|
Note: Large images and
tables on this page may necessitate printing in landscape mode.
Copyright
©2006 The McGraw-Hill Companies. All rights reserved.
Emergency
Medicine Atlas > Part 1. Regional
Anatomy > Chapter 4. Ophthalmic Trauma >
|
Corneal Abrasion
Associated Clinical Features
Corneal abrasions are heralded by
the acute onset of eye discomfort accompanied by tearing and a
foreign-body sensation. Conjunctival injection may also be noted. If the
area of abrasion is large or central, visual acuity may be affected.
Large abrasions or delays in seeking care may be accompanied by
photophobia and headache from ciliary muscle spasm. Associated findings
or complications include traumatic iritis, hypopyon, or a corneal ulcer
(described in Chap. 2). Examination before and after instillation of
fluorescein, preferably with a slit lamp, usually reveals the defect
(Figs. 4.1 and 4.2). Fluorescein pools and stains the area where corneal
epithelium has been denuded.
|
|
|

|
|
Corneal
Abrasion Seen under
magnification from the slit lamp, corneal abrasion can sometimes be
appreciated without fluorescein staining. This abrasion is seen
without using the cobalt blue light. (Courtesy of Harold Rivera.)
|
|
|
|
|

|
|
Corneal
Abrasion The same abrasion as
Fig. 4.1 is seen under magnification from the slit lamp with
fluorescein stain using the cobalt blue light. (Courtesy of Harold
Rivera.)
|
|
Differential Diagnosis
Corneal foreign body,
conjunctivitis, conjunctival foreign body, iritis, and corneal ulcer can
present with similar complaints.
Emergency Department Treatment
and Disposition
Instillation of topical
anesthetic drops permits a better examination and relieves pain. A
short-acting cycloplegic (e.g., cyclopentolate 0.5%, homatropine 5%) may
reduce ciliary spasm and pain and should be considered in patients with
larger abrasions or in those who complain of headache or photophobia.
Topical antibiotic drops or ointment—preferably broad-spectrum
agents such as gentamicin, sulfacetamide, or erythromycin—are used
to prevent secondary bacterial infection. A soft double-layer patch may
also be applied. Neither treatment with topical antibiotics nor patching
has been scientifically validated, and routine use of these practices has
been called into question. Follow-up is required for any patient who is
still symptomatic after 12 h.
Clinical Pearls
1. Only sterile fluorescein
strips should be used, since the corneal epithelium, the primary barrier
to infection, has been potentially disrupted.
2. Mucus may simulate the
fluorescein uptake, but its position changes with blinking.
3. Multiple linear corneal
abrasions, the "ice-rink sign," may result from the adherence
of a foreign body to the conjunctiva under the lid (Fig. 4.3). The lid
should always be everted to rule out a retained foreign body.
4. A high index of suspicion of
a perforating injury should be maintained for any abrasion that occurs as
a result of grinding or striking metal on metal.
5. Fluorescein streaming away
from an "abrasion" (Seidel's test) may be an indication of a
corneal perforation.
|
|
|

|
|
Foreign
Body under the Upper Lid Lid
eversion is an essential part of the eye examination. (Courtesy of
Kevin J. Knoop, MD, MS.)
|
|
|
|
Corneal Foreign Body
Associated Clinical Features
Patients typically give a history
of something in the eye or complain of foreign-body sensation. If the
foreign body overlies the cornea, the patient's vision may be affected.
There may be tearing, conjunctival injection, and ciliary flush (Fig.
4.4). If several hours have elapsed since the occurrence of the injury,
there may be headache and photophobia in addition to the above signs and
symptoms.
|
|
|

|
|
Foreign
Body on the Cornea A foreign
body is lodged at 10 o'clock on the cornea. Note the localized
ciliary flush in the surrounding conjunctiva at the limbus. (Courtesy
of Kevin J. Knoop, MD, MS.)
|
|
Differential Diagnosis
The most important consideration
in the differential is the possibility of a penetrating injury to the
globe. A meticulous history about the mechanism of injury (grinding or
metal on metal) must be elicited. Conjunctival foreign body, corneal
abrasion, intraocular foreign body, conjunctivitis, iritis, and glaucoma
should also be considered.
Emergency Department Treatment
and Disposition
If superficial, removal of the
foreign body with a moist cotton-tipped applicator may be attempted; if
unsuccessful, an eye spud or small (25-gauge) needle may be used. After
removal, if a residual corneal abrasion is present, instill an antibiotic
solution or ointment. A "short-acting" cycloplegic (e.g.,
cyclopentolate 0.5%) should be considered in patients with complaints of
headache or photophobia. Metallic foreign bodies are often accompanied by
a "rust ring" discoloration of the surrounding corneal
epithelium (Fig. 4.5). Removal of the rust ring can be attempted, either
with a needle or preferably with a small burr drill device available
commercially. Alternatively, the patient may be referred to an
ophthalmologist the following day.
|
|
|

|
|
"Rust
Ring" A rust ring has
formed from a foreign body (likely metallic) in this patient. A burr
drill can be used for attempted removal, which, if unsuccessful, can
be reattempted in 24 h. (Courtesy of Kevin J. Knoop, MD, MS.)
|
|
Clinical Pearls
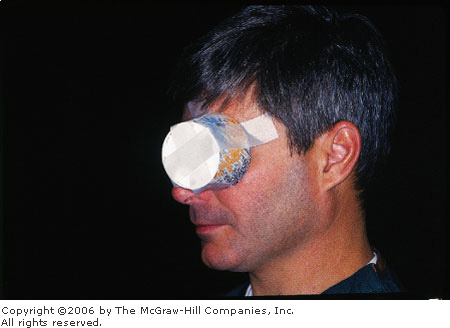
1. Treatment of a suspected
penetrating injury to the globe includes immediate referral, eye rest,
protective patching (Figs. 4.6, 4.7), and elevation of the head of the
bed.
2. If history of ocular
penetration is present, a diligent search for a foreign body is
indicated. X-ray may identify the foreign body (Fig. 4.8), but computed
tomography (CT) is the diagnostic study of choice.
3. Be sure to evert the upper
lid and search carefully for a foreign body. A foreign body adherent to
the upper lid abrades the cornea, producing the "ice-rink"
sign, caused from multiple linear abrasions.
4. If a rust ring is present
from a metallic foreign body, its removal can be attempted, or the
patient may await ophthalmology follow-up in 24 h.
5. Multiple small corneal
foreign bodies (e.g., glass or sand) may be removed by irrigating with
normal saline or tap water. The instillation of a topical anesthetic
facilitates the irrigation process.
|
|
|

|
|
Protective
Metal (Fox) Shield A
protective shield is used in the setting of a suspected or confirmed
perforating injury. (Courtesy of Kevin J. Knoop, MD, MS.)
|
|
|
|
|
|
|
Protective
Shield A protective shield is
readily fashioned from a paper cup if a metal shield is not
available. (Courtesy of Kevin J. Knoop, MD, MS.)
|
|
|
|
|

|
|
Intraocular
Foreign Body A metallic
foreign body is seen on a plain radiograph and—with comparison
with a lateral film—indicates the presence of an intraocular
foreign body. (Courtesy of Department of Ophthalmology, Naval Medical
Center, Portsmouth, VA.)
|
|
|
|
Eyelid Laceration
Associated Clinical Features
Eyelid lacerations should always
prompt a thorough search for associated injury to the globe, penetration
of the orbit, or involvement of surrounding structures (e.g., lacrimal
glands, ducts, puncta) (Fig. 4.9). Depending on the mechanism of injury,
a careful exclusion of foreign body may be indicated.
|
|
|
|
|
Eyelid
and Adnexa Anatomy Ocular
trauma should prompt examination of surrounding anatomic structures
for associated injuries.
|
|
Differential Diagnosis
Laceration of the levator
palpebrae musculature or tendinous attachments, laceration of the canthal
ligamentous support, division of the lacrimal duct or puncta, and
penetration of the periorbital septum should all be considered.
Emergency Department Treatment
and Disposition
Eyelid lacerations involving
superficial skin can be repaired with 6-0 nonabsorbable interrupted
sutures, which should remain in place for 3 days. Lacerations through an
anatomic structure called the gray line (see Fig. 4.9), situated on the
palpebral edge, require diligent reapproximation and should be referred.
Other injuries that require specialty consultation for repair include:
—Lacerations through the
lid margins: these require exact realignment to avoid entropion or
extropion.
—Deep lacerations through
the upper lid that divide the levator palpebrae muscles or their
tendinous attachments: these must be repaired with fine absorbable suture
to avoid ptosis.
—Lacrimal duct injuries:
these are repaired by stenting of the duct, otherwise excessive spilling
of tears (epiphora) will result.
—Medial canthal
ligaments: these must be repaired to avoid drooping of the lids.
The most important objectives are
to rule out injury to the globe and to search diligently for foreign
bodies.
Clinical Pearls
1. Lacerations of the medial
one-third of the lid (Fig. 4.10) should always raise suspicion for injury
to the lacrimal ducts or puncta as well as the medial canthal ligament.
2. A small amount of adipose
tissue seen within a laceration is a sign that perforation of the orbital
septum has occurred (since there is no subcutaneous fat in the lids
themselves).
3. Injuries involving the
orbital septum carry a higher than normal risk of globe injury and
intraorbital foreign body as well as a higher risk for orbital
cellulitis. A CT scan and specialty consultation should be considered.
4. Any injury to the lids
involving tissue loss or avulsion should be referred for specialty
consultation.
|
|
|

|
|
Eyelid
Laceration This laceration
involving the medial third of the lid clearly violates the
canalicular structures. The patient was struck by a person wearing a
ring. (Courtesy of Kevin J. Knoop, MD, MS.)
|
|
|
|
Hyphema
Associated Clinical Features
Injury to the anterior chamber
that disrupts the vasculature supporting the iris or ciliary body results
in a hyphema. The blood tends to layer and because of gravity forms a
meniscus (Fig. 4.11). Symptoms can include pain, photophobia, and
possibly blurred vision secondary to obstructing blood cells. Nausea and
vomiting may signal a rise in intraocular pressure (glaucoma) caused by
blockage of the trabecular meshwork by blood cells or clot.
|
|
|

|
|
Hyphema This hyphema has almost completely layered
while the patient's head was tilted. Note the hazy greenish area at 6
o'clock in contrast to the remainder of the blue iris. This
represents blood circulating in the anterior chamber that has not yet
layered. (Courtesy of Kevin J. Knoop, MD, MS.)
|
|
Differential Diagnosis
Hypopyon (pus within the anterior
chamber), vitreous hemorrhage, iridodialysis, penetrating injury to the
globe, and intraocular foreign body should be considered.
Emergency Department Treatment
and Disposition
Prevention of further hemorrhage
is the first goal. The patient should be kept at rest in the supine
position with the head elevated slightly. A hard eye shield should be
used to prevent further trauma from manipulation. Oral or parenteral pain
medication and sedatives are appropriate, but avoid agents with antiplatelet
activity such as nonsteroidal anti-inflammatory drugs (NSAIDs).
Antiemetics should be used if the patient has nausea. Further treatment
is at the discretion of specialty consultants but may include topical and
oral steroids, antifibrinolytics such as aminocaproic acid, or surgery.
Intraocular pressure (IOP) should be measured in all patients unless
there is a suspicion of penetrating injury to the globe. If elevated, IOP
should be treated with appropriate agents including topical beta
blockers, pilocarpine, and, if needed, osmotic agents (mannitol,
sorbitol) and acetazolamide. The need for admission for small hyphemas is
variable, since some centers admit all whereas others individualize
treatment. Ophthalmologic consultation is warranted to determine local
practices.
Clinical Pearls
1. The patient should be told
specifically not to read or watch television, as these activities result
in greater than usual ocular activity.
2. Depending on the severity of
the initial hyphema, rebleeding may occur in 10 to 25% of patients,
commonly in 2 to 5 days as the original clot retracts and loosens.
3. Blood that is not absorbed
from the anterior chamber may infiltrate and stain the cornea, leaving a
brown discoloration.
4. An "eightball" or
total hyphema occurs when blood fills the entire anterior chamber. These
lesions require surgical evacuation.
5. Patients with sickle cell
and other hemoglobinopathies are at risk for sickling of blood inside the
anterior chamber (Fig. 4.12). This can cause a rise in IOP from physical
obstruction of the trabecular meshwork.
|
|
|

|
|
|
|
Hyphema A small hyphema (about 5%) in a patient with
sickle cell disease. (Courtesy of Dallas E. Peak, MD.)
|
|
|
|
Iridodialysis
Associated Clinical Features
Traumatic iridodialysis is the
result of an injury, typically blunt trauma, that pulls the iris away
from the ciliary body. The resulting deformity appears as a lens-shaped
defect at the outer margin of the iris (Fig. 4.13). Patients may present
complaining of a "second pupil." As the iris pulls away from
the ciliary body, a small amount of bleeding may result. Look closely for
associated traumatic hyphema.
|
|
|

|
|
Traumatic
Iridodialysis The iris has
pulled away from the ciliary body as a result of blunt trauma.
(Courtesy of Department of Ophthalmology, Naval Medical Center,
Portsmouth, VA.)
|
|
Differential Diagnosis
Traumatic hyphema, penetrating
injury to the globe, scleral rupture, intraocular foreign body, and lens
dislocation causing billowing of the iris should all be considered.
Emergency Department Treatment
and Disposition
A remote traumatic iridodialysis
requires no specific treatment in the ED. Recent history of ocular trauma
should prompt a diligent slit-lamp examination for associated hyphema or
lens discoloration. If hyphema is present, it should be treated as
discussed (see "Hyphema", above). Pure cases of iridodialysis
may be referred for specialty consultation to exclude other injuries; if
the defect is large enough to result in monocular diplopia, surgical
repair may be necessary.
Clinical Pearls
1. The examination should
carefully exclude posterior chamber pathology and hyphema.
2. A careful review of the
history to exclude penetrating trauma should be made. If the history is
unclear, CT scan may be used to exclude the presence of intraocular
foreign body.
3. A careful examination
includes searching for associated lens dislocation.
|
|
Lens Dislocation
Associated Clinical Features
Lens dislocation may result from
a sudden blow to the globe with resultant stretching of the zonule fibers
that hold the lens in place (Fig. 4.14). The patient may experience
symptoms of monocular diplopia or gross blurring of images, depending on
the severity of the injury. The edge of the subluxed lens may be visible
when the pupil is dilated (Fig. 4.15). If all the zonule fibers tear and
the lens is dislocated, it may lodge in the anterior chamber or the vitreous.
|
|
|
|
|
|
|
Lens
Dislocation Lens dislocation
revealed during slit-lamp examination. Note the zonule fibers, which
normally hold the lens in place. (Courtesy of Department of
Ophthalmology, Naval Medical Center, Portsmouth, VA.)
|
|
|
|
|

|
|
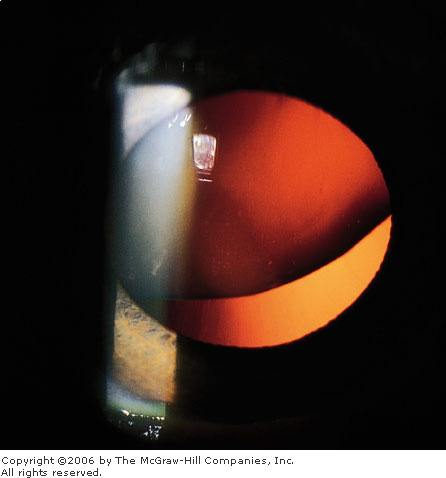
|
|
Lens
Dislocation The edge of this
dislocated lens is visible with the pupil dilated as an altered red
reflex. (Courtesy of Department of Ophthalmology, Naval Medical
Center, Portsmouth, VA.)
|
|
Differential Diagnosis
Marfan's syndrome, tertiary
syphilis, and homocystinuria may be present and should be considered in
patients presenting with lens dislocation.
Emergency Department Treatment
and Disposition
Almost all cases require surgery
if the lens is totally dislocated; partial subluxations may require only
a change in refraction.
Clinical Pearls
1. Patients may experience lens
dislocation with seemingly trivial trauma if they have an underlying
coloboma of the lens (see Fig. 4.20), Marfan's syndrome, homocystinuria,
or syphilis.
2. Iridodonesis is a trembling
movement of the iris noted after rapid eye movements and is a sign of
occult posterior lens dislocation.
|
|
Open Globe
Associated Clinical Features
Open globe injuries resulting
from penetrating trauma can be subtle and easily overlooked. All are
serious injuries. Signs to look for are loss of anterior chamber depth
caused by leakage of aqueous humor, a teardrop-shaped pupil, or prolapse
of choroid through the wound (Fig. 4.16).
|
|
|

|
|
Open
Globe This injury is not
subtle; extruded ocular contents (vitreous) can be seen; a teardrop
pupil is also present. (Courtesy of Alan B. Storrow, MD.)
|
|
Differential Diagnosis
Iridodialysis, corneal foreign
body, and scleral rupture may have similar presentations.
Emergency Department Treatment
and Disposition
All open globe injuries require
specialty consultation. A Fox (metal) eye shield should be placed over
the affected eye. No attempts to examine, measure pressures, or
manipulate the eye should be made. Intravenous antibiotics to cover
gram-positive organisms are appropriate. Sedation and aggressive pain
management are crucial and should be used liberally to prevent or
decrease expulsion of intraocular contents due to crying, activity, or
vomiting. Antiemetics should be given if nausea is present. Tetanus
immunization should be updated. Many open globe injuries are associated
with other significant blunt trauma injuries.
Clinical Pearls
1. When a large foreign body
such as a pencil or nail protrudes from the globe, resist the temptation
to remove it. Such objects should be left in place until definitively
treated in the operating room.
2. Control of pain, activity, and
nausea may be sight-saving and requires proactive use of appropriate
medications.
3. Use of lid hooks, retractors
(Fig. 4.17), or even retractors fashioned from paper clips (Fig. 4.18) is
preferred to open the eyelids of trauma victims with blepharospasm or
massive swelling. Attempts to do this with fingers can inadvertently
increase the pressure on the globe.
4. Penetrating globe injuries
are a relative contraindication to the sole use of depolarizing
neuromuscular blockade (e.g., succinylcholine). Pretreatment with a small
dose of a nondepolarizing agent should be given to abolish the
fasciculations and resultant increased intraocular pressure.
|
|
|

|
|
Eyelid
Retractors Retractors are used
to gain exposure without applying pressure to the globe. (Courtesy of
Dallas E. Peak, MD.)
|
|
|
|
|

|
|
Eyelid
Retractors Retractors
fashioned from paper clips can safely be used when standard
retractors are not available. (Courtesy of Kevin J. Knoop, MD, MS.)
|
|
|
|
Scleral Rupture
Associated Clinical Features
A forceful blow to the eye may
result in a scleral rupture. The diagnosis is obvious when orbital
contents are seen spilling from the globe itself. The diagnosis may be
more occult in situations where only a tiny rent in the sclera has
occurred. When rupture occurs at the limbus, a small amount of iris may
herniate, resulting in an irregularly shaped pupil called a teardrop
pupil (Fig. 4.19). A teardrop pupil may also be the result of a
penetrating foreign body. Mechanism is the key to distinguishing these
two causes. Another associated finding is bloody chemosis of the bulbar
conjunctiva over the area of scleral rupture. This may be distinguished
from a simple subconjunctival hematoma by bulging of the conjunctiva.
|
|
|

|
|
|
|
Corneal-Scleral
Rupture A teardrop pupil is
present, with a small amount of iris herniating from a rupture at the
limbus. These injuries may initially go unnoticed. (Courtesy of
Dallas E. Peak, MD.)
|
|
Differential Diagnosis
Subconjunctival hematoma,
nontraumatic bloody chemosis, corneal-scleral laceration, intraocular
foreign body, iridodialysis, and traumatic lens dislocation may have a
similar presentation. A coloboma of the iris (Fig. 4.20) may appear
similar to a teardrop pupil.
|
|
|

|
|
Iris
Coloboma Iris coloboma is a
congenital finding resulting from incomplete closure of the fetal
ocular cleft. It appears as a teardrop pupil and may be mistaken for
a sign of scleral rupture. (Courtesy of Department of Ophthalmology,
Naval Medical Center, Portsmouth, VA.)
|
|
Emergency Department Treatment
and Disposition
Urgent specialty consultation and
operative management are mandatory. The eye should be protected by a Fox
metal eye shield, and all further examination and manipulation of the eye
should be discouraged to prevent prolapse or worsening prolapse of
choriouveal structures. Tetanus status should be addressed. Intravenous
antibiotics to cover suspected organisms are appropriate. Adequate
sedation and use of parenteral analgesics is encouraged. Antiemetics
should be given proactively, since vomiting may result in further
prolapse of intraocular contents. CT scanning should be considered if the
presence of a foreign body is suspected.
Clinical Pearls
1. The eyeball may appear
deflated or the anterior chamber excessively deep. Intraocular pressure
will likely be decreased, but measurement should be avoided, since this
may worsen herniation of intraocular contents.
2. Rupture usually occurs where
the sclera is the thinnest, at the point of attachment of extraocular
muscles and at the limbus.
3. Bloody chemosis from scleral
rupture is distinguished from subconjunctival hematoma by bulging of the
conjunctiva. A subconjunctival hematoma is flat in appearance (see Fig.
4.22).
4. A teardrop pupil may easily
be overlooked in the triage process or in the setting of multiple
traumatic injuries.
5. Seidel's test (instillation
of fluorescein and observing for fluorescein streaming away from the
injury) may be used to diagnose subtle perforation (Fig. 4.21).
|
|
|

|
|
Seidel
Test A positive Seidel test
shows aqueous leaking through a corneal perforation while being
observed with the slit lamp. (Courtesy of John D. Mitchell, MD. Used
with permission from Tintinalli JE et al: Emergency Medicine: A
Comprehensive Study Guide, 5th ed. New York:
McGraw-Hill; 2000.)
|
|
|
|
Subconjunctival Hemorrhage
Associated Clinical Features
A subconjunctival hemorrhage or
hematoma occurs with often trivial events such as a cough, sneeze,
Valsalva maneuver, or minor blunt trauma. The patient may present with
some degree of duress secondary to the appearance of the bloody eye. The
blood is usually bright red and appears flat (Fig. 4.22). It is limited
to the bulbar conjunctiva and stops abruptly at the limbus. This
appearance is important to differentiate the lesion from bloody chemosis,
which can occur with scleral rupture. Aside from appearance, this
condition does not cause the patient any pain or diminution in visual
acuity.
|
|
|

|
|
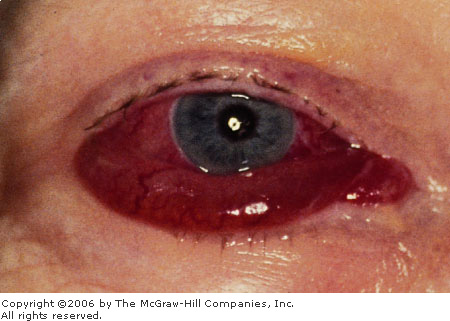
Subconjunctival
Hemorrhage Subconjunctival
hemorrhage in a patient with blunt trauma. The flat appearance of the
hemorrhage indicates its benign nature. (Courtesy of Dallas E. Peak,
MD.)
|
|
Differential Diagnosis
Scleral rupture, nontraumatic
bloody chemosis (Fig. 4.23), conjunctivitis, iritis, corneal-scleral
laceration, severe hypertension, and coagulopathy may have a similar
appearance or presentation.
|
|
|
|
|
Bloody
Chemosis "Bloody
chemosis" was confused with "subconjunctival
hemorrhage" in this patient with no history of trauma and positive
cranial nerve palsies. Cavernous sinus thrombosis was diagnosed.
(Courtesy of Eric Einfalt, MD.)
|
|
Emergency Department Treatment
and Disposition
No treatment is required. The
patient should be told to expect the blood to be resorbed in 2 to 3 weeks.
Clinical Pearls
1. Subconjunctival hematoma may
be differentiated from bloody chemosis by the flat appearance of the
conjunctival membranes.
2. A subconjunctival hematoma
involving the extreme lateral globe after blunt trauma is very suspicious
for zygomatic arch fracture.
3. Patients with nontraumatic
bloody chemosis should be evaluated for an underlying metabolic
(coagulopathy) or structural (cavernous sinus thrombosis) disorder.
|
|
Traumatic Cataract
Associated Clinical Features
Any trauma to the eye that
disrupts the normal architecture of the lens may result in the
development of a traumatic cataract—a lens opacity (Fig. 4.24). The
mechanism behind cataract formation involves fluid infiltration into the
normally avascular and acellular lens stroma. The lens may be observed to
swell with fluid and become cloudy and opacified. The time course is
usually weeks to months following the original insult. Cataracts that are
large enough may be observed by the naked eye. Those that are within the
central visual field may cause blurring of vision or distortion of light
around objects (e.g., halos).
|
|
|

|
|
Traumatic
Cataract This traumatic
cataract is seen as a large lens opacity overlying the visual axis. A
traumatic iridodialysis is also present. (Courtesy of Dallas E. Peak,
MD.)
|
|
Differential Diagnosis
Lens dislocation, intraocular
foreign body, hypopyon, corneal abrasion, and hyphema can present with
similar complaints. History and physical examination are helpful in
discriminating most of these conditions from traumatic cataract.
Emergency Department Treatment
and Disposition
No specific treatment is rendered
in the ED for cases of delayed traumatic cataract. Routine ophthalmologic
referral is indicated for most cases.
Clinical Pearls
1. Traumatic cataracts are
frequent sequelae of lightning injury. All lightning-strike victims
should be warned of this possibility.
2. Cataracts may also occur as
a result of electric current injury to the vicinity of the cranial vault.
3. Cataracts can be easily
examined using the +10-diopter setting on an ophthalmoscope or in more
detail with a slit lamp.
4. Leukocoria results from a dense
cataract, which causes loss of the red reflex.
5. If a cataract develops
sufficient size and "swells" the lens, the trabecular meshwork
may become blocked, producing glaucoma.
|
|
Chemical Exposure
Associated Clinical Features
Most symptomatic ocular exposures
involve either immediate or delayed onset of eye discomfort accompanied
by one or more of the following: itching, tearing, redness, photophobia,
blurred vision, and/or foreign-body sensation. Conjunctival injection or
chemosis may be noted on examination. Abrupt onset of more severe
symptoms may indicate exposure to caustic alkaline or acidic substances
and should be regarded as a true ocular emergency. Exposure to defensive
sprays or riot-control agents (e.g., Mace or tear gas) causes immediate onset
of severe ocular burning, intense tearing, blepharospasm, and irritation
of the mucous membranes of the nose and oropharynx. Chemical
conjunctivitis in the newborn may stem from the use of silver nitrate
drops at delivery for prophylaxis against Neisseria gonorrhoeae.
Many hospitals now favor erythromycin-based ointments.
Differential Diagnosis
Alkali or acid exposure, corneal
foreign body, corneal abrasion, infectious conjunctivitis, and
conjunctival foreign body should be considered.
Emergency Department Treatment
and Disposition
Treatment should begin in the
prehospital arena with immediate and copious irrigation. The patient who
presents acutely with possible caustic exposure should be triaged to
immediate treatment. An attempt should be made to determine the pH of the
conjunctival sac with a broad-range pH paper, though this determination
should not delay the initiation of treatment. Instillation of topical
anesthetic drops will permit a better examination. The conjunctiva should
be closely examined for concretions or foreign body, with eversion of the
upper lid. Any debris should be removed with a moistened cotton-tipped
applicator. If pH determination demonstrates acid or alkali exposure,
irrigation with warmed normal saline (NS) or lactated ringers (LS)
(preferred) solution should begin, using 1-L bags connected through
standard intravenous tubing to a Morgan lens. A minimum of 2-L should be
instilled, followed by a recheck of the pH or reassessment for continued
symptoms. If a normal tear film pH of 7.4 has not been achieved,
irrigation should be continued. Alkali exposures may cause severe injury
due to liquifaction necrosis, which penetrates the deeper tissues (Fig.
4.25). Acids produce a coagulative necrosis, which creates a barrier to
further penetration.
|
|
|

|
|
Alkali
Burn Diffuse opacification of
the cornea occurred from a "lye" burn to the face.
(Courtesy of Stephen Corbett, MD.)
|
|
Irrigation should be strongly
considered after chemical exposure to a non–acid or alkali source.
Many chemicals merely cause irritative symptoms; however, some may also
denude the corneal epithelium and inflame the anterior chamber. All
patients should undergo slit-lamp examination to document corneal
injuries (e.g., abrasions, punctate erosions, opacities) or anterior
chamber inflammation. Antibiotic drops may be indicated, particularly if
corneal injury is noted. Cycloplegics may be of benefit as well to reduce
ciliary spasm and pain in these cases.
Clinical Pearls
1. Immediate onset of severe
symptoms calls for immediate treatment and should prompt consideration of
alkali or acid exposure.
2. Determination of ocular pH
should be made in all cases of chemical exposure.
3. Prolonged (up to 24 h)
irrigation may be needed for alkaline exposures.
4. Concretions from the
exposure agent may form deep in the conjunctival fornices and must be
removed to prevent further injury (Fig. 4.26).
5. Corneal abrasions or
punctate erosions may be a direct result of the chemical agent or from
treatment with irrigation or placement of the Morgan lens.
|
|
|

|
|
Caustic
Burn Adhesions (Symblepharon)
Scarring of both palpebral and bulbar conjunctivae results in severe
adhesions between the lids and the globe. (Courtesy of Arden H.
Wander, MD.)
|
|
|
|