusted lesions within
48 h. The classic lesions are teardrop vesicles surrounded by an
erythematous ring (dewdrop on a rose petal) (Fig. 14.17). Secondary
bacterial infection of these lesions can occur, causing cellulitis, which
may be severe. Other complications from varicella include encephalitis,
pancreatitis, hepatitis, pneumonia, arthritis, or meningitis. Cerebritis
(ataxia) may develop and is usually self-limiting.
|
|
|

|
|
Varicella
(Chickenpox) Multiple
umbilicated cloudy vesicles of varicella. (Courtesy of Lawrence B.
Stack, MD.)
|
|
|
|
|

|
|
Varicella
(Chickenpox) Vesicles in
different stages of maturation. Note the clear vesicle on an
erythematous base ("dewdrop in a rose petal") in the center
of the chest. (Courtesy of Judith C. Bausher, MD.)
|
|
Differential Diagnosis
Although several illnesses can
present with vesiculobullous lesions, the typical case of varicella is
seldom confused with other problems. Common viral infections that
manifest with vesicular rashes include herpes simplex, herpes zoster,
coxsackie, influenza, and echovirus infections or vaccinia. On occasion
varicella can be confused with papular urticaria.
Emergency Department Treatment
and Disposition
Most patients do not develop any
complications. Treatment should be symptomatic and directed to pruritus
and fever control (avoid salicylates because of their association with
Reye's syndrome). Oral acyclovir given within 24 h of the onset of the
illness may result in a modest decrease in the duration of symptoms and
in the number and duration of skin lesions. Acyclovir is not recommended
routinely for treatment of uncomplicated varicella in an otherwise
healthy child. In the immunocompromised host, VZIG (varicella zoster
immunoglobulin) and intravenous acyclovir are effectively used.
Clinical Pearl
1. Skin lesions in varicella
present in successive crops, so that papules, vesicles, and crusted
lesions may all be present at the same time. The earliest lesions may
begin at the hairline on the nape of the neck.
|
|
Measles
Associated Clinical Features
Measles presents as an acute
febrile illness with a 3- to 4-day prodromal period characterized by
cough, coryza, and conjunctivitis associated with fever (101° to 104°F),
chills, and malaise. Koplik's spots, the pathognomonic sign of measles,
appear as 1- to 3-mm white elevations on the buccal mucosa (Fig. 14.18).
They usually present 1 to 2 days before the development of the
characteristic erythematous maculopapular rash. This rash appears during
the third or fourth day of the illness. It usually begins around the
hairline, behind the earlobes, and spreads downward (Fig. 14.19). It
tends to fade in the same order it appears. Most cases recover without
complications; others may develop otitis media, croup, pneumonia,
encephalitis, and rarely subacute sclerosing panencephalitis (SSPE), a
very late complication.
|
|
|

|
|
Koplik's
Spots Tiny white dots
(Koplik's spots) are seen on the buccal mucosa. (Courtesy of Lawrence
B. Stack, MD.)
|
|
|
|
|

|
|
Measles School-age child with a morbilliform rash on
his face consistent with measles. (Courtesy of Javier A. Gonzalez del
Rey, MD.)
|
|
Differential Diagnosis
The differential diagnosis of the
characteristic rash is vast and includes exanthem subitum; rubella;
infections caused by echovirus, coxsackie and adenoviruses;
toxoplasmosis; infectious mononucleosis; scarlet fever; Kawasaki disease;
drug reactions; Rocky Mountain spotted fever; and meningococcemia.
Emergency Department Treatment
and Disposition
Supportive therapy includes bed
rest, antipyretics, and adequate fluid balance. Complications should be
treated according to the presentation. Current available antiviral
compounds are not effective. The use of gamma globulins and steroids in
SSPE is limited. Passive immunization is effective for prevention and
attenuation of measles if given within 5 days of the initial exposure.
During outbreaks, measles-mumps-rubella (MMR) vaccine is given earlier
than 15 months and may need to be repeated. A second dose is recommended
after the primary series for those born after 1956. This is given at age
11 or 12 years or by entry to junior high school.
Clinical Pearls
1. The classic presentation
includes a prodromal phase (fever, hacking cough, coryza, and
conjunctivitis), Koplik's spots followed by an abrupt temperature rise,
and a rash spreading in a caudal distribution.
2. Examination of the oral
mucosa to identify Koplik's spots may diagnose measles early if performed
in all children with an acute febrile illness.
|
|
Hand, Foot, and Mouth Disease
Associated Clinical Features
Hand, foot, and mouth disease is
a seasonal (summer–fall) viral infection caused by coxsackievirus
A16. It is characterized by fever, malaise, and anorexia over 1 to 2
days, followed by oral lesions (small, red macules that evolve into small
vesicles 1 to 3 mm in diameter) in the posterior oropharynx (Fig. 14.20).
This enanthem is then followed by a superficial, nonloculated vesicular
eruption on the hands and feet (3 to 7 mm) (Figs. 14.21 and 14.22). These
may also be present on the buttocks, face, and legs.
|
|
|

|
|
Hand,
Foot, and Mouth Disease
Discrete vesicular erosions on the posterior oropharynx and soft
palate secondary to coxsackievirus. (Courtesy of James F. Steiner,
DDS.)
|
|
|
|
|

|
|
Hand,
Foot, and Mouth Disease
Erythematous vesicular rash scattered on the palms, consistent with
coxsackievirus. (Courtesy of Michael J. Nowicki, MD.)
|
|
|
|
|

|
|
Hand,
Foot, and Mouth Disease
Vesicular rash of the feet consistent with coxsackievirus. (Courtesy
of Raymond C. Baker, MD.)
|
|
Differential Diagnosis
Herpes simplex, varicella,
varicella zoster, influenza, echovirus infections, vaccinia, and other
coxsackieviruses should all be considered.
Emergency Department Treatment
and Disposition
Supportive therapy, especially
fluid maintenance and fever control for the patient's comfort, is the
mainstay of treatment. The duration and characteristics of the illness
should be discussed with the parents. In the majority of cases, the
course is self-limited and the prognosis excellent. On rare occasions,
secondary complications such as myocarditis, pneumonia, and
meningoencephalitis may occur.
Clinical Pearl
1. The individual lesions are
usually seen on the palms, fingertips, and soles. Oral cavity lesions
appear as discrete oval erosions and most are classically seen in the
posterior oropharynx and soft palate.
|
|
Cold Panniculitis (Popsicle Panniculitis)
Associated Clinical Features
Cold panniculitis is an acute
cold injury to the fat of the cheeks in infants. It manifests as red,
indurated nodules and plaques on exposed skin, especially the face (Fig.
14.23). These lesions appear 1 to 3 days after exposure and gradually
soften and return to normal over 1 or more weeks. This phenomenon is
caused by subcutaneous fat solidification when exposed to low
temperature. It is more frequent in children than in adults.
|
|
|
|
|
Cold
Panniculitis Infant with cheek
erythema, swelling, and discoloration consistent with popsicle
panniculitis or cold injury. (Courtesy of Anne W. Lucky, MD.)
|
|
Differential Diagnosis
Facial cellulitis, trauma,
pressure erythema, giant urticaria, and contact dermatitis may have a
similar presentation.
Emergency Department Treatment
and Disposition
Treatment is not necessary;
parental reassurance is very important.
Clinical Pearl
1. Because these lesions may
also be painful, the differentiation of cold panniculitis from cellulitis
may be difficult on occasion. The absence of systemic symptoms,
especially fever, and the history of cold exposure are very suggestive of
cold panniculitis.
|
|
Herpetic Gingivostomatitis
Associated Clinical Features
Herpetic gingivostomatitis is a
viral infection commonly seen in infants and children; it is caused by
herpes simplex. Patients usually present with fever, malaise, cervical
adenopathy, and pain in the mouth and throat on attempting to swallow.
Vesicular and ulcerative lesions appear throughout the oral cavity. The
gingiva becomes very friable and inflamed, especially around the alveolar
rim. Increased salivation with foul breath may be present. Although fever
disappears in 3 to 5 days, children may have difficulty eating for 7 to
14 days. Sometimes, autoinoculation produces vesicular lesions on the
fingers (herpetic whitlow) (Fig. 14.24).
|
|
|

|
|
Herpetic
Gingivostomatitis Multiple
oral vesicular lesions consistent with herpes gingivostomatitis.
Vesicular lesions from autoinoculation are present on the finger
(herpetic whitlow). (Courtesy of Michael J. Nowicki, MD.)
|
|
Differential Diagnosis
Vincent's angina, aphthous
stomatitis, erythema multiforme, Behçet's disease, and other viral
infections such as herpangina and hand, foot, and mouth disease
(coxsackieviruses) should be considered.
Emergency Department Treatment
and Disposition
No specific treatment is
available. In immunocompromised patients, acyclovir should be considered.
In the normal host, fluid balance should be maintained throughout the
illness. Because of ulcerative lesions, avoidance of citrus juices or
spicy food prevents pain on swallowing. Clear fluids, ice pops, and ice
cream may be used in small children. Not infrequently, admission for
intravenous hydration is necessary. Adequate fever control is also necessary
for patient comfort and to avoid an increase in fluid losses. Pain
control may be achieved by using mixtures of antihistamine
(diphenhydramine elixir) and antacids (1:1) applied to lesion with
Q-tips. In small children, local application of viscous lidocaine
(Xylocaine) should be avoided, since patients may develop toxic plasma
levels due to an altered absorption from an inflamed oral mucosa.
Clinical Pearl
1. Most of these lesions are in
the anterior two-thirds of the oral cavity. Posterior lesions sparing the
gingiva are most commonly seen in coxsackievirus infections.
|
|
Urticaria
Associated Clinical Features
Urticaria is a localized,
edematous skin reaction from histamine release that usually follows an
infection, insect sting or bite, ingestion of certain foods, or
medications. It is characterized by a sudden onset of pruritic,
transient, well-circumscribed wheals scattered over the body. These are
flat-topped and may vary from pinpoint size to several centimeters in
diameter. They usually have a central clearing and peripheral extension
and can have tense edema (Fig. 14.25). Most urticarial reactions last 24
to 48 h; on rare occasions, they may take weeks to resolve. Rarely, there
may be systemic reactions such as wheezing, stridor, or angioedema.
|
|
|

|
|

|
|
Urticaria Preschool child with annular, raised pruritic
lesions with the central clearing and tense edema of polycyclic
urticaria. The lesions had completely disappeared after about 5 min.
(Courtesy of Kevin J. Knoop, MD, MS.)
|
|
Differential Diagnosis
Erythema multiforme, arthropod
bites, dermatographism, contact dermatitis, reactive erythemas, allergic
vasculitis, juvenile rheumatoid arthritis, mastocytosis, and pityriasis
rosea can all present with a similar-appearing rash.
Emergency Department Treatment
and Disposition
Treatment is symptomatic. Oral
antihistamines are useful in the control of pruritus. If a systemic
reaction is also part of the initial presentation, epinephrine and
steroids should be added to the therapy. In most cases it is very
difficult to identify the etiologic factor. Unless there is evidence of
acute angioedema, most cases can be discharged home on oral
antihistamines.
Clinical Pearl
1. Erythema multiforme can be
commonly mistaken for polycyclic urticaria (multiple red wheals of
different sizes). Clinicially these two entities can be differentiated by
the duration and color of the lesions. In urticaria, the center is clear
and each lesion usually lasts a few hours. In erythema multiforme, the
center is dusky and the lesion remains in the same place for several days
to weeks.
|
|
Staphylococcal Scalded Skin Syndrome
Associated Clinical Features
Staphylococcal scalded skin
syndrome is caused by a staphylococcal toxin-producing strain. It may
present with fever, malaise, and irritability following an upper
respiratory infection. Patients develop a diffuse faint erythematous rash
that becomes tender to touch. Crusting around the mouth, eyes, and neck
is not uncommon. Within 2 to 3 days, the upper layers of dermis may be
easily removed; finally a flaccid bulla develops with subsequent
exfoliation of the skin (Fig. 14.26). In young patients, this exfoliation
may involve a large surface area with significant fluid and electrolyte
losses.
|
|
|

|
|

|
|
Staphylococcal
Scalded Skin Syndrome Toddler
with diffuse macular peeling eruption consistent with scalded skin
syndrome from Staphylococcus aureus. (Courtesy of Judith C.
Bausher, MD.)
|
|
Differential Diagnosis
Toxic epidermal necrolysis,
exfoliative erythroderma, bullous erythema multiforme, bullous
pemphigoid, bullous impetigo, sunburn, acute mercury poisoning, toxic
shock syndrome, and scarlet fever should be considered.
Emergency Department Treatment
and Disposition
Treatment is directed at the
eradication of Staphylococcus, thus terminating the production of toxin.
Synthetic penicillins should be used intravenously. Admission is usually
necessary, especially in young infants. This age group requires careful
attention to fluid and electrolyte losses and the prevention of secondary
infection of the affected skin.
Clinical Pearl
1. The wrinkling or peeling of
the upper layer of the epidermis (pressure applied with a Q-tip or gloved
finger) that occurs within 2 or 3 days of the onset of this illness is
known as Nikolsky's sign.
|
|
Meningococcemia
Associated Clinical Features
Meningococcemia is an acute
febrile illness with generally rapid onset of marked toxicity, purpura,
and petechiae (Fig. 14.27). It progresses rapidly to hypotension with
multisystem failure. In cases of fulminant disease, this shock stage is
accompanied by disseminated intravascular coagulation and massive mucosal
hemorrhages. Occasionally there may be a specific prodrome with upper
respiratory infection and malaise.
|
|
|

|
|
Meningococcemia Diffuse petechiae in a patient with
meningococcemia. (Courtesy of Richard Straight, MD.)
|
|
Differential Diagnosis
Gonococcemia, Haemophilus
influenzae infection, pneumococcemia, Rocky Mountain spotted fever,
sepsis with thrombocytopenia or disseminated intravascular coagulation
(DIC), endocarditis, Henoch-Schönlein purpura, typhoid fever, leukemia,
hemorrhagic measles, or hemorrhagic varicella may have a similar
appearance.
Emergency Department Treatment
and Disposition
In stable patients in whom the
diagnosis of meningococcemia is entertained, cultures of blood, spinal
fluid, nasopharynx, complete blood count, platelet count, and coagulation
studies should be obtained. Consider arterial blood gas, liver function
tests, and other studies as indicated. These patients should be admitted
for close monitoring to institutions capable of delivering critical care
services. Broad-spectrum parenteral antibiotics should be used in the
initial coverage until the organism is identified and sensitivities are
available. In the unstable septic patient, adequate ventilation and
cardiac function must be ensured in addition to performing the above tests
and treatment. Hemodynamic monitoring and support (fluids and vasoactive
drugs) are of paramount importance in the management. Peripheral and
central venous catheters and urinary and arterial catheters are usually
necessary for optimal care of these patients.
Clinical Pearls
1. Skin scrapings of the
purpuric lesion can be microscopically examined for the presence of
gram-negative diplococci and may be cultured for organisms.
2. A child with a fever and a
petechial rash must be presumed to have meningococcemia.
|
|
Scarlet Fever
Associated Clinical Features
Scarlet fever manifests itself as
erythematous macules and papules that result from an erythrogenic toxin
produced by a group A streptococcus. The most common site for invasion by
this organism is the pharynx and occasionally skin or perianal areas. The
disease usually occurs in children (2 to 10 years of age) and less
commonly in adults. The typical presentation of scarlet fever includes
fever, headache, sore throat, and malaise followed by the scarlatiniform
rash (Fig. 14.28). The rash is typically erythematous; it blanches (in
severe cases may include petechiae), and—owing to the grouping of
the fine papules—gives to the skin a rough, sandpaper-like texture
(Fig. 14.29). On the tongue, a thick, white coat and swollen papillae
give the appearance of a strawberry ("strawberry tongue").
|
|
|

|
|
Scarlatina Erythematous scarlatiniform rash of scarlet
fever. (Courtesy of Lawrence B. Stack, MD.)
|
|
|
|
|

|
|
Sandpaper
Rash Typical sandpaper rash of
scarlet fever. The grouping of the fine papules gives the skin a
rough, sandpaper-like texture. (Courtesy of Jeffery S. Gibson, MD.)
|
|
Differential Diagnosis
A similar syndrome is caused by
staphylococci producing an exfoliative exotoxin, which can be
differentiated from the streptococcal infection because of the absence of
pharyngitis, strawberry tongue, and negative cultures. Enteroviral
infections, viral hepatitis, infectious mononucleosis, toxic shock
syndrome, drug eruptions, rubella, mercury intoxication, and
mucocutaneous lymph node syndrome should be considered.
Emergency Department Treatment
and Disposition
Penicillin, either benzathine
penicillin G or oral penicillin, to maintain levels for 10 days is the
key to therapy. Alternatives include erythromycin or clindamycin in
penicillin-allergic patients.
Clinical Pearls
1. Petechiae (commonly found as
part of the scarlatiniform eruption) in a linear pattern seen along the
major skin folds in the axillae and antecubital fossa are known as
"Pastia's lines" (Fig. 14.30).
2. In black skin, the rash may
be difficult to differentiate and may consist only of punctate papular
elevations called "goose flesh."
|
|
|

|
|

|
|
Pastia's
Lines Confluent petechia in a
linear pattern in the antecubital fossa consistent with Pastia's
lines are seen in these patients with scarlet fever. Top: The forearm
on the right belongs to the patient's sister and does not show
Pastia's lines. Bottom: Pastia's lines in a Caucasian patient. A
classic sandpaper rash is also evident on the arm and trunk.
(Courtesy of Stephen Corbett, MD.)
|
|
|
|
Blistering Distal Dactylitis
Associated Clinical Features
Blistering distal dactylitis is a
cellulitis of the fingertips (Fig. 14.31) caused by beta-hemolytic
streptococcal and, in rare occasions, by Staphylococcus aureus
infections. The typical lesion is a fluid-filled, tense blister with
surrounding erythema located over the volar fat pad on the distal portion
of the fingers. Polymorphonuclear leukocytes and gram-positive cocci can
be found in the Gram's stain of the purulent exudate from the lesion.
|
|
|

|
|
Blistering
Distal Dactylitis Blistering
rash of the distal fingers with surrounding erythema typically caused
by Streptococcus. Note the location of the rash over the volar
finger pad. (Courtesy of Anne W. Lucky, MD.)
|
|
Differential Diagnosis
Bullous impetigo, burns, friction
blisters, and herpetic whitlow should be considered.
Emergency Department Treatment
and Disposition
There is usually a rapid response
to incision and drainage of the blister and a 10-day course of antibiotic
therapy (dicloxacillin, cephalexin, or erythromycin).
Clinical Pearl
1. This diagnosis should be
entertained in any child presenting with a tender, cloudy, fluid-filled
blister of the fingertips or toes.
|
|
Strawberry Hemangioma
Associated Clinical Features
Strawberry hemangioma often
appears as small telangiectatic papules or a patch surrounded by an area
of pallor. These lesions grow and become vascularized during the first 2
months of life. The classic lesion is a raised gray to reddish nodule
with defined borders (Fig. 14.32). It commonly regresses in almost all patients
by 2 to 3 years of age. In a few cases, very large vascular lesions can
cause platelet trapping or high-output cardiac failure. Localized
hemangiomas can affect the airway, eyes, or other areas where they occur.
|
|
|

|
|
Strawberry
Hemangioma Raised umbilicated
vascular lesion on the right forehead consistent with strawberry
hemangioma. (Courtesy of Anne W. Lucky, MD.)
|
|
Differential Diagnosis
Malignant vascular tumors,
pyogenic granulomas, and giant melanocytic birthmarks should be
considered.
Emergency Department Treatment
and Disposition
Most cases require no therapy
because strawberry hemangiomas usually regress without residua. Treatment
is indicated when there is an obstruction of a vital orifice (i.e.,
airway, mouth, or nares) or vision (eyelids) or if hematologic or
cardiovascular complications are present. Parental reassurance is
important because there is great pressure to treat for cosmetic reasons.
Steroids, liquid nitrogen, grenz-ray therapy, and pulse dye laser are
some of the different therapeutic modalities used in its treatment. In
complex cases, dermatologic consultation is recommended.
Clinical Pearl
1. The diagnosis of strawberry
hemangioma should always be considered in the presence of any purplish,
red, raised, tumorlike lesion not present at birth that appears in the
first month of life.
|
|
Orbital and Periorbital (Preseptal) Cellulitis
Associated Clinical Features
Orbital cellulitis is a serious
bacterial infection characterized by painful purple-red swelling of the
eyelids, restriction of eye movement (Fig. 14.33), proptosis, and a
variable degree of decreased visual acuity. It may begin with eye pain
and low-grade temperature. In general it is caused by Staphylococcus
aureus, Haemophilus influenzae, Streptococcus, or Pneumococcus.
It usually follows an upper respiratory tract infection or sinusitis but
can occur from local trauma. If not treated promptly, it can lead to
abscess formation, blindness, or meningitis. Periorbital (preseptal)
cellulitis usually presents with edema and erythema of the eyelids (Fig.
14.34), minimal pain of the affected area, and fever. Proptosis or
ophthalmoplegia are not characteristic. Common organisms are H.
influenzae type B or Pneumococcus. In cases of eyelid trauma,
S. aureus and group A streptococcus are the most common pathogens.
|
|
|

|
|
Orbital
Cellulitis Left orbital
cellulitis with decreased range of motion secondary to edema. Note
the infected conjunctiva. (Courtesy of Javier A. Gonzalez del Rey,
MD.)
|
|
|
|
|
|
|
Periorbital
Cellulitis Left periorbital
cellulitis with edema and erythema of the eyelids. Note that the
conjunctiva is clear and not infected. (Courtesy of Kevin J. Knoop,
MD, MS.)
|
|
Differential Diagnosis
Erysipelas, allergic reactions,
trauma, sunburn, frostbite, chemical burns, subperiosteal abscess, and
cavernous sinus thrombosis should be considered.
Emergency Department Treatment
and Disposition
Parenteral antibiotic coverage
with broad-spectrum antistaphylococcal coverage, ophthalmologic
consultation, and admission are indicated in cases of orbital cellulitis.
Computed tomography of the orbit is necessary in certain cases to rule
out the possibility of an abscess requiring surgical drainage. In febrile
or ill-appearing patients with periorbital cellulitis, admission with
broad-spectrum antibiotic therapy is indicated. This coverage can be
adjusted once results of cultures are available. Mild cases of preseptal
cellulitis (especially those with history of trauma, e.g., abrasion,
insect sting) can be treated as outpatients with close follow-up.
Adequate coverage for Staphylococcus and Streptococcus is
necessary.
Clinical Pearls
1. Periorbital cellulitis
presents with circumferential redness, edema, and tenderness in the
febrile toddler. Orbital cellulitis must be considered if there is eye
pain or limitation of globe motion.
2. The conjunctiva is typically
clear with periorbital cellulitis.
|
|
Cystic Hygroma (Lymphangiomas)
Associated Clinical Features
Cystic hygromas are lymphatic
tumors found in the head and neck region (Fig. 14.35). They present as
nontender or nonpainful, compressible, unilocular or multilocular masses
with thin, transparent walls and are filled with straw-colored fluid.
Unlike hemangiomas, these lesions rarely undergo spontaneous regression.
The vast majority tend to grow and infiltrate adjacent structures. In
cases where the tongue is involved, they may produce tracheal compression
and respiratory difficulty.
|
|
|

|
|
Cystic
Hygroma A bright,
supraclavicular, soft, boggy, compressible mass consistent with
cystic hygroma. (Courtesy of Richard M. Ruddy, MD.)
|
|
Differential Diagnosis
Cavernous hemangiomas and
cavernous lymphangiomas should be considered.
Emergency Department Treatment
and Disposition
Surgery is the treatment of
choice in the vast majority of cases, since these lesions do not regress
and may affect local tissues. Extent of the lesion should be evaluated
prior to its removal (x-rays and computed tomography). The earlier these
lesions can be removed, the better the cosmetic results.
Clinical Pearls
1. The diagnosis of cystic
hygroma should be considered in all cases of spongy, soft, tumor-like
masses in the neck that are filled with fluid. Such a lesion may appear
spontaneously during a coughing episode or after Valsalva as a mass in
the neck.
2. This "benign"
tumor can locally invade adjacent tissues and become life-threatening.
|
|
Cat Scratch Disease
Associated Clinical Features
Cat-scratch disease is a benign,
self-limited condition that manifests with regional lymphadenopathy (Fig.
14.36), which usually follows (1 to 2 weeks) a skin papule at the
presumed site of bacterial inoculation. A history of contact with or
scratch from a cat (Fig. 14.37) is usually present. Lymphadenopathy may
persist for months and in rare cases patients may develop complications
such as encephalitis, osteolytic lesion, hepatitis, weight loss, fever,
and fatigue. A skin test using cat-scratch antigen can identify the
etiology in suspected patients when confirmation of the diagnosis is needed.
|
|
|

|
|
Cat
Scratch Disease An
erythematous, tender, suppurative node is seen in a young febrile
patient with a history of cat scratch on the extremity. The node
required drainage 2 days later. (Courtesy of Kevin J. Knoop, MD, MS.)
|
|
|
|
|

|
|
Cat
Scratch Disease The
precipitating wound that caused the suppurative node in Fig. 14.36.
(Courtesy of Kevin J. Knoop, MD, MS.)
|
|
Differential Diagnosis
Lymphogranuloma venereum,
bacterial adenitis, sarcoidosis, infectious mononucleosis, tumors (benign
or malignant), tuberculosis, tularemia, brucellosis, and histoplasmosis
should be considered.
Emergency Department Treatment
and Disposition
The disease is usually
self-limited and management is primarily symptomatic. Parents and
patients should be reassured that the nodes are benign and frequently
resolve within 2 to 4 months. In cases of painful, fluctuant nodes,
needle aspiration may be necessary for relief of symptoms. Antibiotic
therapy should be considered for acutely or severely ill patients.
Several anecdotal reports have suggested that oral antibiotics such as
rifampin, trimethoprim-sulfamethoxazole, and ciprofloxacin or intravenous
gentamicin, cefotaxime, and mezlocillin may be effective. Surgical
excision of the affected nodes is generally unnecessary.
Clinical Pearl
1. Cat-scratch disease is the
most common cause of regional adenitis and should be considered in all
children or adolescents with persistent lymphadenopathy.
|
|
Epiglottitis
Associated Clinical Features
Epiglottitis is a
life-threatening condition characterized by sudden onset of fever,
toxicity, moderate to severe respiratory distress with stridor, and
variable degrees of drooling. The patient prefers a sitting position,
leaning forward in a sniffing position with an open mouth. This
symptomatology is the result of a direct infection and subsequent
swelling of the epiglottis and aryepiglottic folds (Figs. 14.38 and
14.39) from Haemophilus influenzae type B (HIB). However, since
the release of the vaccine in 1985, there has been a dramatic decrease in
the incidence of this disease. Adults have a more indolent course and are
infrequently protected by the vaccine. Other infectious causes include
staphylococcal or streptococcal disease, thermal epiglottitis, and Candida
in the immunocompromised host. Direct thermal injuries have been reported
as a noninfectious cause of epiglottitis. On x-ray, the epiglottis is
seen as rounded and blurred (thumbprint) (Fig. 14.40). Epiglottitis
frequently worsens to complete obstruction if not treated with
endotracheal intubation and antibiotics.
|
|
|
|
|
Epiglottitis Endoscopic view of almost complete airway obstruction
secondary to epiglottitis. Note the slit-like opening of the airway.
(Courtesy of Department of Otolaryngology, Childrens Hospital Medical
Center, Cincinnati, OH.)
|
|
|
|
|
|
|
Epiglottitis Endoscopic view of the same patient
immediately after extubation. Although erythema and some edema
persist, the airway is widely patent. (Courtesy of Department of
Otolaryngology, Childrens Hospital Medical Center, Cincinnati, OH.)
|
|
|
|
|

|
|
Epiglottitis Lateral soft-tissue x-ray of the neck
demonstrating thickening of aryepiglottic folds and thumbprint sign
of epiglottis. (Courtesy of Richard M. Ruddy, MD.)
|
|
Differential Diagnosis
Acute infectious laryngitis,
acute laryngotracheobronchitis, acute spasmodic laryngitis, membranous
tracheitis, diphtheritic croup, aspiration of foreign body,
retropharyngeal abscess, and extrinsic or intrinsic compression of the
airway (tumors, trauma, cysts) should be considered.
Emergency Department Treatment
and Disposition
Immediate intervention is required.
An artificial endotracheal airway must be established. If time and
clinical status permit, this should be done in the operating room or
designated area where advanced airway management with sedation but not
neuromuscular paralysis can be implemented. An experienced
anesthesiologist and surgeon should be available in case a surgical
airway is needed. Once the airway has been protected, the patient should
be sedated to avoid accidental extubation and adequate antibiotic therapy
should be immediately instituted (second- or third-generation
cephalosporins or ampicillin/chloramphenicol).
Clinical Pearls
1. Children with epiglottitis
usually present with respiratory distress of sudden onset and high fever.
Because of the inflammation of the epiglottis, they commonly refuse to
drink fluids secondary to pain.
2. Every effort should be made
to allow the child to remain undisturbed (in mother's lap) in a position
of comfort while urgent preparations are made for airway management. An
agitated child is at risk for suddenly losing the airway.
|
|
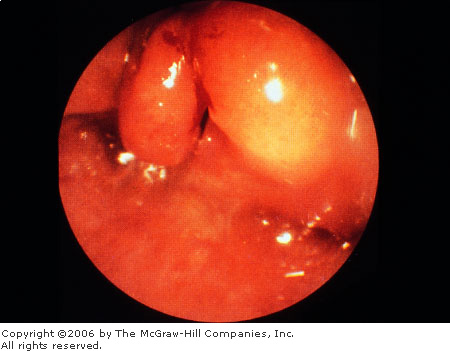
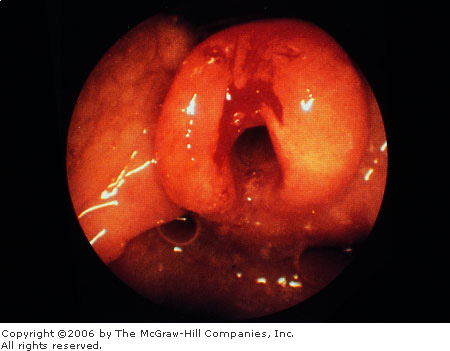
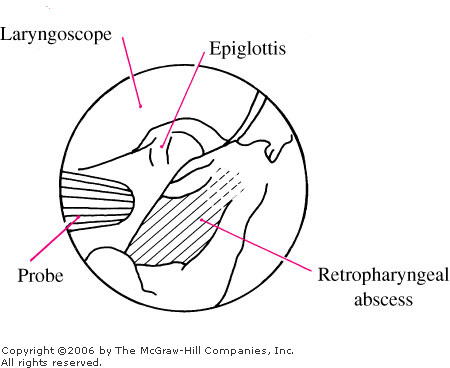
Retropharyngeal Abscess
Associated Clinical Features
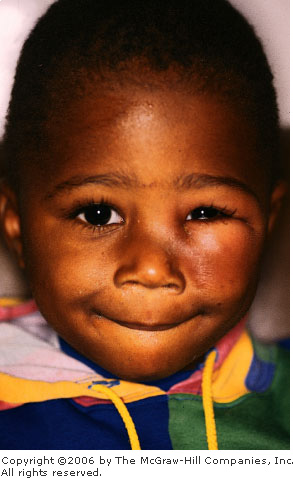
Patients with a retropharyngeal
abscess usually present with fever, difficulty in swallowing, excessive
drooling, sore throat, changes in voice, or neck stiffness (Fig. 14.41).
The resultant edema (Fig. 14.42) is the result of a cellulitis and
suppurative adenitis of the lymph nodes located in the prevertebral
fascia and is seen on a soft tissue lateral x-ray of the neck as
prevertebral thickening (Fig. 14.43). The initial insult may be the
result of pharyngitis, otitis media, or a wound infection following a
penetrating injury into the posterior pharynx. [It is helpful for the
examiner to be familiar with the normal laryngeal structures (Fig.
14.44)].
|
|
|

|
|
Retropharyngeal
Abscess This ill-appearing
6-year-old child presented with a several-day history of fever, neck
pain, sore throat, cough, and headache. Soft tissue lateral
radiography of the neck showed thickened prevertebral tissues
opposite C2-4. Computed tomography (CT) showed the airway narrowed to
a width of 5 mm within the oropharynx. (Courtesy of Mark Ralston,
MD.)
|
|
|
|
|

|
|
|
|
Retropharyngeal
Abscess Endoscopic view of a
retropharyngeal abscess. Note the massive swelling posteriorly.
(Courtesy of Department of Otolaryngology, Childrens Hospital Medical
Center, Cincinnati, OH.)
|
|
|
|
|

|
|
Retropharyngeal
Abscess Lateral soft tissue
neck x-ray demonstrating prevertebral soft tissue density consistent
with retropharyngeal abscess. (Courtesy of Richard M. Ruddy, MD.)
|
|
|
|
|

|
|
|
|
Normal
Laryngeal Structures
Endoscopic view of a normal epiglottis and surrounding structures.
(Courtesy of Department of Otolaryngology, Childrens Hospital Medical
Center, Cincinnati, OH.)
|
|
Differential Diagnosis
Acute laryngotracheobronchitis,
epiglottitis, membranous tracheitis, acute bacterial laryngitis,
infectious mononucleosis, peritonsillar abscess, aspiration of foreign
body, and diphtheria should be considered. These patients may present
with stiff neck mimicking meningitis.
Emergency Department Treatment
and Disposition
This illness requires immediate
intervention to prevent respiratory obstruction. The first step is to
evaluate the airway and establish an artificial one if necessary.
Antibiotic coverage should be initiated immediately (semisynthetic
penicillin or equivalent). Analgesia should be given as needed. If
obstruction is present or there is evidence of abscess, immediate
incision and drainage should be performed in the operating room. These
patients require hospitalization and immediate otolaryngologic or
surgical consultation.
Clinical Pearls
1. If the diagnosis of
retropharyngeal abscess is considered in a patient with the above
presentation, a lateral soft tissue neck x-ray may help to confirm the
diagnosis. In these cases, the retropharyngeal soft tissue at the level
of C-3 is > 5 mm, or more than 40% of the diameter of the body of C-4
at that level.
2. Computed tomography of the
neck is a useful tool to evaluate the extent of the lesion.
|
|
Membranous (Bacterial) Tracheitis
Associated Clinical Features
Membranous tracheitis is an acute
bacterial infection (Staphylococcus aureus, Haemophilusinfluenzae,
streptococci, and pneumococci) of the upper airway capable of causing life-threatening
airway obstruction. It is considered a bacterial complication because it
almost always follows an apparent viral infection of the upper
respiratory tract. The infection produces marked swelling and thick,
purulent secretions of the tracheal mucosa below the vocal cords. The
secretions form a thick plug that, if dislodged, may ultimately lead to
an acute tracheal obstruction. Patients appear toxic, with fever and a
croup-like syndrome that can progress rapidly. The usual treatment for
croup is ineffective in these patients. The characteristic
"membranes" may be seen on x-rays of the airway as edema with
an irregular border of the subglottic tracheal mucosa. On direct
laryngoscopy, copious purulent secretions can be found in the presence of
a normal epiglottis.
Differential Diagnosis
Acute laryngotracheobronchitis,
retropharyngeal abscess, peritonsillar abscess, foreign-body aspiration,
and acute diphtheric laryngitis can present in a similar manner.
Emergency Department Treatment
and Disposition
Otolaryngologic consultation
should be obtained as soon as the diagnosis is considered. Aggressive
airway management, including endotracheal intubation, may be needed to
protect the airway and allow for repeated suctioning to prevent acute
airway obstruction. The patient should be admitted to the intensive care
unit for close monitoring and sedation needs. Appropriate antibiotic
coverage against suspected organisms should be instituted immediately.
Clinical Pearls
1. Bacterial tracheitis often
presents with acute, severe airway obstruction after a short prodrome. It
should be suspected in all patients with an atypical croup-like
presentation: unusual age group, toxicity, not improving with routine
croup therapy, and unusual roentgenographic changes.
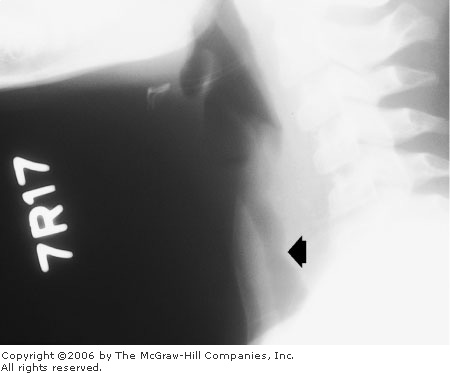
2. Up to 50% of soft tissue
films may delineate a subglottic membrane (Fig. 14.45).
|
|
|
|
|
Membranous
Tracheitis Lateral soft tissue
x-ray of the neck reveals mild subglottic narrowing (arrow)
and membrane consistent with bacterial tracheitis. (Courtesy of Alan
S. Brodie, MD.)
|
|
|
|
Physeal Fractures: Salter-Harris Classification
Associated Clinical Features
There are several fractures
unique to children. These include physeal fractures, torus fracture,
greenstick fractures, avulsion fractures, and bowing fractures or
deformities. Physis fractures (growth plate fractures) are relatively
common because of weakness of the germinal growth plate. The
Salter-Harris (SH) classification was designed to describe each type of
physeal fracture, its prognosis, and its treatment (Fig. 14.46).
|
|
|
|
|
Salter-Harris
Fracture Classification
Salter-Harris classification for epiphyseal plate fractures.
|
|
Differential Diagnosis
SH type I: Fracture
that extends through the physis. It is a very difficult radiologic
diagnosis since the fracture may not be displaced. It is usually a
clinical diagnosis, but occasionally a physeal widening is observed on
the x-ray.
SH type II: Oblique
fracture extending through the metaphysis into the physis. It is the most
common type and the prognosis is good.
SH type III: This rare
type of fracture goes along the growth plate, then extends through the
epiphysis, ossification center, and articular cartilage into the joint.
SH type IV: Fracture
that extends from the metaphysis, across the growth plate and into the
joint.
SH type V: Crushing
injury to the growth plate.
Emergency Department Treatment
and Disposition
Immobilization by splinting is
the treatment of choice in types I and II (minimum of 3 weeks). In these
cases, reduction is easy to achieve and maintain. Growth is unimpaired.
Types III and IV may require open reduction to avoid later traumatic
arthritis and, in some cases, growth arrest. Type V fractures are rare
and require very close follow-up because of arrest of growth caused by
the death of the germinal cells. Types III, IV, and V require immediate
orthopedic consultation.
Clinical Pearl
1. After initial assessment and
evaluation, always suspect SH type I if there is evidence of tenderness
around the growth plate area despite negative x-rays.
|
|
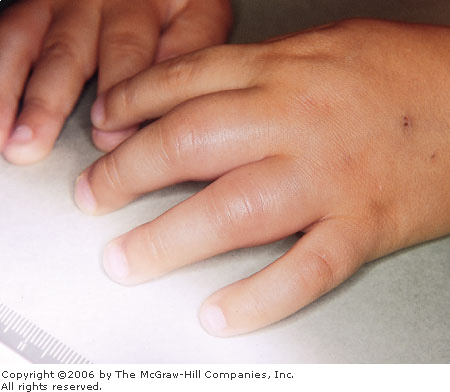
Acute Sickle Dactylitis (Hand-Foot Syndrome)
Associated Clinical Features
This painful condition is
commonly the first clinical manifestation of sickle cell disease. It
usually presents in children younger than 5 years of age. The pain and
abnormalities are the result of ischemic necrosis of the small bones
caused by the decreased blood supply as the bone marrow rapidly expands.
These children present acutely ill, with fever, refusal to bear weight,
and puffy hands and feet (Fig. 14.47). They may have a marked
leukocytosis, and the initial x-rays may be normal. It is not until 1 to
2 weeks later that subperiosteal new bone, cortical thickening, and even
complete bone destruction can be seen.
|
|
|
|
|
Acute
Sickle Dactylitis Bilateral
cylindrical swelling of soft tissue of the hands in sickle cell
disease consistent with vasoocclusive crisis or dactylitis. (Courtesy
of Donald L. Rucknagel, MD, PhD.)
|
|
Differential Diagnosis
Osteomyelitis, trauma, cold
injuries, acute rheumatic fever, juvenile rheumatoid arthritis, and
leukemias should be considered.
Emergency Department Treatment
and Disposition
The most important aspects in the
treatment of vasooclusive crisis in sickle cell disease (hemoglobin SS)
include an adequate fluid balance, oxygenation, and analgesia. Therapy
should be individualized. Codeine, hydromorphone, morphine, and ketorolac
are analgesic agents commonly used in the treatment of children with
painful sickle crisis. In cases of dactylitis, very close follow-up is
necessary not only for the management of sickle cell disease but to
reevaluate the radiologic changes in small bones. In most instances, the
previously described changes disappear; however, in rare cases,
shortening of the fingers and toes has been described as the result of
severe bone infarcts.
Clinical Pearl
1. Most clinical manifestations
of sickle cell disease occur after the first 5 to 6 months of life. The
hemolytic anemia gradually develops over the first 2 to 4 months (changes
that follow the replacement of fetal hemoglobin by hemoglobin S) and
leads to the clinical syndromes associated with an increased SS hemoglobin.
|
|
Hair Tourniquet
Associated Clinical Features
A single strand of hair or thread
may encircle a finger, a toe, or the penis, leading to constriction (Fig.
14.48). Children in their first year of life are particularly at risk
from inadvertent attachment of a parent's hair or loose thread. The digit
appears edematous, erythematous, and painful. If not corrected vascular
compromise or infection can ensue.
|
|
|

|
|
Hair
Tourniquet A strand of hair
has encircled the middle toe in two places, causing erythema and
swelling. (Courtesy of Kevin J. Knoop, MD, MS.)
|
|
Differential Diagnosis
Insect bites, trauma, or
cellulitis of the digit may have a similar appearance.
Emergency Department Treatment
and Disposition
Visualization of the constricting
material may be difficult. Edema, erythema, and periarticular skin folds
may hide the hair or thread. It is imperative to carefully retract the
skin around the proximal aspect of the edema. A magnifying lens may be
helpful in identifying the band. Since the removal can be painful,
consider local digital block prior to removal. Using a small hemostat,
grasp a portion of the material, and then cut it with a surgical blade.
On occasions, depilatory agents have been used to remove hair fibers.
Elevation of the involved digit after removal of the constricting agent
provides resolution of the edema and erythema within 2 to 3 days. In some
cases the digit's blood supply may have been irreversibly compromised.
Subspecialty consultation should be considered whenever neurovascular
integrity is in question.
Clinical Pearl
1. In the vast majority of
cases, a clear line of demarcation can be identified between the normal
tissue and the affected area.
|
|
Failure to Thrive
Associated Clinical Features
Failure to thrive (FTT) is a
chronic pattern of inability to maintain a normal growth pattern in
weight, stature, and occasionally in head growth (Fig. 14.49). It is most
common in infancy, and the condition is nonorganic (50%), organic (25%),
or mixed (25%) in etiology. The diagnosis is made after complete history
and physical examination with comparison of the measurements of length
(supine in children <3 years of age), weight, and head circumference
(maximal occipital-frontal circumference) to standard measurements. In
cases of deficient caloric intake or malabsorption, the patient's head
circumference is normal and the weight is reduced out of proportion to
height. Subnormal head circumferences with weight reduced in proportion
to height and normal or increased head circumferences with weight
moderately reduced are usually indicative of an organic problem.
|
|
|

|
|
Failure
to Thrive This infant has not
been able to maintain a normal growth pattern and appears cachectic.
(Courtesy of Kevin J. Knoop, MD, MS.)
|
|
Differential Diagnosis
The differential diagnosis of
failure to thrive is lengthy. Nonorganic disorders include poor feeding
technique, disturbed maternal-child interaction, emotional deprivation,
inadequate caloric intake, and child neglect. Organic causes are numerous.
Emergency Department Treatment
and Disposition
Depending on history, physical
findings, and the social situation, some cases can be managed as
outpatients. The primary care provider can determine whether outpatient
management is indicated. For the vast majority of cases, if the diagnosis
of failure to thrive is made in the ED, admission is suggested to
complete the evaluation. This could be the only indication of a poor
social environment or inadequate access to medical care. Initial
laboratory investigations should include a complete blood count,
electrolytes, BUN and creatinine urinalysis, and stool examination if the
stool pattern is abnormal. More specific testing should be used only if
clinically indicated and targeted to the possible underlying cause. Early
involvement of social services may facilitate the evaluation and
follow-up. Treatment will vary according to the underlying disorder.
Clinical Pearl
1. Failure to thrive in
neglected children is accompanied by signs of developmental delays,
emotional deprivation, apathy, poor hygiene, withdrawing behavior, and
poor eye contact.
|
|
Nursemaid's Elbow (Radial Head Subluxation)
Associated Clinical Features
Nursemaid's elbow is a condition
that occurs commonly in children younger than 5 years of age who are
usually picked up or pulled by the arm while the arm is pronated. The
children present unwilling to supinate or pronate the affected elbow
(Fig. 14.50). Generally they keep the arm in a passive pronation and
develop pain over the head of the radius. Radiographic studies should be
considered only in patients with an unusual mechanism of injury or those
who do not become rapidly asymptomatic after the reduction maneuvers.
|
|
|

|
|

|
|

|
|
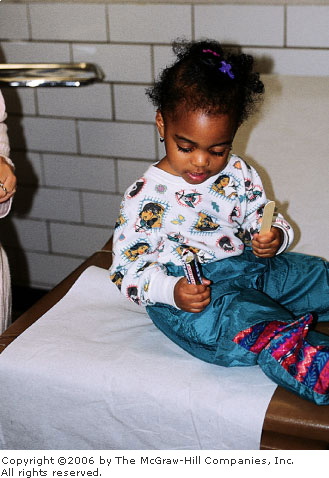
Nursemaid's
Elbow This child presents with
pseudoparalysis of the right arm after a pulling injury. Note how she
avoids use of the affected arm and preferentially uses the other arm.
(Courtesy of Kevin J. Knoop, MD, MS.)
|
|
Differential Diagnosis
Radial head fracture or complete
dislocation, posterior elbow dislocation, condylar and supracondylar
fractures of the distal humerus, or buckle fracture of radius or ulna
should be considered.
Emergency Department Treatment
and Disposition
Carefully palpate for tenderness
at all points of the affected arm. (No tenderness is found when not
rotating the involved arm.) Orthopedic consultation is generally not
indicated unless an underlying fracture is diagnosed. Reduction is
usually achieved by one of two maneuvers: (1) while supinating the
forearm, pressure is applied over the radial head and the elbow is
flexed, or (2) while holding the elbow in extension, hyperpronation of
the forearm is maintained until reduction is achieved. The patient
usually becomes asymptomatic after a few minutes (Fig. 14.51). When the
injury has been present for several hours, reduction may be difficult,
and it may take several hours to recover full function of the elbow.
|
|
|
|
|
|
|
|
|
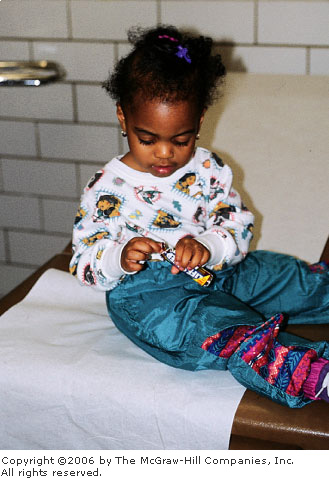
Nursemaid's
Elbow—Reduced After
reduction, there is initial reluctance to use the injured arm. With
distraction and encouragement, the patient demonstrates successful
use of the extremity. (Courtesy of Kevin J. Knoop, MD, MS.)
|
|
Clinical Pearls
1. In any child (usually
between 1 to 5 years of age) who presents with sudden onset of elbow pain
and immobility following a traction injury, the diagnosis of nursemaid's
elbow should be strongly considered.
2. Nonjudgmental parental
education about the mechanism should be an integral part of the visit.
|
|
Nursing Bottle Caries
Associated Clinical Features
This extensive form of tooth
decay (generally in the necks of the teeth near the gingiva) is the
result of sleeping with a bottle containing milk or sugar-containing
juices. The condition generally occurs before 18 months of age and is
more prevalent in medically underserved children. Upper central incisors
are most commonly involved (Fig. 14.52).
|
|
|

|
|
Nursing
Bottle Caries Extensive tooth
decay from sleeping with a bottle containing milk or sugar-containing
juices. (Courtesy of Lawrence B. Stack, MD.)
|
|
Differential Diagnosis
Less extensive tooth decay
(caries) may be seen in some infants who do not sleep with a bottle.
Caries can also result from tooth trauma. Dental referral is indicated.
Emergency Department Treatment
and Disposition
Parental education and immediate
referral to a dentist is necessary to prevent complications. If
untreated, the caries may destroy the teeth and spread to contiguous
tissues. These patients have a high risk for microbial invasion of the
pulp and the alveolar bone, with the subsequent development of a dental
abscess and facial cellulitis. In these cases, aggressive treatment with
antibiotics (penicillin) and pain control, with prompt dental referral
for definitive care, is necessary.
Clinical Pearl
1. The role of the ED physician
is to recognize this pattern of dental decay (upper incisors most
commonly) and immediately initiate dental referral and parental
education.
|
|
Pinworm Infection (Enterobiasis)
Associated Clinical Features
Enterobius vermicularis is
a 0.5-in. threadlike white worm that infects the colon and causes intense
pruritus of the perianal region, where the adult gravid female migrates to
deposit eggs (Fig. 14.53). On rare occasions it can cause vulvovaginitis.
The diagnosis can be made by direct visualization of the nematode by the
parents or by using a transparent adhesive tape and touching it to the
perianal lesion (at night). This tape is then applied to a glass slide
for microscopic examination under low power.
|
|
|

|
|
Pinworms Multiple tiny pearly-white worms are seen at
the anus. (Courtesy of Timothy D. McGuirk, DO.)
|
|
Differential Diagnosis
Perianal irritation, fissures,
hemorrhoids, and contact dermatitis should be considered.
Emergency Department Treatment
and Disposition
The treatment of choice is
pyrantel pamoate or mebendazole. Either of these drugs is given as a
single dose and repeated in 1 to 2 weeks (to treat secondary hatchings of
the organism). Because of the high frequency of reinfection, families
should be treated as a group.
Clinical Pearls
1. Reinfection from other
infected individuals or autoinfection is necessary to maintain
enterobiasis in the individual, since these nematodes usually die after
depositing their eggs in the perianal region. Good personal hygiene may
reduce chances of infection.
2. If there is evidence of
cellulitis, antibiotic coverage primarily against Staphylococcus
is indicated.
3. If infection and point
tenderness (in the absence of cellulitis) persist, antipseudomonal
coverage should be considered.
4. Pinworms are the most common
cause of pruritus in children.
|
|
Oculogyric Crisis
Associated Clinical Features
Oculogyric crisis (OGC) is the
most common of the ocular dystonic reactions. It includes blepharospasm,
periorbital twitches, and protracted staring episodes. Usually it occurs
as a side effect of neuroleptic drug treatment. OGC represents
approximately 5% of the dystonic reactions. The onset of a crisis may be
paroxysmal or stuttering over several hours. Initial symptoms include
restlessness, agitation, malaise, or a fixed stare followed by the more
characteristically described maximal upward deviation of the eyes in a
sustained fashion. The eyes may also converge, deviate upward and
laterally, or deviate downward. The most frequently reported associated findings
are backward and lateral flexion of the neck, widely opened mouth, tongue
protrusion, and ocular pain (Fig. 14.54). A wave of exhaustion follows
some episodes. Other features noted during attacks include eye blinking,
lacrimation, pupil dilation, drooling, facial flushing, vertigo, anxiety,
and agitation.
|
|
|

|
|
Oculogyric
Crisis This 6-year-old boy
developed extrapyramidal symptoms, including opisthotonos and
oculogyric crisis, after his dosage of risperidone was increased.
Benadryl 12.5 mg PO given at home resolved the opisthotonos.
Persistent oculogyric crisis (vertical gaze deviation) and hypertonia
resolved completely after Benadryl 25 mg IM. (Courtesy of Mark
Ralston, MD.)
|
|
Differential Diagnosis
Several medications have been
associated with the occurrence of OGC: neuroleptics, amantadine,
benzodiazepines, carbamazepine, chloroquine, levodopa, lithium, metoclopramide,
and nifedipine. Careful history and physical examination should exclude
the possibility of focal seizures, encephalitis, head injury, conversion
reaction, and other types of movement disorders.
Emergency Department Treatment
and Disposition
Treatment in the acute phase in
children involves reassurance and diphenhydramine at a dosage of 1 mg/kg
initially; this may be repeated if there is no effect. Occasionally,
doses up to 5 mg/kg are required. Benztropine and/or diazepam or
lorazepam can also be used; however, benztropine is not approved for
children below 3 years of age, and this agent has been noted to cause
dystonic reactions. Close monitoring of these drug side effects is
important during treatment and for a few hours thereafter because dystonic
reactions are occasionally accompanied by fluctuations in blood pressure
and disturbances of cardiac rhythm.
Clinical Pearls
1. The abrupt termination of
the psychiatric symptoms at the conclusion of the crisis, after the use
of diphenhydramine, is diagnostic and most striking.
2. In infants presenting with
"seizures" and unusual behavior, eye deviation and history of
reflux treated with metoclopramide, the possibility of OGC should always
be included in the differential. Although the overall incidence of
extrapyramidal effects associated with this drug is 0.2%, very old and
very young patients are affected more commonly, with an incidence as high
as 10%. These side effects usually occur within a few days after
initiation of the medication, as in this case, and are more common at
higher doses.
|
|
Herpes Zoster
Associated Clinical Features
Herpes zoster virus (HZV) has
been noted as early as the first week of life (in infants born to mothers
who contracted varicella during pregnancy). These lesions can present in
the distribution of one to three sensory dermatomes (Fig. 14.55). Pain is
intense and in certain cases can persist beyond 1 month after the lesions
have disappeared (postherpetic neuralgia). The diagnosis is usually made
clinically; however, tissue cultures, direct fluorescent antibodies, and
Tzanck smears (see Fig. 13.15) can be done from vesicle scraping to
confirm the diagnosis.
|
|
|

|
|
Herpes
Zoster Vesicles in a classic
dermatomal distribution are seen in this child. (Courtesy of Frank
Birinyi, MD.)
|
|
Differential Diagnosis
The diagnosis is usually
clinically apparent but not always straightforward. Impetigo and
cutaneous burns (cigarette) may mimic the appearance of herpetic
vesicles. Varicella is more diffusely spread, although a small crop of
lesions may mimic zoster. Zoster may mimic herpes simplex virus (HSV),
although a close examination should reveal a dermatomal distribution in
zoster.
Emergency Department Treatment
and Disposition
The management of HZV in children
is limited to symptomatic treatment and prevention of secondary
infections. Oral acyclovir is not recommended for routine use in otherwise
healthy children with zoster or varicella. However, acyclovir therapy
should be considered in older children with severe cases, chronic
cutaneous or pulmonary disorders, and patients receiving salicylates or
corticosteroids therapy. Intravenous antiviral therapy is recommended for
immunocompromised patients. There is no pediatric formulation of
famciclovir and valacyclovir or sufficient data on their use in children.
Clinical Pearls
1. HZV can occur in children of
all ages.
2. A vesicular rash with a dermatomal
distribution is diagnostic of HZV.
3. Reports are that acyclovir
is of benefit only if used within 24 h of the initial presentation
(modest decrease of symptoms).
4. An infected patient can
transmit chickenpox (varicella) to a nonimmune child.
|
|
Henoch-Schönlein Purpura (HSP)
Associated Clinical Features
Also known as "anaphylactoid
purpura," HSP is a systemic vasculitis of small vessels
characterized by 2- to 10-mm erythematous hemorrhagic papules in a
symmetric acral distribution, over the buttocks, and extremities (Fig.
14.56; see Fig. 15.19). Lesions occur in crops, fade after 5 days, and
are followed by purpura ("palpable purpura"), abdominal pain
(caused by edema and hemorrhage of the intestinal wall), and joint
symptoms. HSP is a disease of children (commonly aged 3 to 12 years) and
young adults. Mucosal involvement is rare; however, edema of the scalp,
hands, scrotum, and periorbital tissue is not uncommon. Gastrointestinal
symptoms (abdominal pain, occult and gross bleeding, and intussusception)
may precede the rash. Renal involvement is the most frequent and serious
complication and usually occurs during the first month. It commonly
manifests itself as acute glomerulonephritis. Hypertension is uncommon.
The diagnosis is made by history and clinical examination. Laboratory
tests are usually normal (platelets, complement level, and antinuclear
antibodies) except for the urinalysis, which may be positive for blood or
protein in 50% of the patients. The prognosis is excellent, with full
recovery in most instances. The course of HSP is marked by relapses and
remissions in 50% of patients (rash seems to recur within the first 6
weeks). Prognosis is dictated by the renal involvement. Overall, 1 to 4%
of patients progress to end-stage renal disease.
|
|
|

|
|
Henoch-Schönlein
Purpura These erythematous,
hemorrhagic papules and petechiae in a symmetric acral distribution
are classic findings in HSP. This child presented with no other
symptons. (Courtesy of Kevin J. Knoop, MD, MS.)
|
|
Differential Diagnosis
During the initial phases of the
disease, the diagnosis may be difficult. Rash may be confused with drug
reactions, erythema multiforme, urticaria, and even physical abuse. Other
causes of purpura, bleeding disorders, and/or infection (meningococcemia)
should always be included in the differential diagnosis.
Emergency Department Treatment
and Disposition
Treatment is empiric,
symptomatic, and supportive. Corticosteroids are used acutely to treat
severe abdominal pain or arthritis. In cases where intussusception is
suspected, prompt surgical consultation and diagnostic ultrasonography or
air-contrast enema fluoroscopy (diagnostic and therapeutic) is indicated.
Patients with HSP limited to the skin and joints can be managed as
outpatients. Severe abdominal pain, gastrointestinal hemorrhage,
intussusception, and severe renal involvement are indications for
admission.
Clinical Pearls
1. All children presenting to
the ED with suspected HSP and gastrointestinal symptoms should have a
stool guaiac test performed and a urinalysis to monitor for nephritis.
2. Intussusception associated
with HSP is seen in 2% of patients, most commonly in boys, particularly
those about 6 years of age.
|
|