|
Note: Large images and
tables on this page may necessitate printing in landscape mode.
Copyright
©2006 The McGraw-Hill Companies. All rights reserved.
Emergency
Medicine Atlas > Part 2. Specialty
Areas > Chapter 15. Child Abuse > Physical
Abuse >
|
Inflicted Burns
Associated Clinical Features
Burns in children are frequently
the result of child abuse. The most common types of pediatric burns from
abuse are immersion burns and contact burns. Certain clues may assist the
physician in differentiating accidental burns from inflicted burns, but
often considerable doubt remains even after a careful evaluation.
In an immersion burn, a
thoughtful assessment of the pattern and location of the burns, as well
as of the unaffected areas, helps to differentiate between accidental and
inflicted burns. Postulate possible mechanisms for the injury and
correlate the assessment with the given history. A child who is held
firmly and deliberately immersed has burn margins that are sharp and
distinct. If the child has little opportunity to struggle, few or no
burns from splashing liquid will occur. In contrast, a child who
accidentally comes into contact with a hot liquid will move about in an
attempt to escape further injury. This movement causes the burn margins
to be less distinct and may result in additional small burns as hot
liquid splashes onto the skin. Children who are "dipped" into a
bath of hot water often show sparing of their feet and/or buttocks
because they are held firmly against the tub's bottom (Fig. 15.1). A
child who has had a hand dipped into hot water and held there may
reflexively close the fingers, sparing the palm and fingertips.
|
|
|

|
|
Immersion
Burns Immersion burns are
often associated with toilet training accidents. This girl was
plunged into hot water after soiling herself. She shows sparing of
the buttocks, which contacted the surface of the bathtub and avoided
being burned. (Courtesy of The Visual Diagnosis of Child Physical
Abuse. American Academy of Pediatrics, 1994.)
|
|
Contact burns usually have a distinct and
recognizable shape. Contact burn patterns most commonly associated with
abuse include burns from curling irons, hair dryers, heater elements, and
cigarettes (Figs. 15.2, 15.3, 15.4, 15.5). A child who has multiple
contact burns or burns to areas that are unlikely to come in contact with
the hot object accidentally should be evaluated for abuse.
|
|
|

|
|
Contact
Burn (Curling Iron) Burns on
the chest and abdomen from a curling iron. The burn pattern on the
injured skin indicates multiple contact burns from an object the size
and shape of a curling iron. Accidental curling iron burns occur, but
because this infant has so many burns, the injury is suspicious for
abuse. Child abuse should be suspected and reported unless the
historian can provide a plausible explanation of how these burns
occurred accidentally. (Courtesy of Robert A. Shapiro, MD.)
|
|
|
|
|

|
|
Contact
Burn (Hair Dryer) The heated
grid from the end of a hair dryer caused this child's burns. The burn
size and pattern marks of the burn matched exactly the hair dryer
grid that was found in the child's home. The history of accidental
injury was thought to be unlikely, and child abuse was suspected.
(Courtesy of Robert A. Shapiro, MD.)
|
|
|
|
|

|
|
Contact
Burn (Heater Grate) This child
was held against a heater grate. The pattern became more obvious with
the child's knee flexed—the position of the leg at the time of
the injury. (Courtesy of David W. Munter, MD.)
|
|
|
|
|

|
|
Contact
Burn (Cigarette) Cigarette
burns are circular injuries with a diameter of about 8 mm. It can be
difficult for the clinician to determine if the burn is from an
accidental injury or from abuse. Children who accidentally run into a
lit cigarette often have burns to the face or distal extremities.
Accidental burns may be less distinct and deep compared with
inflicted burns. A report of alleged child abuse should be made if
there are multiple cigarette burns, burns to locations unlikely to
come into contact with a cigarette accidentally, or other signs that
suggest abuse. (Courtesy of Robert A. Shapiro, MD.)
|
|
Differential Diagnosis
Some burn look-alikes may be
confused with child abuse. Impetigo (Fig. 15.6) may be mistaken for
healing cigarette burns, and bullous impetigo can resemble second-degree
burns. Contact dermatitis and cellulitis may resemble first-degree burns.
|
|
|

|
|
Impetigo These circular lesions of impetigo resemble
healing cigarette burns. (Courtesy of Michael J. Nowicki, MD.)
|
|
Emergency Department Treatment
and Disposition
Document thoroughly all burns
that may be due to abuse. Draw sketches and take photographs of the
injuries. Obtain a skeletal survey in children under the age of 2 years.
Report any suspected abuse immediately to the local child protective
agency before discharge from the ED. Provide standard burn therapy.
Clinical Pearls
1. Evaluate the alleged history
carefully and obtain sufficient details before making any judgment.
Assess whether the explanation and history that are given of the alleged
episode are inconsistent with the injuries and/or with the child's
developmental abilities. Suspect abuse if, without convincing
explanation, the historian alters the initial history.
2. Maintain a high index of
suspicion whenever caring for a pediatric burn patient. Look carefully
for other signs of abuse, such as bruising, fractures, or signs of
neglect.
3. Accidental burns from a
cigarette are usually single, superficial, and not completely round.
Common sites of accidental cigarette burns are the face, trunk, and
hands.
4. Report suspicions to the
mandated child protection agency whenever a burn may have been
deliberately inflicted.
5. Injuries due to suspected
child abuse may be photographed without parental consent in most states.
|
|
Inflicted Bruises and Soft-Tissue Injuries
Associated Clinical Features
Bruises are the most common
manifestation of physical child abuse. Child abuse should be suspected
whenever bruises are (1) over soft body areas, such as the thighs,
buttocks (Fig. 15.7), cheeks, abdomen, and genitalia, since common
childhood activities do not commonly cause trauma to these areas; (2)
more numerous than usual; (3) of different ages (suggests repeated
episodes of abuse); (4) the shape of objects such as belts, cords, or
hands (demonstrates that the injuries were inflicted) (Figs. 15.8, 15.9,
15.10); or (5) noted in young, nonambulating children (infants are not
capable of getting into accidents).
|
|
|

|
|
Gluteal
Fold Bruises This injury to
the buttocks demonstrates linear, parallel bruises near the gluteal
folds. Forceful spanking causes gluteal fold bruises. They do not
indicate a separate trauma in addition to the spanking. (Courtesy of
Robert A. Shapiro, MD.)
|
|
|
|
|

|
|
Looped
Pattern Markings Loop marks
are clearly seen within the bruising on this child's back. The loop
marks indicate that an extension cord, belt, or some similar object
was used to punish him. The color of the bruise is red, which
indicates that the injury is only a few days old. (Courtesy of Robert
A. Shapiro, MD.)
|
|
|
|
|

|
|
Hand-Print
Bruise Bruise from a slap
showing the outline of her father's hand is clearly seen on the back
of this adolescent. (Courtesy of Robert A. Shapiro, MD.)
|
|
|
|
|

|
|
Linear
Bruises These linear, parallel
bruises on the buttocks with unaffected skin between them are
indicative of an injury caused by an object. The width of the object
can be determined by measuring the space between the parallel lines.
Common objects that cause injuries like these, include belts,
fingers, cords, and rulers. (Courtesy of Robert A. Shapiro, MD.)
|
|
The color of the ecchymosis will change as healing
progresses. New injuries are usually red and purple. They may also be
tender and swollen. Within a few days, the bruise may turn blue, then
green, then yellow, and finally brown. The shape and margins of the
bruise become less distinct as it heals. The time period in which these
color changes occur is variable. Some bruises resolve within a few days,
whereas others resolve over weeks. The amount of time until resolution
depends on factors such as the location, size, and depth of the injury.
Bite marks (Figs. 15.11, 15.12,
15.13) have special forensic characteristics that should be recorded. The
size, shape, and pattern of the injury can identify a specific
perpetrator. Most human bite injuries are caused by children, not adults,
but recognition of an adult bite is important because the injury
represents abuse. Compared with an adult's, the shape of a child's bite
is rounder. If the impressions from the canines are visible in the bite,
the perpetrator's age can be estimated. Most children under 8 years of
age have less than 3 cm between their canines. Some bites have saliva
within the center of the bite, which can also be used to identify the
perpetrator. Although some bite marks are immediately obvious during the
initial inspection, others can be difficult to recognize. If an adult
bite is suspected but unprovable because distinct impressions of the
teeth are absent, reexamination of the injury a few days later may
facilitate recognition and documentation.
|
|
|

|
|
Bite
Mark (Child) Distinct
impressions of teeth are seen in this injury. The shape of the injury
outlines the upper and lower oral arches. Note the size of the
mother's mouth in relation to the size of the bite on the neck,
making an adult mouth an unlikely source. (Courtesy of Kevin J.
Knoop, MD, MS.)
|
|
|
|
|

|
|
Bite
Mark (Adult) This bite mark is
on a young girl's breast. Note the larger size of the wound, which is
more consistent with an adult bite. (Courtesy of Robert A. Shapiro,
MD.)
|
|
|
|
|

|
|
Bruises Bruises cover this child's left arm. The
circular bruise on the upper arm is a human bite. Saliva from the
perpetrator will usually be present within the center of the bite if
the injury is acute and the skin has not yet been washed. Moistened
swabs should be used to transfer the saliva from the skin onto the
gauze. This gauze must be saved for DNA analysis. As with all trace
evidence, the chain of evidence must be documented. (Courtesy of
Robert A. Shapiro, MD.)
|
|
The bites of animals are usually
easy to distinguish from human bites. The size is usually smaller and the
shape of the arch mark is narrower than a human's. Sharp animal canines
often cause tearing of the skin instead of the crushing seen in human
bites.
Differential Diagnosis
Bleeding disorders—such as
idiopathic thrombocytopenic purpura (ITP), Henoch-Schönlein purpura, and
leukemia—can mimic child abuse. Folk remedies, such as cupping and
coining, may result in soft tissue findings that are not reportable as
abuse (see "Lesions Mistaken for Abuse," below).
Emergency Department Treatment
and Disposition
Completely undress the child and
look for additional signs of abuse (Figs. 15.14 and 15.15). Obtain a
complete history of all injuries. Sketch and photograph the injuries.
Obtain a platelet count and bleeding studies [prothrombin time and
partial thromboplastin time (PT and PTT)] to rule out a bleeding
diathesis as the cause of the findings. For children under 2 or 3 years
of age who have extensive injuries, obtain a skeletal survey, alanine
transferase (ALT), aspartate aminotransferase (AST), amylase, and
urinalysis.
|
|
|

|
|
Pinch
Marks on Pinna Children may be
pulled up or along by their ears, causing this injury. A child's ears
should be inspected for this injury whenever abuse is suspected.
(Courtesy of Robert A. Shapiro, MD.)
|
|
|
|
|

|
|
Strangulation
Bruise This child was beaten
while at the sitter's and suffered circumferential linear neck
abrasions consistent with attempted strangulation. There is also
occipital ecchymosis from the abuse. (Courtesy of Barbara R. Craig,
MD.)
|
|
If human bites are found or
suspected, consider consultation with a forensic dentist. If appropriate,
collect swabs for DNA forensic analysis from the center of unwashed,
fresh bites, which may contain saliva from the perpetrator.
Report suspected abuse to the
legally mandated child protection agency before the child is discharged
from the ED.
Clinical Pearls
1. Determination of the age of
a bruise is imprecise. Bruises that are "fresh" (< 48 h) are
usually recognizable because they are tender, red, and swollen.
Occasionally, bruises may not be visible for up to 48 h after an injury.
2. Children may deny abuse when
questioned because of threats made to them. The child in Fig. 15.16
initially denied that he had been gagged. He told the examining physician
that he had spilled some cleaning fluid onto his lips.
3. When a parent or caretaker
inflicts an injury while disciplining a child, the incident must be
reported to the local child protection agency. Even if corporal
punishment is lawful in a given state, the infliction of an injury is
never lawful.
4. Place a millimeter ruler or
coin next to a pattern injury before taking photographs so that
measurements can be made.
5. Consent is not required in
most states to photograph injuries suspicious for child abuse.
|
|
|

|
|
Gagging
Bruise This child had a sock
stuffed into his mouth and tied around his head. The bruises in the
corners of the child's mouth are indicative of gagging. Additionally,
there are circular bruises on his left and right cheeks caused from
the perpetrator's fingers while holding the child still to insert the
sock. Pattern markings within the bruises match the fabric pattern of
the sock. Photographs of these patterns should be obtained and
provided to the police. The red color of the bruises and the fresh
facial excoriations indicate that the injuries are recent. (Courtesy
of Robert A. Shapiro, MD.)
|
|
|
|
Lesions Mistaken for Abuse
Associated Clinical Features
Whenever bruising is excessive,
is not associated with a compatible history, or occurs in an unusual
distribution, seek a specific etiology. It may be appropriate to suspect
and report child abuse when these conditions exist but also consider
other diagnoses.
Common Childhood Bruising
Accidental trauma can result in a
bruise to any part of the body, but the forehead and the extensor
surfaces of the tibia, elbow, and knee are the most common locations.
When other areas of the body are bruised, etiologies other than accidental
bruising should be considered.
Mongolian Spots
Mongolian spots are bluish sacral
or truncal lesions, most often seen in non-Caucasian infants and young
children. They may be mistaken for bruises. Mongolian spots may be
limited to only a few lesions, or they may extend up the back and
shoulders of the child (Fig. 15.17).
|
|
|

|
|
Mongolian
Spots Numerous mongolian spots
on this youngster extend up the back and shoulders. (Courtesy of
Douglas R. Landry, MD.)
|
|
Cupping, Coining, and
Moxibustion
Asian families sometimes practice
traditional cures with their children, such as cupping, coining, and
moxibustion. Each of these practices leaves markings on the child's skin,
which may be interpreted as child abuse. In cupping, a flammable object
is ignited and placed into a cup. After the flames have extinguished, the
cup is inverted and placed onto the child's skin. As the warm air within
the cup cools, a vacuum is produced. This "cure" leaves
circular suction markings on the child's skin but should not be painful
to the child. Coining (Fig. 15.18) is done by rubbing a coin up and down
the child's back, just lateral to the spine. This results in petechiae
and chronic skin changes on the back. Coining should also not be painful
to the child. Neither of these practices should be reported as child
abuse. In moxibustion, a flammable object, such as a thread, is ignited
on or near the child's skin. Moxibustion may cause superficial burns.
Whether moxibustion is reported as child abuse would depend on the
physical findings and the judgment of the physician.
|
|
|

|
|
Coining
(Cheut Sah or Cao Gio) This
child has petechiae and bruising along her spine. Her parents were
practicing the Southeast Asian practice of coining, a healing remedy,
in which a coin is rubbed along the spine to heal an illness. Coining
should not be painful and is not considered abusive. (Courtesy of
Charles Schubert, MD.)
|
|
Henoch-Schönlein Purpura
Henoch-Schönlein purpura (HSP) is
a vasculitis of the small blood vessels. The skin lesions are usually
small, symmetric, palpable purpuras. They may appear in a linear pattern
and are often confined to the lower extremities (Fig. 15.19). Associated
symptoms may include joint and abdominal pain.
|
|
|

|
|
Henoch-Schönlein
Purpura (HSP) This child has
palpable purpura on the extensor surfaces of the legs. HSP should be
considered whenever there is symmetric ecchymosis along the extensor
surfaces of the extremities and buttocks. The illness is most often
seen in school-age children. Migratory arthritis and abdominal pain
may be present. (Courtesy of Ralph A. Gruppo, MD.)
|
|
Idiopathic Thrombocytopenic
Purpura
Idiopathic thrombocytopenic
purpura (ITP) is an acquired platelet disorder that results in abnormal
bleeding. It is most common in 1- to 4-year-old children. The presenting
complaint is most often abnormal bruising. The bruises can appear
anywhere on the body and are numerous, mimicking child abuse. The child
may also have epistaxis, hematuria, or other bleeding.
Hemophilia
Hemophilia is usually diagnosed
soon after birth because of abnormal bleeding. The ecchymosis and
soft-tissue swelling are greater than would be expected given the history
of trauma (Figs. 15.20, 15.21).
|
|
|

|
|
Hemophiliac
with Bruising This child's bruising
is due to factor VIII deficiency. The degree of bleeding within the
ecchymosis is more extensive than that seen in children without
coagulopathies. A history of other abnormal bleeding episodes or a
history that the child suffers from a coagulopathy is most often
obtained at the time of presentation. (Courtesy of Ralph A. Gruppo,
MD.)
|
|
|
|
|

|
|
Grey
Turner's Sign This child
presented after a minor fall. This pattern of bruising (flank
ecchymosis) should alert the examiner to the possibility of
retroperitoneal bleeding, which was found on CT scan in this
hemophiliac patient. (Courtesy of Louis LaVopa, MD.)
|
|
Differential Diagnosis
Diagnostic suspicion and
awareness of the above conditions is the most important step leading to
the correct diagnosis. HSP, mongolian spots, and cultural practices such
as moxibustion and cupping are diagnosed clinically. If ITP or other
thrombocytopenic disorders are suspected, a platelet count is diagnostic.
Newborns and infants with significant bleeding should have PT and PTT
tests to rule out a coagulopathy.
Emergency Department Treatment
and Disposition
A hematologist should be consulted
for children with platelet disorders and coagulopathies. HSP requires
supportive care and close follow-up. The most serious complication of HSP
is bowel obstruction from intussusception.
Clinical Pearls
1. Mongolian spots are noted
first in the newborn period.
2. Consider HSP in school-age
children with purpura of the lower extremities.
3. Consider ITP in preschool
children who have multiple ecchymosis and petechiae without other signs
or indications of abuse.
4. Vitamin K deficiency is a
cause of bleeding in infancy.
5. Trauma to the forehead may
cause bilateral eye ecchymosis (Fig. 15.22) within a few days and can be
mistaken for eye trauma.
|
|
|

|
|
Raccoon
Eyes, or Black Eyes The
etiology of this child's raccoon eyes was a forehead hematoma. He
fell onto his forehead a few days earlier and developed a hematoma, a
common accidental injury. As the hematoma healed, blood from the
hematoma tracked down along the facial soft tissues and settled under
his eyes. The resulting ecchymosis suggests that he was punched,
leaving him with two black eyes. The absence of other trauma about
the eyes—such as lacerations, abrasions, soft tissue swelling,
or eye injury—should cause the examiner to consider a diagnosis
other than direct trauma. Observation or palpation of forehead soft
tissue swelling results in the correct diagnosis. (Courtesy of Robert
A. Shapiro, MD.)
|
|
|
|
Fractures Suggestive of Abuse
Associated Clinical Features
Certain fractures should always
raise a suspicion of child abuse, such as metaphyseal corner fractures,
rib fractures, fractures in a nonambulating child, and untreated healing
fractures. Fractures incompatible with the history and those for which no
explanation is available are also suspicious of child abuse (Figs. 15.23,
15.24, 15.25, 15.26, 15.27, 15.28, and 15.29).
|
|
|

|
|
Healing
Corner Fracture This
radiograph shows a healing metaphyseal corner fracture of the
proximal tibia, sometimes referred to as a bucket-handle fracture.
Arrows point to the impressive periosteal elevation, causing the
bucket-handle appearance. This fracture is most often seen in
children who have been the victims of child abuse, the result of
shaking or pulling. (Courtesy of Alan E. Oestreich, MD.)
|
|
|
|
|

|
|
Healing
Corner Fracture Periosteal
reaction (arrow) of the distal tibia from a corner fracture.
(Courtesy of Alan E. Oestreich, MD.)
|
|
|
|
|

|
|
Spiral
Femur and Proximal Tibia Fracture
This radiograph shows a displaced spiral femur fracture with faint
callus formation. The age of the fracture is just over 10 days. There
is also periosteal reaction of the proximal tibia, which is more
solid and therefore older than the femur fracture. Spiral femur
fractures are caused by trauma that includes a twisting, rotational
force to the bone. Accidental falls can result in spiral fractures if
the child's foot is fixed while his or her body is rotating. Spiral
fractures from abuse are often caused by an angry adult who twists
the leg of the child. The radiographic finding in this photograph is
almost certainly indicative of child abuse because there are two
injuries which occurred at different times and no treatment was
obtained when the injuries occurred. (Courtesy of Alan E. Oestreich,
MD.)
|
|
|
|
|

|
|
Healing
Fracture of the Distal Humerus
The periosteal reaction along the distal humerus dates this fracture
as older than 10 days. No treatment was obtained for the acute
injury. (Courtesy of Alan E. Oestreich, MD.)
|
|
|
|
|

|
|
Multiple
Healing Rib Fractures There
are healing rib fractures of the right posterior fifth, sixth, and
seventh ribs, the right lateral sixth rib, the left posterior fourth
rib, and the right proximal humerus. The surrounding callus indicates
the fractures are older than 10 days. Rib fractures must always raise
a suspicion of child abuse since accidental rib fractures are
unusual. Rib fractures are usually due to very firm squeezing and may
be seen with shaken baby syndrome. Normal handling of infants or
playful activities do not cause rib fractures. (Courtesy of Alan E.
Oestreich, MD.)
|
|
|
|
|

|
|
Compression
Fracture The wedging of T-12 (arrow)
and probably L-1 indicates vertebral compression fractures. These
fractures are the result of significant forces applied to the spinal
column and are often indicative of child abuse. (Courtesy of Alan E.
Oestreich, MD.)
|
|
|
|
|

|
|
"Bucket-Handle"
Fracture Metaphyseal fractures
may appear as in this photograph. When captured at this angle, the
fracture is frequently described as a bucket-handle fracture.
(Courtesy of Michael P. Poirier, MD.)
|
|
Differential Diagnosis
Normal pediatric radiographic
variants, periosteal changes caused by conditions other than healing
fractures, and illnesses that cause fragile bones may all be mistaken for
fractures due to child abuse. A pediatric radiologist should be consulted
if any doubt exists about the radiographic interpretation. Specific
disorders that can be mistaken for child abuse include osteogenesis
imperfecta, copper deficiency, osteopetrosis, rickets, scurvy,
hypervitaminosis A, osteomyelitis, tumors, leukemia, prostaglandin E
overdose, and Caffey's infantile cortical hyperostosis.
Conditions that cause
"brittle bones" must be considered when unexpected fractures
are discovered, even though such cases are rare. The most frequently
discussed brittle bone disorder is osteogenesis imperfecta (OI), a rare
inherited connective-tissue disorder. Associated features seen in some
children with OI include blue sclerae, wormian bones (seen on the skull
x-ray), and osteopenia. A family history of bone fragility, hearing loss,
and short stature is often present. In rare instances, children with OI
lack these associated features.
Emergency Department Treatment
and Disposition
If abuse is suspected in a child
under 2 or 3 years of age, obtain a skeletal survey. The skeletal survey
should include a minimum of 19 films (Table 15.1), including frontal
views of the appendicular skeleton and frontal and lateral views of the
axial skeleton. Coned down views over a joint may be needed for best
visualization of metaphyseal injuries. Oblique views are useful for hand,
rib, and nondisplaced lone bone-shaft fractures. All images obtained
(including those of the chest) should use bone technique. Ideally, all studies
should be read by a radiologist while the patient is still in the ED.
Consider computed tomography or magnetic resonance imaging of the head in
infants with skull fractures when abuse is suspected. Suspected abuse
must be reported immediately to the appropriate child protection agency.
Fractures should be managed appropriately.
|
Table 15.1 Skeletal Survey for
Suspected Child Abuse
|
|
|
AP skull
|
|
Lateral
skull
|
|
Lateral
cervical spine
|
|
AP thorax
|
|
Lateral
thorax
|
|
AP pelvis
|
|
Lateral
lumbar spine
|
|
AP humeri (2)a
|
|
AP
forearms (2)a
|
|
Oblique
hands (15°–20°) (2)a
|
|
AP femurs
(2)a
|
|
AP tibias
(2)a
|
|
AP feet
(2)a
|
|
|
a Each a separate exposure: can be combined on one
film.
Source: Courtesy of Paul Kleinman, MD.
|
Clinical Pearls
1. Suspect abuse when a child
has multiple fractures, fractures of different ages, unsuspected (occult)
fractures, or fractures without a consistent trauma history.
2. Accidental trauma that
includes rotational forces can result in a spiral fracture.
3. Obtain a skeletal survey in any
child under 2 years of age who has injuries suspicious of abuse.
4. Radiographic signs of
healing are typically first seen 10 days after a fracture.
5. Fractures that are not
immobilized have a larger callus than immobilized fractures.
|
|
Shaken Baby Syndrome
Associated Clinical Features
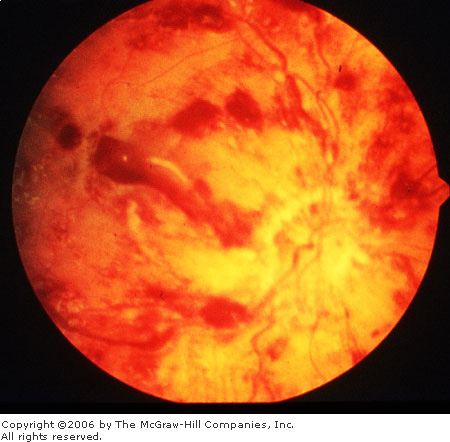
Infants who are violently shaken
may suffer intracranial injury, commonly referred to as "shaken baby
syndrome." Typically, the infant is held by the chest and violently
shaken back and forth. This shaking results in subdural hemorrhages and
cerebral contusions (Figs. 15-30, 15-31, and 15-32). Most of the victims
are under 1 year of age. Some investigators believe that shaking alone is
insufficient to cause these injuries and that therefore some blunt head
trauma must also occur. The name "shaken impact syndrome" has
been suggested to include this mechanism. There are usually no external
signs of trauma, although infants who are shaken may also have fractures,
abdominal trauma, bruises, and other injuries. Neurologic symptoms such
as apnea, seizures, irritability, or altered mental status are commonly
seen but may be absent. Retinal hemorrhages (Figs. 15.33, 15.34) are seen
in 80% of shaken babies. The hemorrhages may be unilateral or bilateral.
Shaken baby syndrome should be strongly considered when retinal
hemorrhages are found in any child under 2 years of age.
|
|
|
|
|
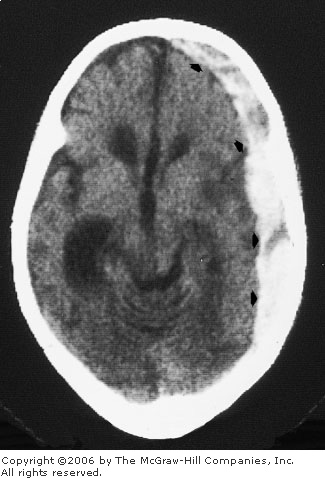
Acute
Subdural Hematoma There is a
crescent-shaped, hyperdense collection, indicating an acute subdural
hematoma over the left cerebral hemisphere (arrows). In
addition, the brain demonstrates chronic injury from a previous
insult, which left the child severely impaired. (Courtesy of William
S. Ball, MD.)
|
|
|
|
|
|
|
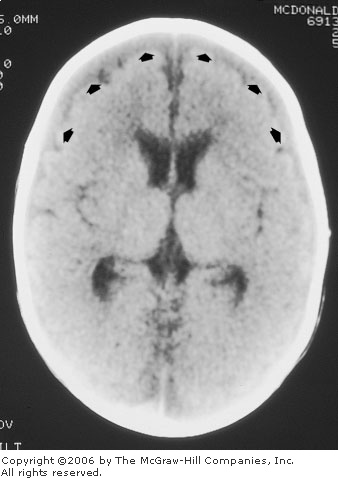
Subacute
Brain Injury from Shaken Baby Syndrome This noncontrast computed tomography scan
demonstrates bilateral subdural collections over the frontal
convexity (arrows). (Courtesy of William S. Ball, MD.)
|
|
|
|
|

|
|
Old
Brain Injury from Shaken Baby Syndrome Three months later there is evidence of
diffuse cerebral volume loss with multifocal areas of increased
density (arrows), representing diffuse cortical and
subcortical injury. (Courtesy of William S. Ball, MD.)
|
|
|
|
|
|
|
Retinal
Hemorrhage Multiple retinal
hemorrhages are present. (Courtesy of Rees W. Shepherd, MD.)
|
|
|
|
|

|
|
Retinal
Hemorrhages Multiple discreet
subhyaloid hemorrhages seen on funduscopic examination in an infant
with shaken baby syndrome. (Courtesy of John D. Baker, MD, and Massie
Research Laboratories, Inc.)
|
|
Differential Diagnosis
Shaken baby syndrome is the most
common cause of intracranial injury in infants. Relatively minor trauma,
such as a fall off a couch or bed, should not cause intracranial damage
unless there are predisposing conditions such as a bleeding disorder or a
preexisting intracranial vascular disorder. Retinal hemorrhages in
association with intracranial trauma is almost always indicative of
shaken baby syndrome.
Findings on computed tomography
(CT) or magnetic resonance imaging (MRI) that may mimic SBS include
benign extraoral fluid collections, glutaric aciduria type, ruptured
aneurysm, or arteriovenous malformation.
Retinal hemorrhages may be caused
by birth trauma, blunt eye trauma, meningitis, severe hypertension,
sepsis, and coagulopathies. The hemorrhages that result from birth
usually resolve within 3 weeks. There have been reports of
cardiopulmonary resuscitation (CPR) causing retinal hemorrhages. Retinal
hemorrhages from CPR and mechanisms other than major trauma are typically
less extensive than those seen in SBS.
Emergency Department Treatment
and Disposition
CT or MRI of the head should be
obtained and the patient treated in the usual fashion. A report of
suspected child abuse must be made to the child protective agency. A
skeletal survey should also be obtained and other injuries noted (Fig.
15.35). An ophthalmologist should follow the patient's retinal injuries.
|
|
|

|
|

|
|
Bruises This child was a victim of shaken baby
syndrome (SBS). Unlike most victims of SBS, he also has signs of
cutaneous injury. Bruises on his right pinna (A) and left upper arm
(B) were noted on examination. (Courtesy of Robert A. Shapiro, MD.)
|
|
Clinical Pearls
1. Child abuse should be
suspected in any infant with retinal hemorrhages or facial bruising.
2. Infants with SBS may have no
external signs of trauma and minimal neurologic deficits.
3. When retinal hemorrhages are
present, an ophthalmologist should be consulted to assist with the
differential diagnosis and for medicolegal documentation.
4. SBS is most common in
children under 1 year of age.
|
|
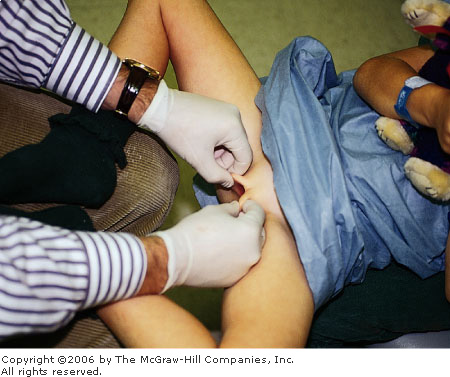
Examination Techniques and Normal Findings
Associated Clinical Features
The genital examination of
prepubertal girls is usually limited to inspection of the external
genitalia and hymen for injury and infection. An internal inspection is
rarely required. Children should first be examined in the
"frog-leg" position. The child can lie on the examination table
or sit on a parent's lap (Fig. 15.36), whichever makes her most
comfortable. Position the patient in a supine position with her knees
flexed and out. The soles of her feet should be opposed (Fig. 15.36).
Alternatively, the child can be placed in a knee-chest position. The
knee-chest position is particularly useful to visualize foreign bodies in
the vagina as well as the posterior vaginal rim.
|
|
|
|
|
Child
Sitting in Mother's Lap for Genital Examination This young girl is being examined while she
sits in her mother's lap. Many young children are less fearful of the
examination if they are held by a parent during the examination. Her
legs are held in the "frog-leg" position as labial traction
is applied. (Courtesy of Robert A. Shapiro, MD.)
|
|
First, examine the perineum for trauma, condylomata,
herpetic lesions, or discharge. Next examine the hymen. To visualize the
hymen, hold the labia majora between the thumb and index fingers of each
hand. Apply lateral and posterior traction to the labia while pulling
them outward (Fig. 15.37). When done properly, this procedure is not
painful and provides excellent visualization of the hymen (Figs. 15-38,
15-39, and 15-40). If the hymen cannot be visualized in the supine
frog-leg position, the knee-chest position should be attempted (Fig.
15.41). Examine the hymen for indications of trauma, such as swelling,
ecchymoses or tears. In pubertal girls, a Foley catheter can help the
examiner inspect the edges of the hymen for injury (Fig. 15.42). To
perform this procedure, insert the deflated catheter into the vagina and
inflate the catheter balloon with 10 mL of saline. Gentle traction can
then be placed on the catheter by pulling until the balloon expands the
hymenal edges. By moving the inflated balloon from side to side to
different sections of the hymen can be exposed.
|
|
|
|
|
Labial
Traction Examination Techniques
Hymenal inspection in prepubertal girls is best accomplished in the
supine position when lateral (1) and posterior (2) traction to the
labia is applied as shown here. (Adapted from Giandino AP et al: A
Practical Guide to the Evaluation of Sexual Abuse in the Prepubertal
Child. Sage Publications, 1992.)
|
|
|
|
|

|
|
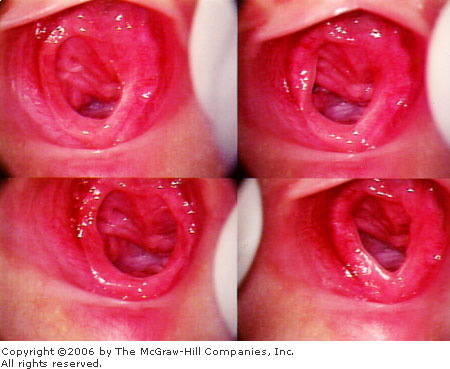
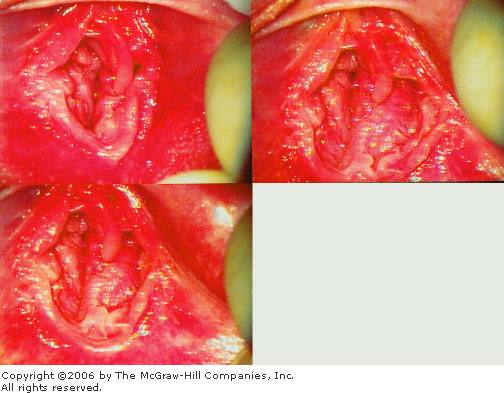
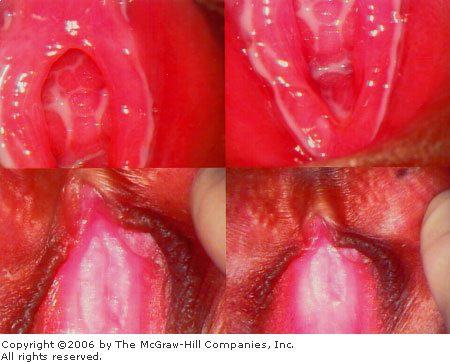
Effect
of Labial Traction on the Appearance of the Prepubertal Introitus These photographs demonstrate how the
appearance of the introitus changes using different examination
techniques in a prepubertal girl. Each photograph shows the introitus
of the same child as different types of labial traction are used. A.
Bottom right: Lateral labial traction only. The hymenal introitus
is closed and the hymenal margins cannot be visualized. B. Bottom
left: More aggressive lateral traction is applied. The introitus
is now partially visible. C. Top right and left: Lateral,
posterior, and caudal labial traction (as illustrated in 15.37). The
introitus is now clearly seen, and the hymen can be adequately
inspected for signs of injury. (Courtesy of Robert A. Shapiro, MD.)
|
|
|
|
|
|
|
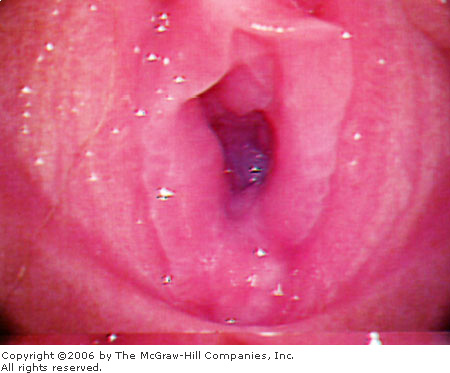
Redundant
Hymenal Tissue These
photographs show the genitalia of the same patient. Because of
redundant hymenal tissue, the introitus appears asymmetric in the top
two photos as well as the bottom left. The text describes methods to
handle redundant hymen. When the hymen is no longer adherent to
itself, the introitus appears symmetric and normal. (Courtesy of
Robert A. Shapiro, MD.)
|
|
|
|
|
|
|
Normal
Pubertal Hymen The hymen is
thicker and more redundant in this pubertal child compared to a
prepubertal hymen. This redundancy is due to the effects of estrogen
and begins during puberty. The hymen at 6 o'clock is not adequately
documented by this photograph. Additional
examinations—discussed in the above text—should be used
to visualize the posterior hymen. (Courtesy of Robert A. Shapiro,
MD.)
|
|
|
|
|

|
|
Supine
and Prone Examination Image
(A) of this examination was obtained while the child was supine. The
posterior hymen at 6 o'clock appears to be very narrow. When the
child was examined in the prone (knee-chest) position (B), the 6
o'clock area, now at the top of the photo, is better seen and is
completely normal in appearance. (Courtesy of Robert A. Shapiro, MD.)
|
|
|
|
|
|
|
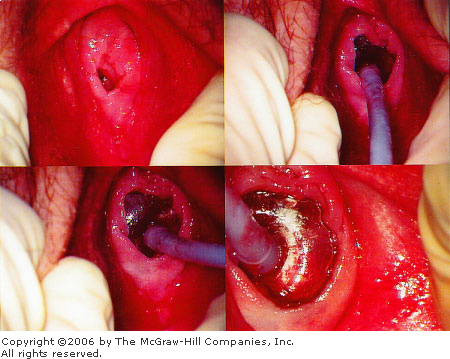
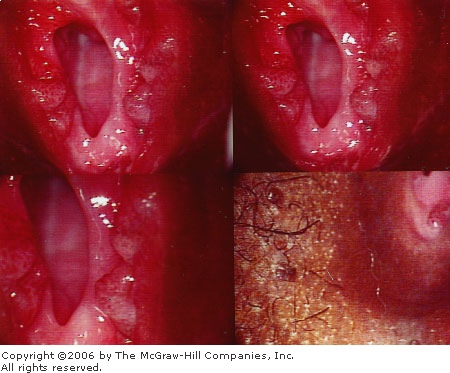
Foley
Catheter Technique A Foley
catheter inserted into the vaginal subsequently filled with 10 cc
saline is used to inspect the hymenal edges for injury. Gentle
traction and movement of the inflated balloon from side to side
exposes different sections of the hymen. The hymen shown in these
photographs is normal. (Courtesy of Robert A. Shapiro, MD.)
|
|
Techniques
Supine or "frog-leg"
position:
1. The child can lie on an
examination table or, if more comfortable, can sit on her parent's lap.
2. Position the child in a
supine position with her knees out and soles together.
3. Apply traction, as
demonstrated in Fig. 15.38.
Prone or knee-chest position:
1. On the examination table,
position the child on her hands and knees. Her knees should be spread
wider than her shoulders.
2. Have the child rest her
chest to the examination table.
3. Maintain the knee placement
with a swayed backbone.
Emergency Department Treatment
and Disposition
If sexual abuse is suspected, a
report of alleged sexual abuse must be made to the child protective
agency. Suspicious or abnormal examination findings should be documented.
The child should be referred for a definitive examination by an expert in
child abuse.
Clinical Pearls
1. Allow the child to sit on
her mother's lap during the examination if this makes her more
cooperative and less afraid.
2. Speculum examinations are
rarely indicated in prepubertal girls and are reserved for removal of an
intravaginal foreign body or evaluation of intravaginal trauma. General
anesthesia is often required before inserting a speculum into a
prepubertal child.
3. Apply caudal traction to the
labia during examination to prevent a superficial tear of the posterior
fourchette.
4. If a portion of the hymen
cannot be visualized because it is adherent to the adjacent labia or to
itself, gently touch the adherent tissue with the contralateral labia to
pull it free. A drop of saline placed onto the posterior hymen may also
separate adherent tissues without causing discomfort to the child.
5. The inner hymenal ring is
usually smooth and uninterrupted. Notches at 3 and 9 o'clock are normal.
6. The shape and appearance of
the normal prepubertal hymen is variable. Annular (Fig. 15.43) and crescentic
(Fig. 15.44) configurations are the most common. Normal hymens may also
be septate (Fig. 15.45), imperforate (no central opening), or cribriform
(multiple small openings).
7. A normal examination does
not exclude sexual abuse. The majority of abused prepubertal girls have
normal genital examinations. Examination findings specific for sexual
abuse are found in approximately 10 to 20% of girls who allege abuse.
|
|
|
|
|
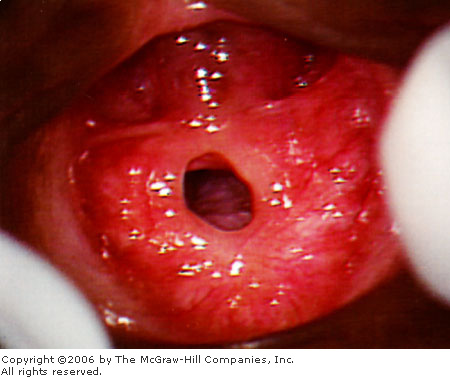
Normal
Annular Hymen The hymen in
this prepubertal girl is annular in shape, extending completely
around the vaginal opening. The inner hymenal ring (introitus) is
smooth and free of any defects, such as lacerations or scars. The
color of the hymen is more deeply red than seen in pubertal women and
does not necessarily indicate infection or trauma. (Courtesy of
Robert A. Shapiro, MD.)
|
|
|
|
|
|
|
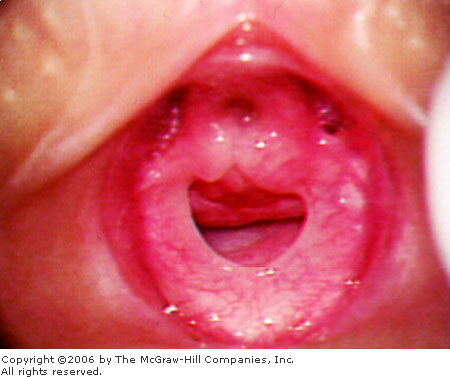
Normal
Crescentic Hymen The hymen in
this prepubertal girl extends from 2 to 10 o'clock and is absent
beneath the urethra between 10 and 2 o'clock. This annular shape is
very common and should not be mistaken for trauma or rupture of the
superior (2 to 10 o'clock) section. The inner hymenal ring (the
introitus) is smooth and free of any defects, such as lacerations or
scars. (Courtesy of Robert A. Shapiro, MD.)
|
|
|
|
|
|
|
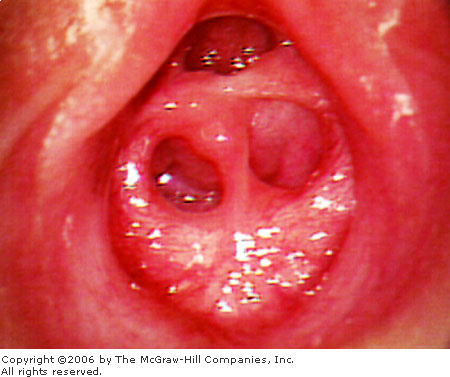
Normal
Septate Hymen This prepubertal
girl has a septum in the center of her introitus. Hymenal septa are
rarely seen after puberty. (Courtesy of Robert A. Shapiro, MD.)
|
|
|
|
Injuries and Findings Due to Sexual Abuse
Associated Clinical Features
Sexual abuse must be considered
in any child with a genital or rectal injury, a sexually transmitted
infection, a history of alleged abuse, or symptoms or behaviors seen in
abused children.
Acute injuries include
lacerations, bruises, abrasions and swelling (Figs. 15-46, 15-47, 15-48,
and 15-49). Acute injuries heal quickly, often within a few days to a
week. Nonacute findings of trauma secondary to sexual abuse can be more
difficult to recognize and should be considered by a child abuse expert.
Nonacute findings include scars, absent hymen, abnormal clefts (Fig.
15.50), and anal changes. Accurate interpretation of genital findings is
dependent on examination technique (see preceding section for suggestions
on examination technique).
|
|
|
|
|
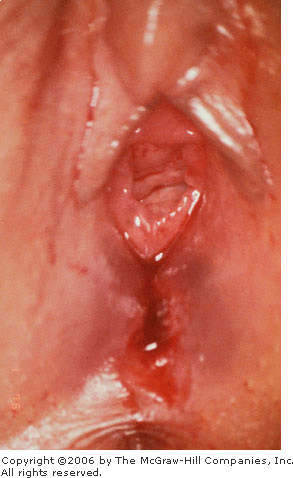
Hymenal
Injury Healed injuries to the
vaginal introitus have caused significant distortion of the anatomy.
The vaginal opening is gaping revealing multiple vaginal rugae. Only
small remnants of the hymen remain.
|
|
|
|
|
|
|
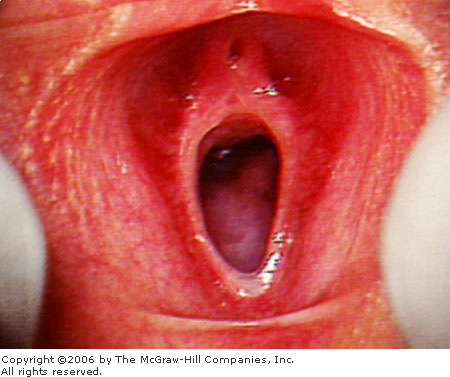
Hymenal
Laceration An acute laceration
with bruising of the posterior fourchette. The nearby hymen is
edematous and ecchymotic. This injury is most likely less than 72 h
old. Injuries to the hymen and posterior fourchette are usually
indicative of sexual assault. Forensic specimens should be collected
after acute sexual assault when the history or examination findings
suggest that semen, saliva, hair, or blood from the perpetrator might
be recovered from the victim. (Courtesy of Robert A. Shapiro, MD.)
|
|
|
|
|

|
|
Acute
Rectal Trauma An acute rectal
injury is visible at 12 o'clock. The perianal skin may normally be
darker, with red or blue coloration, than the surrounding skin.
(Courtesy of Robert A. Shapiro, MD.)
|
|
|
|
|

|
|
Acute
Hymenal Trauma There is a deep
laceration of the hymen at 7 o'clock and ecchymosis of the hymen at 6
o'clock after recent sexual assault. (Courtesy of Robert A. Shapiro,
MD.)
|
|
|
|
|
|
|
Gaping
Introitus, Absent Hymen The
hymen is almost totally absent in this prepubertal girl. There may be
a slight rim of hymen at 6 o'clock. The hymen in young girls is often
very thin and may be totally destroyed after vaginal penetration.
(Courtesy of Robert A. Shapiro, MD.)
|
|
Sexually transmitted infections diagnosed in a young
person may indicate sexual abuse (Fig. 15.51). Children infected with Neisseria
gonorrhoeae, Chlamydia trachomatis, Trichomonas, and syphilis (Fig.
15.52) who did not become infected through perinatal transmission have
almost certainly been infected through sexual contact. Condylomata
acuminata (genital warts) (Fig. 15.53) and herpes simplex may be
transmitted through sexual or nonsexual contact, so that sexual abuse as
well as other mechanisms should be considered.
|
|
|
|
|
Vaginal
Discharge Copious white
discharge is present in this photograph. Vaginal discharge in a
prepubertal child may be an indication of an STD. All children with
vaginal discharge should be cultured for N. gonorrhoeae and Chlamydia.
(Courtesy of Robert A. Shapiro, MD.)
|
|
|
|
|

|
|
Perirectal
Condyloma Lata (Secondary Syphilis) Perirectal condyloma lata are visible around the rectum.
(Courtesy of Robert A. Shapiro, MD.)
|
|
|
|
|

|
|
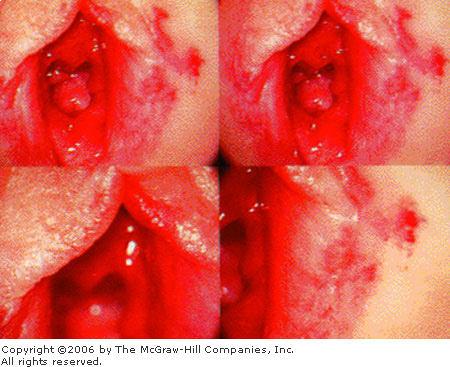
|
|
Perirectal
Condylomata Acuminata (Warts)
Multiple perianal (A) and perihymenal (B) condyloma acuminata are
visible in these photographs. Both individual and multidigitate
lesions are seen. The hymen appears to be normal. (Courtesy of
Charles J. Schubert, MD.)
|
|
All children who allege sexual
abuse should be evaluated, treated, and protected from the alleged
perpetrator. Because of threats by family members or the perpetrator, it
is not unusual for a child to recant initial allegations of sexual abuse.
Although uncommon, some children falsely allege sexual abuse. The
determination of whether allegations are false or of the significance of
recantation should be made by the child protective services worker or by
law enforcement, not by the emergency physician.
Behaviors or symptoms of abuse
are frequently absent at the time of diagnosis but can include fear or
avoidance of an individual, genital or rectal pain, sleep disorders,
regression, enuresis, encopresis, sexual acting out or promiscuity,
depression, declining in school performance, and perpetration of sexual
abuse on younger victims.
Differential Diagnosis
Injury to the hymen from an event
other than sexual abuse is possible though unusual. Masturbation and
self-exploration do not cause vaginal injury in the vast majority of
children. Subtle findings of hymenal trauma are difficult to recognize.
Normal hymenal anatomy may be misdiagnosed as trauma by inexperienced
examiners. Other genital findings mistaken for sexual abuse are listed in
the next section.
Emergency Department Treatment
and Disposition
Report suspected or alleged
sexual abuse to the appropriate child protection agency. Clearly document
all examination findings. If injuries require repair, appropriate
consultation with surgery or gynecology should be made. Culture for
sexually transmitted infections if there is a vaginal or urethral
discharge. If the history of abuse suggests a risk for infection, obtain
cultures from the genitalia, rectum, and pharynx. Consider syphilis and
HIV testing. Obtain forensic specimens if the alleged abuse occurred
within the previous 72 h and the examination findings or history suggests
that blood, semen, saliva, or hair of the perpetrator might be found on
the victim's body. Offer sexually transmitted disease (STD) and pregnancy
prophylaxes when indicated. Make discharge plans in consultation with the
child protection worker so that the child is not returned to the abusive
environment.
Clinical Pearls
1. It is not necessary to
measure the vaginal opening of prepubertal girls. The size of the
introitus is dependent on examination technique, degree of patient
relaxation, patient age, and other variables. There is no consensus on
normal introitus size among experts.
2. Hymenal notches at 3 and 9
o'clock can be a normal finding.
3. Changes to the posterior
hymen, such as narrowing and notching, may be indicative of penetrating
injury.
4. Rectal abuse often results
in no visible trauma. When trauma does occur, healing may be complete
within 1 to 2 weeks, leaving no visible indication of the injury.
5. The external anus is darker
in color than the rest of the skin and should not be mistaken for
erythema from abuse or infection.
6. Consider sexual abuse when
significant anal fissures are present on examination.
7. Condyloma lata (syphilis)
can be mistaken for condylomata acuminata (warts).
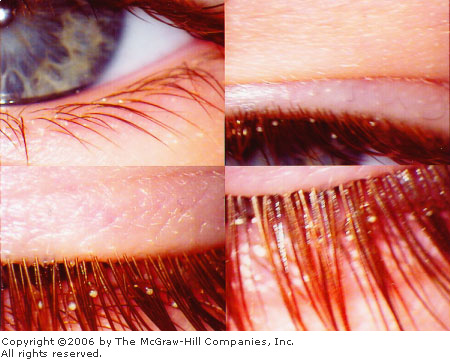
8. Vaginal discharge in a
prepubertal child should always be cultured for Neisseria gonorrhoeae
and Chlamydia.
9. When nits are observed in
the eyelashes of children (Fig. 15.54), the infecting louse is the pubic
louse. The mode of transmission must be sought and sexual abuse must be
suspected.
|
|
|
|
|
Nits
Nits (the larval form of the
louse) from Phthirus pubis are seen firmly adherent to the
eyelashes in this child. Sexual abuse should be considered. (Courtesy
of Robert A. Shapiro, MD.)
|
|
|
|
Straddle Injury
Associated Clinical Features
Straddle injuries are a frequent
cause of genital trauma and most often result in unilateral abrasions,
bruising, and hematomas of the labia majora and clitoral hood (Fig.
15.55). A clear history describing the straddle injury should be given by
the caretaker.
|
|
|

|
|
Straddle
Injury Laceration of the
clitoral hood due to a fall onto the bar of a bicycle. (Courtesy of
Robert A. Shapiro, MD.)
|
|
Differential Diagnosis
Sexual abuse must be considered
in all children with genital injuries. Injuries involving the hymen are
not typical of straddle injuries and are usually the result of sexual
abuse or assault.
Emergency Department Treatment
and Disposition
Check for urethral injury. Sitz
baths and Polysporin ointment promote healing and minimize discomfort. If
the child has difficulty voiding, she should be encouraged to void in a
bath of warm water.
Clinical Pearls
1. Straddle injuries usually
present with a clear mechanism of injury and a physical examination that supports
the history.
2. Straddle injuries do not
typically involve the hymen or internal vaginal mucosa.
|
|
Labial Adhesions
Associated Clinical Features
Adhesions of the labia minora
occur in young girls and may persist until puberty. A thin translucent line
is seen where the labia meet (Fig. 15.56). The extent of the adhesions
varies from child to child. Involvement is often limited to the posterior
portion of the labia, but some children have more extensive adhesions
completely obscuring the introitus. It is postulated that vulvar
irritation and poor hygiene contribute to the etiology of labial
adhesions.
|
|
|

|
|
Labial
Adhesions Labial adhesions
obscure the hymen in this prepubertal girl. (Courtesy of Robert A.
Shapiro, MD.)
|
|
Differential Diagnosis
The hymen and introitus may be
obscured by the adhesions. If the adhesions are unrecognized, a diagnosis
of hymenal trauma and "gaping" introitus may be incorrectly
made. Adhesions may be mistaken for vaginal scars.
Emergency Department Treatment
and Disposition
Estrogen cream (Premarin) can be
prescribed and applied gently over the adhesions twice daily for 2 to 4
weeks. Recurrence is not uncommon.
Clinical Pearls
1. Adhesions may be congenital
or acquired.
2. It is postulated that vulvar
irritation from sexual abuse may cause labial adhesions, but clear
supporting evidence is lacking.
|
|
Urethral Prolapse
Associated Clinical Features
Prepubertal girls with urethral
prolapse present with vaginal bleeding, vaginal mass, or urinary
complaints. On examination, an annular, erythematous vaginal mass is seen
(Fig. 15.57). Upon close examination, the mass can be seen to originate from
the urethra. If necrotic, the mass is friable.
|
|
|

|
|
Urethral
Prolapse A round
reddish-purple mass is seen in this child's introitus. Careful
examination reveals that the mass originates from the urethra.
(Courtesy of Michael P. Poirier, MD.)
|
|
Differential Diagnosis
Urethral prolapse may be mistaken
for vaginal injury, sexual abuse, or vaginal mass.
Emergency Department Treatment
and Disposition
The prolapse may resolve within a
few weeks with conservative medical management consisting of daily sitz
baths and topical antibiotics. Topical estrogen cream and oral antibiotic
therapy have also been used with some success. Surgical repair is usually
not required but may be indicated if necrosis is present or conservative
management fails.
Clinical Pearls
1. Urethral prolapse often
presents with painless genital bleeding of unknown etiology.
2. Prolapse is more common in
African American girls.
|
|
Toilet Bowl Injury
Associated Clinical Features
Acute bruising to the glans and
corona of the penis can occur if the toilet seat falls onto the penis
during voiding, trapping the penis between the seat and toilet bowl (Fig.
15.58). This injury is not uncommon in boys of about 3 years of age who
are both inexperienced at voiding while standing and are short enough for
this injury to occur.
|
|
|

|
|
Toilet
Bowl Injury This toddler
presented with a straightforward history of the toilet seat falling
onto his penis during voiding. Despite the swelling and ecchymosis,
he was able to void without difficulty. (Courtesy of Kevin J. Knoop,
MD, MS.)
|
|
Differential Diagnosis
Genital trauma is always
suspicious for sexual abuse. The mechanism of injury may be difficult to
determine if the injury was unwitnessed.
Emergency Department Treatment
and Disposition
No specific treatment is needed
unless the child is unable to void. If the child cannot void, a
retrograde urethrogram and urologic consult are indicated.
Clinical Pearl
1. Genital injuries are
suspicious of sexual abuse if no appropriate history of accidental trauma
is given.
|
|
Perianal Streptococcal Infection
Associated Clinical Features
Presenting complaints are often
rectal pain, itching, bleeding, and rash. Symptoms may be present for
months prior to the diagnosis. The child may be constipated because of
stool retention and may have recently been given laxatives because of
these symptoms. Systemic symptoms are absent. The perianal area is
erythematous and tender (Fig. 15.59). The involved area is well
demarcated from the uninfected skin. Anal fissures and bleeding may be
seen.
|
|
|

|
|
Perianal
Streptococcal Infection
Intense erythema around the anus consistent with perianal
streptococcal infection. (Courtesy of Raymond C. Baker, MD.)
|
|
Differential Diagnosis
Sexual abuse is often
misdiagnosed because of the child's complaints of rectal pain and
bleeding and the above findings on examination. This infection can also be
mistaken for poor hygiene, dermatitis, nonspecific irritation, and
constipation.
Emergency Department Treatment
and Disposition
Culture or obtain direct antigen
studies for group A beta-hemolytic streptococci. Treat with oral
penicillin for 10 days. Substitute erythromycin for patients allergic to
penicillin. Treatment failures should be treated with IM penicillin
and/or oral clindamycin.
Clinical Pearls
1. Direct antigen studies are
sensitive (89%) and specific (100%) for perianal group A streptococcal infection.
2. Examine the pharynx for
streptococcal infection when considering perianal strep infection.
3. Infection is unusual in
children older than 10 years.
|
|
Lichen Sclerosus Atrophicus
Associated Clinical Features
Lichen sclerosus atrophicus (LSA)
is an unusual dermatitis that affects the anogenital area. The diagnosis
should be suspected whenever an area of hypopigmentation in the shape of
an hourglass is seen around the child's anus and genitalia. The
hypopigmented area is caused by small white or yellowish papules which
coalesce into large plaques. The affected skin is atrophic and bleeds
easily after minor trauma. The hemorrhagic form of LSA includes
subepithelial hemorrhagic lesions to the labia and affected skin, which
can be mistaken for traumatic lesions (Fig. 15.60). Children may complain
of pruritus and dysuria.
|
|
|
|
|
Lichen
Sclerosus Atrophicus The perineum
surrounding the vagina has a bruised appearance. Atrophic skin is
also evident. (Courtesy of Robert A. Shapiro, MD.)
|
|
Differential Diagnosis
The findings of hemorrhage around
the genitalia and rectum are often mistaken for signs of sexual abuse.
Emergency Department Treatment
and Disposition
Use symptomatic treatment if
needed; 1%hydrocortisone cream can be prescribed. Refer to dermatologist
for treatment.
Clinical Pearl
1. Lichen sclerosus atrophicus
is the most common dermatitis mistaken for sexual abuse.
|
|