|
Note: Large images and
tables on this page may necessitate printing in landscape mode.
Copyright
©2006 The McGraw-Hill Companies. All rights reserved.
Emergency
Medicine Atlas > Part 1. Regional
Anatomy > Chapter 5. Ear, Nose, and Throat
Conditions >
|
Otitis Media
Associated Clinical Features
Children between the ages of 6
months and 2 years are at highest risk of developing acute otitis media
(AOM). Males, North American Eskimos, non-breast-fed infants, and
children with craniofacial anomalies have the highest incidence of AOM.
Additionally, children who contract their first episode prior to their
first birthday, have a sibling with a history of recurrent AOM, are in
day care, or have parents who smoke are at increased risk of recurrent
AOM.
In its most basic form, AOM is
defined as an acute inflammation and effusion of the middle ear. Otoscopy
of the middle ear should focus on color, position, translucency, and
mobility. Compared with the tympanic membrane of a normal ear (Fig. 5.1),
AOM causes the tympanic membrane to appear dull, erythematous or
injected, bulging, and less mobile (Figs. 5.2 and 5.3). Pneumatic
otoscopy and tympanometry enhance accuracy in diagnosing AOM. The light
reflex, normal tympanic membrane landmarks, and malleus become obscured.
|
|
|

|
|
|
|
Normal
Tympanic Membrane Normal
tympanic membrane anatomy and landmarks. (Courtesy of Richard A.
Chole, MD, PhD.)
|
|
|
|
|
|
|
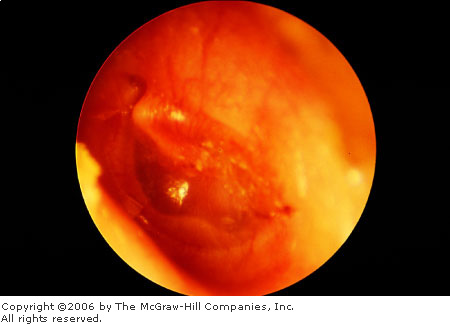
Early
Acute Otitis Media A mildly
erythematous tympanic membrane is seen with a small purulent effusion
in the middle ear. (Courtesy of C. Bruce MacDonald, MD.)
|
|
|
|
|

|
|
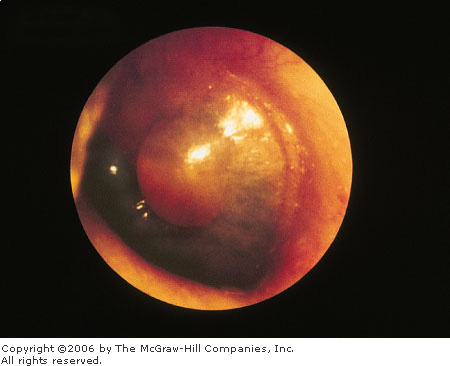
Acute
Otitis Media The middle ear is
filled with purulent material behind an erythematous, bulging
tympanic membrane. (Courtesy of Richard A. Chole, MD, PhD.)
|
|
There are many classifications and hence
presentations of AOM based on symptom duration and clinical presentation.
Regardless of classification, the common pathogenesis of AOM is
eustachian tube dysfunction, allowing retention of secretions (serous
otitis) (Figs. 5.4 and 5.5) and seeding of bacteria.
|
|
|

|
|
Serous
Otitis Media with Effusion (OME)
Copious purulent drainage in a newborn with neonatal gonococcal
conjunctivitis. (Reprinted with permission of the American Academy of
Ophthalmology, Eye Trauma and Emergencies: A Slide-Script Program.
San Francisco, 1985.)
|
|
|
|
|

|
|
Serous
OME A clear, amber-colored
effusion with multiple air-fluid levels is seen in the middle ear
behind a normal tympanic membrane. (Courtesy of C. Bruce MacDonald,
MD.)
|
|
AOM is caused by a wide variety
of viral, bacterial, and fungal pathogens. The most common bacterial
isolates are Streptococcus pneumoniae, Haemophilus influenzae,
Moraxella catarrhalis, and Streptococcus pyogenes.
Approximately 20% of middle ear effusion aspirations are sterile. The
prevalence of  -lactamase–producing
strains of H. influenzae and M. catarrhalis is variable but
increasing. -lactamase–producing
strains of H. influenzae and M. catarrhalis is variable but
increasing.
Patient presentations and
complaints vary with age. Infants with AOM have vague, nonspecific
symptoms such as irritability, lethargy, and decreased oral intake. Young
children can be irritable, often febrile, and frequently pull at their
ears, but they may also be completely asymptomatic. Older children and
adults note ear pain, decreased auditory acuity, and occasionally
otorrhea.
Differential Diagnosis
Myringitis, otitis externa,
perforations of the tympanic membrane, and herpes zoster can mimic otitis
media. Less common causes of ear pain include temporomandibular joint
disorders, odontogenic infections, and sinusitis. Erythema of the
tympanic membrane can appear in an otherwise healthy ear when a child
cries.
Emergency Department Treatment
and Disposition
Although AOM generally resolves
spontaneously, most patients are treated with antibiotics and analgesics.
Steroids, decongestants, and antihistamines do not alter the course in
AOM but may improve upper respiratory tract symptoms. Rarely, myringotomy
may be needed for pain relief.
Antibiotic selection is widely
variable. Amoxicillin, in the dose range of 80 to 90 mg/kg/day divided
tid, is a suitable first choice for an AOM. Alternatives for initial
therapy include trimethoprim-sulfamethoxazole,
erythromycin-sulfisoxazole, and second-generation cephalosporins. If the
patient remains symptomatic 48 to 72 h after beginning antibiotics,
amoxicillin with clavulanate, cefixime, or the newer macrolides may
provide broader coverage.
Patients should be instructed to
follow up in 10 to 14 days or return if symptoms persist or worsen after
48 h. Patients who have significant hearing loss, failed two complete
courses of outpatient antibiotics during a single event, have chronic
otitis media (OM) with or without acute exacerbations, or have failed
prophylactic antibiotics warrant referral to an otolaryngologist for
further evaluation, an audiogram, and possible tympanostomy tubes (Fig.
5.6).
|
|
|

|
|
Tympanostomy
Tube Typical appearance of a
tympanostomy tube in the tympanic membrane. These tubes will migrate
to the periphery and eventually drop out. Occasionally, they will be
found in the external ear canal. (Courtesy of C. Bruce MacDonald,
MD.)
|
|
Clinical Pearls
1. In children, recurrent OM is
often due to food allergies.
2. Only 4% of children under 2
years old with OM develop temperatures greater than 104°F. Children with
temperatures higher than 104°F or with signs of systemic toxicity should
be closely evaluated for other causes of the illness before attributing
the fever to OM.
|
|
Bullous Myringitis
Associated Clinical Features
Bullous myringitis is a direct
inflammation and infection of the tympanic membrane (TM) secondary to a
viral or bacterial agent. Vesicles filled with blood or serosanguinous
fluid or bullae on an erythematous tympanic membrane are the hallmark of
bullous myringitis (Fig. 5.7). Frequently a concomitant otitis media with
effusion is noted. Common bacterial agents are Mycoplasma pneumoniae,
Streptococcus pneumoniae, and Haemophilus influenzae.
|
|
|
|
|
Bullous
Myringitis A large
fluid-filled bulla is seen distorting the surface of the tympanic
membrane. (Courtesy of Richard A. Chole, MD, PhD.)
|
|
The onset of bullous myringitis
is preceded by an upper respiratory tract infection and is heralded by
sudden onset of severe ear pain, scant serosanguinous drainage from the
ear canal, and frequently some degree of hearing loss. Otoscopy reveals
bullae on either the inner or outer surface of the TM, often filled with
red bloody fluid. Patients presenting with fever, hearing loss, and
purulent drainage are more likely to have other concomitant infections,
such as otitis media and otitis externa.
Differential Diagnosis
Barotrauma is usually associated
with swimming, diving, or airplane travel. Herpes zoster oticus produces
facial nerve palsy and facial pain. Otitis externa causes edema of the
external auditory canal and drainage, whereas otitis media may distort
the TM but rarely causes bullae.
Emergency Department Treatment
and Disposition
Differentiation between viral and
bacterial etiologies for tympanic membrane bullae is difficult but,
fortunately, seldom necessary. Although most episodes resolve spontaneously,
many physicians prescribe antibiotics, such as
trimethoprim-sulfamethoxazole or a macrolide. Warm compresses, topical or
strong systemic analgesics, and oral decongestants may provide
symptomatic relief. Referral is not necessary in most cases unless
rupture of the bullae is required for pain relief.
Clinical Pearl
1. Facial nerve paralysis
associated with clear, fluid-filled TM vesicles is characteristic of
herpes zoster oticus.
|
|
Cholesteatoma and Osteoma
Associated Clinical Features
Contrary to the origin suggested
by their name, cholesteatomas are not neoplasms but rather epidermoid
inclusion cysts: collections of desquamating stratified squamous
epithelium found in the middle ear or mastoid air cells. Congenital
cholesteatomas are most frequently found in children and young adults.
Acquired cholesteatomas originate from perforations of the tympanic
membrane, usually marginally or in the pars flaccida, allowing migration
of stratified squamous epithelium from the external auditory canal into the
middle ear.
Cholesteatomas can be locally
destructive of the middle ear ossicles and tympanic membrane and, through
the production of collagenases, erode into the temporal bone, inner ear
structures, mastoid sinus, or posterior fossa dura. Delays in treatment
can lead to permanent conductive hearing loss or infectious
complications.
Patients present with progressive
hearing loss, foul-smelling ear drainage, and, in advanced stages, pain,
headache, dizziness, facial paralysis, fever, or vertigo. Many cholesteatomas
have an insidious progression without associated pain or symptoms.
Cholesteatomas are seen on otoscopy as either a retraction pocket
containing white debris or a yellow crust on the tympanic membrane with
or without a perforation (Figs. 5.8 and 5.9). A middle ear cholesteatoma
appears as a pearly white or yellow middle ear mass behind the tympanic
membrane, producing a focal bulge, in contrast to the more diffuse
displacement of the tympanic membrane seen in otitis media. Radiographs
and computed tomography (CT) scans may reveal bony destruction.
|
|
|

|
|
Congenital
Cholesteatoma A congenital
cholesteatoma is seen behind an intact tympanic membrane. (Courtesy
of C. Bruce McDonald, MD.)
|
|
|
|
|

|
|
|
|
Cholesteatoma A cholesteatoma is seen in this ear. Primary
acquired cholesteatomas are thought to arise from gradual
invagination of the pars flaccida, usually secondary to trauma. Note
the yellow epithelial debris from the cholesteatoma in the area of
the pars flaccida. Often there is an effusion and debris, which can
distort the anatomy on otoscopy. (Courtesy of C. Bruce MacDonald,
MD.)
|
|
Osteomas (sometimes called exostoses) are benign
bone overgrowths of the external auditory canal (EAC) found deep in the
meatus. Osteomas are often seen in patients with recurrent cold water
exposures, such as swimmers and divers. Osteomas are seen on otoscopy as
single or multiple round shiny swellings of the bony external auditory
canal (Fig. 5.10). A secondary cerumen impaction or an otitis externa may
obscure the examination.
|
|
|

|
|
Osteomas Multiple osteomas almost occlude the external
auditory canal. The tympanic membrane can be seen in the center, past
the osteomas. These lesions are often seen in patients who are cold
water swimmers. (Courtesy of C. Bruce MacDonald, MD.)
|
|
Differential Diagnosis
Wax particles and EAC foreign
bodies may resemble cholesteatomas on otoscopy. Furuncles are painful to
palpation, whereas otitis externa and otitis media cause EAC drainage and
middle ear effusions, respectively.
Emergency Department Treatment
and Disposition
Early diagnosis of cholesteatomas
is essential for proper referral. Water avoidance as well as topical and
sometimes systemic antibiotics are important. Small cholesteatomas found
in retraction pockets can be excised and a tympanostomy tube placed to
equilibrate middle ear pressures. More extensive cholesteatomas may
require surgical excision, tympanoplasty, and radical mastoidectomy.
Osteomas require no medical or surgical management unless they become
symptomatic.
Clinical Pearls
1. Persistent pain associated
with headache, facial motor weakness, nystagmus, or vertigo suggests
inner ear or intracranial involvement.
2. Polyps found on the tympanic
membrane can indicate the presence of a cholesteatoma and require further
evaluation to exclude its presence.
|
|
Tympanic Membrane Perforation
Associated Clinical Features
Acute tympanic membrane (TM)
perforations are often the result of direct penetrating trauma, water or
air pressure changes (barotrauma, blast injuries), chronic otitis media,
corrosives, thermal injuries (electricity, lightning, heated objects),
and iatrogenic causes (foreign-body removal, tympanostomy tubes). TM
perforations are occasionally complicated by damage to the ossicular
chain that produces a more complete conductive hearing loss, temporal
bone injuries, and cranial nerve damage.
Patients complain of a sudden
onset of ear pain, vertigo, tinnitus, and altered hearing after a
specific event. Patients with posterior perforations present with a more
profound deafness than those with anterior perforations. Physical
examination of the TM reveals a slit-shaped tear or larger perforation
with an irregular border. An acute perforation can have blood on the
perforation margin and blood or clot in the canal (Fig. 5.11). The
margins are smooth in subacute or chronic perforations.
|
|
|

|
|
Acute
Tympanic Membrane Perforation
An acute tympanic membrane perforation is seen. Note the sharp edges
of the ruptured tympanic membrane. (Courtesy of Richard A. Chole, MD,
PhD.)
|
|
Differential Diagnosis
Congenital malformations, chronic
perforations, residual perforations from tympanostomy tubes, and
retraction pockets have more regular borders and no bleeding or TM
erythema.
Emergency Department Treatment
and Disposition
Treatment of acute tympanic
membrane perforations is tailored to the mechanism. All easily removable
foreign bodies should be extracted. Corrosive exposures require face,
eye, and ear decontamination. Antibiotics and irrigation do not improve
the rate or completeness of healing unless the injury is associated with
OM. Systemic antibiotics should be used for perforations associated with
OM, penetrating injury, and possibly water-sport injuries (see
"Otitis Media," above). Topical steroids impede perforation
closure.
Patients are instructed to avoid
allowing water to get into the ear while the perforation is healing and
to return if symptoms of infection appear. All TM perforations should be
referred to an otolaryngologist for follow-up for possible myringoplasty.
Even though nearly 80% of all TM perforations heal spontaneously, some do
not, and complications can develop.
Clinical Pearls
1. Cortisporin eardrops of any
formulation have been shown to retard spontaneous healing and should be
avoided.
2. Traumatic TM perforation
associated with cranial nerve deficits or persistent vertigo requires
immediate ear/nose/throat (ENT) consultation for possible temporal bone
fractures or injury to the round or oval window.
|
|
Otitis Externa
Associated Clinical Features
Otitis externa (OE), or
"swimmer's ear," is an inflammation and infection (bacterial or
fungal) of the auricle and external auditory canal (EAC). Typical
symptoms include otalgia, pruritus, otorrhea, and hearing loss. Physical
examination reveals EAC hyperemia and edema (Fig. 5.12), otorrhea,
malodorous discharge, occlusion from debris and swelling, pain with
manipulation of the tragus, and periauricular lymphadenopathy.
|
|
|

|
|
Otitis
Externa A discharge is seen
coming from the external auditory canal, which is swollen and almost
completely occluded. An ear wick placed in the EAC facilitates
delivery of topical antibiotic suspension and drainage of debris.
(Courtesy of Frank Birinyi, MD.)
|
|
Several factors predispose the EAC to infection:
increased humidity and heat, water immersion, foreign bodies, trauma,
hearing aids, and cerumen impaction. Bacterial OE is primarily an
infection due to Pseudomonas species or Staphylococcus aureus.
Diabetics are particularly prone to infections by Pseudomonas, Candida
albicans, and, less commonly, Aspergillus niger (Fig. 5.13).
|
|
|

|
|
Aspergillus
Otitis Externa Chronic otitis
externa with copious debris, including black spores from Aspergillus
niger, cottony fungal elements, and wet debris. This patient had
been treated with topical and systemic antibiotics. (Courtesy of C.
Bruce MacDonald, MD.)
|
|
Differential Diagnosis
Cholesteatomas and foreign bodies
can produce a secondary OE. Periauricular cellulitis, herpes zoster
oticus (Fig. 5.14), and malignant otitis externa have auricular and
facial involvement. EAC dermatitis, eczema, and furuncles rarely produce
EAC drainage.
|
|
|

|
|
Herpes
Zoster Oticus Erythema and
drainage coming from the EAC is seen in this patient with herpes
zoster oticus. Otitis externa can have a similar appearance but does
not have vesicles, as seen in this patient. (Courtesy of Robin T.
Cotton, MD.)
|
|
Emergency Department Treatment
and Disposition
Saline irrigation and suctioning
is recommended to thoroughly evaluate the EAC. Topical antibiotic suspensions
(containing polymyxin, neomycin, and hydrocortisone or ciprofloxacin)
with ear wicks are effective. Topical solutions are not
pH-balanced and thus are irritating and may cause inflammation in the
middle ear if a perforation is present. Systemic antibiotics are not
indicated unless extension into the periauricular tissues is noted.
Patients should avoid swimming and prevent water from entering the ear
while bathing. Dry heat aids in resolution, and analgesics provide
symptomatic relief. Follow-up should be arranged in 10 days for routine
cases.
Clinical Pearls
1. Resistant cases may have an
allergic or edematous component. These typically present with a dry,
scaly, itchy EAC and are recurrent and chronic in nature.
2. Drying the EAC after water
exposure with a 50:50 mixture of isopropyl alcohol and water or with
acetic acid (white vinegar) minimizes recurrence. If the TM is possibly
perforated, isopropyl alcohol should be avoided.
3. Often the symptoms are out
of proportion to the visible findings, necessitating narcotic analgesia.
|
|
Mastoiditis
Associated Clinical Features
Mastoiditis or acute coalescent
mastoiditis is an infection or inflammation of the mastoid air cells that
usually results from extension of purulent otitis media with progressive
destruction and coalescence of air cells. Medial wall erosion can cause
cavernous sinus thrombosis, facial nerve palsy, meningitis, brain
abscess, and sepsis. With the use of antibiotics for acute otitis media,
the incidence of mastoiditis has fallen sharply.
Patients present with fever,
chills, postauricular ear pain, and frequently discharge from the
external auditory canal. Patients may have tenderness, erythema,
swelling, and fluctuance over the mastoid process; lateral displacement
of the pinna (Fig. 5.15); erythema of the posterior-superior external
auditory canal wall; and purulent otorrhea through a tympanic membrane
perforation.
|
|
|

|
|
Acute
Mastoiditis Postauricular
swelling and redness in a young girl with acute mastoiditis.
(Courtesy of Robin T. Cotton, MD.)
|
|
Differential Diagnosis
Postauricular abscesses,
furuncles, suppurative adenitis, lymphadenitis, and, rarely, carcinomas
of the mastoid can present with signs and symptoms of acute mastoiditis.
Emergency Department Treatment
and Disposition
Initial evaluation includes a
thorough head, neck, and cranial nerve examination while mastoid
radiographs may demonstrate coalescence of the mastoid air cells.
Computed tomography, the diagnostic procedure of choice, may reveal bony
extension and intracranial involvement.
Penicillinase-resistant
penicillins, amoxicillin-clavulanic acid, second-generation
cephalosporins, and the newer macrolides are effective in mild cases of
mastoiditis. Severe cases require parenteral semisynthetic penicillins,
cephalosporins, or vancomycin. Mastoiditis requires close follow-up and
prompt consultation.
Clinical Pearls
1. Most patients require
admission for parenteral antibiotics to cover Haemophilus influenzae,
Moraxella catarrhalis, streptococcal species, and Staphylococcus
aureus.
2. Surgical irrigation and
debridement and possibly mastoidectomy are reserved for refractory cases.
3. Delays in treatment can
result in significant morbidity and mortality.
4. Chronic mastoiditis
describes chronic otorrhea of at least 2 months duration. It is often
associated with craniofacial anomalies.
|
|
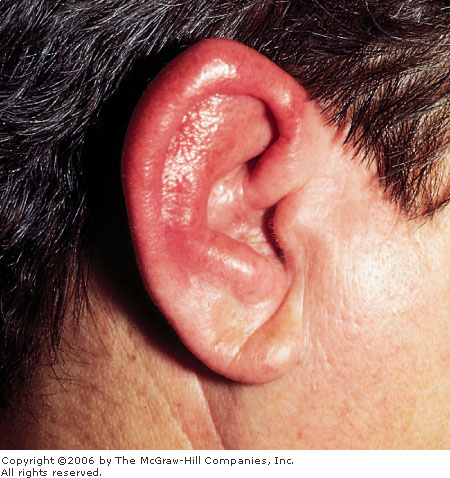
Perichondritis
Associated Clinical Features
Perichondritis is an infection of
the auricular cartilage. It can result from direct trauma; traumatic
hematomas; thermal injuries, typically frostbite; foreign bodies in the
external auditory canal; chronic otitis media; otitis externa; skin
infections; chronic mastoiditis; acupuncture and surgical procedures on
the ear. Destruction and necrosis of the auricular cartilage can lead to
a flaccid, flat ear.
The microbiology of
perichondritis reflects the source of infection. Infections of skin
structures and trauma involve streptococci and staphylococci. Ear and
mastoid sources frequently involve gram-negative organisms. Untreated
perichondritis in elderly diabetic and immunocompromised patients can lead
to malignant external otitis.
Patients present with severe pain
and diffuse swelling of the ear. Physical examination reveals an
erythematous, swollen, warm and tender pinna (Fig. 5.16). Advanced cases
can progress to necrosis of the ear cartilage (chondritis) and spreading
cellulitis.
|
|
|
|
|
Perichondritis The pinna is swollen and erythematous. No
concomitant otitis externa, mastoiditis, or furuncle is noted.
(Courtesy of Lawrence B. Stack, MD.)
|
|
Differential Diagnosis
Periauricular cellulitis can
mimic perichondritis but has facial involvement. Auricular hematomas
follow direct trauma. Contact dermatitis can develop from topical ear
medications and jewelry. The first episode of relapsing polychondritis
may be difficult to distinguish from perichondritis. The absence of fever
and history of previous cartilage involvement suggests relapsing
polychondritis.
Emergency Department Treatment
and Disposition
Immediate treatment of
perichondritis is essential to preserve the external ear cartilage. Early
perichondritis is treated by irrigation and debridement of any abscess,
with administration of broad-spectrum antibiotics such as
penicillinase-resistant penicillins, amoxicillin-clavulanate, or
ciprofloxacin. Topical antibiotics are ineffective. A compressive mastoid
and auricular dressing is beneficial. Strict follow-up is essential to
prevent treatment failure and progression of infection. Advanced
perichondritis requires high-dose parenteral antibiotics and early
specialist referral for surgical irrigation and debridement.
Clinical Pearl
1. Early diagnosis and
treatment are necessary to avoid permanent deformity of the pinna.
|
|
Septal Hematoma
Associated Clinical Features
Septal hematomas are an uncommon
complication of direct trauma to the nose. While often associated with
fracture of the nasal septum with or without concomitant nasal bone
fracture, the trauma is typically minor. Septal hematomas may also result
from septal surgery or rhinoplasty. Regardless of the mechanism, bleeding
from submucosal blood vessels leads to an accumulation of blood between
the mucoperichondrium and the septal cartilage. Pressure exerted by the
hematoma on the septal cartilage and its blood supply may lead to
ischemic avascular necrosis of the underlying cartilage, causing
destruction of the cartilage and deformity of the distal nose (saddle
deformity). The hematoma and any necrotic cartilage may then serve as a
nidus for infection, resulting in a septal abscess.
In addition to the cosmetic nasal
deformity, septal hematomas and deformity may lead to chronic sinus
infections, recurrent epistaxis, and sleep disturbances. Rarely, septal
abscesses can result in more serious complications such as cavernous
sinus thrombosis and meningitis. Since the original trauma is often
minor, patients may present days to weeks after the injury. Young
children and infants may present with poor feeding, fever, and rhinorrhea,
while older children and adults may note bleeding, headache, and more
focal pain. Patients with obvious nasal fractures tend to present
earlier.
On nasal examination, the
hematoma appears as a large, red, round swelling originating off the
septum and occluding most of the nasal cavity (Fig. 5.17). The mass is
very painful to palpation and may cause the outer aspects of the nose to
be tender as well. Septal abscesses tend to be more painful and larger
than uncomplicated hematomas. Constitutional symptoms such as fever are
frequently present. The microbiology of septal abscesses reflects the
normal flora of the nasal cavity. Staphylococcus aureus, group A  -hemolytic
streptococcus, Haemophilus influenzae, and Streptococcus
pneumoniae are the organisms most commonly isolated. -hemolytic
streptococcus, Haemophilus influenzae, and Streptococcus
pneumoniae are the organisms most commonly isolated.
|
|
|

|
|
Septal
Hematoma A septal hematoma is
seen in both nares in this child. (Courtesy of Robin T. Cotton, MD.)
|
|
Differential Diagnosis
Septal abscesses, foreign bodies,
and nasal polyps may also appear as masses in the nasal cavity.
Emergency Department Treatment
and Disposition
An index of suspicion and prompt
recognition are essential in diagnosing septal hematomas. Once
identified, prompt referral to an otolaryngologist is mandatory for
incision of the hematoma and drainage through the mucosal surface.
Purulent drainage should be sent for microbiology and culture.
Many authors recommend packing of
the nasal cavity to prevent further accumulation. Other surgeons use
temporary drains, such as a Penrose, while still others place dissolvable
sutures in the mucoperichondrium to prevent hematoma reaccumulation.
Clinical Pearls
1. Intranasal examination in
all patients with a history of nasal trauma regardless of severity is
crucial.
2. Antibiotics are required in
septal hematomas with a clinical suspicion for a secondary infection or
abscess.
3. The physician must explore
the possibility of child abuse in young children and infants with septal
hematomas and abscesses.
|
|
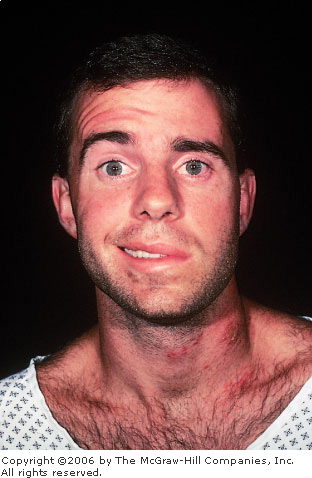
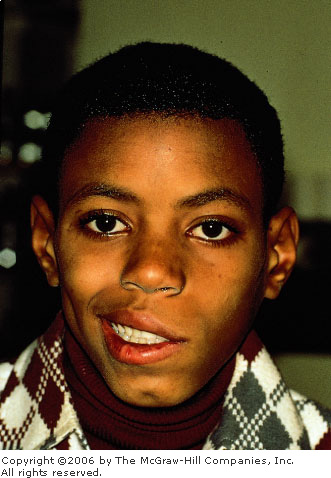
Herpes Zoster Oticus (Ramsay Hunt Syndrome)
Associated Clinical Features
Herpes zoster oticus (HZO), or
Ramsay Hunt syndrome, is the second most common cause of facial
paralysis, representing 3 to 12% of such patients. The syndrome consists
of facial and neck pain, acoustic symptoms, and facial palsy associated
with the reactivation of varicella zoster in the facial nerve and
geniculate ganglion (Figs. 5.18 and 5.19; see also Fig. 5.14). Patients
first note a pruritus, followed by pain out of proportion to the physical
examination over the face and ear. Patients may note vertigo, hearing
loss (sensorineural) from involvement of the eighth cranial nerve,
tinnitus, rapid onset of facial paralysis, decrease in salivation, loss
of taste sensation over the posterolateral tongue, and vesicles on the
ear, external auditory canal, and face.
|
|
|
|
|
Herpes
Zoster Oticus Facial palsy in
a young adult. Note the vesicular eruptions on the neck. (Courtesy of
Frank Birinyi, MD.)
|
|
|
|
|

|
|
Herpes
Zoster Oticus On closer
examination, the vesicles extend up the neck to the external auditory
canal. (Courtesy of Frank Birinyi, MD.)
|
|
Differential Diagnosis
Cerebrovascular accidents develop
acutely and do not produce pain in the face or external auditory canal.
Facial paralysis from temporal bone fractures is associated with
antecedent trauma. Ménière's disease can be confused with early HZO but
is painless and does not cause facial paralysis.
Emergency Department Treatment
and Disposition
The diagnosis of HZO is based
largely on history and physical examination. Tzanck preparations may be
difficult because of the vesicles' location. Magnetic resonance imaging
(MRI) with contrast may show enhancement of the geniculate ganglion and
facial nerve, but it is not required to make the diagnosis.
Oral acyclovir, 800 mg five times
a day for 7 to 10 days, or famciclovir, 500 mg tid for 7 days in
combination with oral steroids (such as prednisone 60 to 80 mg/day) are
the mainstays for HZO treatment. It is important to protect the involved
eye from corneal abrasions and ulcerations by using lubricating drops.
Clinical Pearl
1. The prognosis for facial
paralysis due to HZO is worse than that for Bell's palsy. Approximately
10 and 66% of patients with full and partial facial paralysis,
respectively, recover fully. The prognosis improves if the symptoms of
HZO are preceded by the vesicular eruption.
|
|
Facial Nerve Palsy
Associated Clinical Features
The seventh cranial or facial
nerve provides innervation of the facial muscles via the five branches of
the motor root; it innervates the submandibular, sublingual, and lacrimal
glands as well as the taste organs on the anterior two-thirds of the
tongue and provides sensation to the pinna of the ear. A seventh-nerve
palsy may occur as an isolated finding or as part of a constellation of
symptoms. Facial palsies are classified as being either central or
peripheral. Central seventh-nerve lesions occur before or proximal to the
seventh-nerve nucleus in the pons. Lesions that occur distal to the
nucleus are classified as peripheral lesions. The hallmark of central lesions
is the sparing of the ipsilateral frontalis muscle (Fig. 5.20), since it
receives innervation in the nucleus from both ipsilateral and
contralateral motor cortices. Peripheral injuries involve the entire side
of the face, including the forehead (Fig. 5.21).
|
|
|

|
|
Central
Seventh-Nerve Palsy Central
facial nerve paralysis with forehead sparing. (Courtesy of Frank
Birinyi, MD.)
|
|
|
|
|
|
|
Peripheral
Seventh-Nerve Palsy A
peripheral nerve paralysis involving the entire ipsilateral face,
including the forehead, is seen in this patient with Bell's palsy.
(Courtesy of Robin T. Cotton, MD.)
|
|
The most common etiology of
seventh-nerve dysfunction is Bell's palsy, an idiopathic facial nerve
dysfunction. Bell's palsy is most likely a viral or postviral syndrome,
with 60% of patients having a viral prodrome. Bell's palsy shows no age,
sex, or racial predilection. The incidence is higher in pregnant women,
diabetics, and those with a family history of Bell's palsy. It is
bilateral in less than 1% of patients.
Patients with Bell's palsy have
an acute onset of facial weakness and may note numbness or pain on the
ipsilateral face, ear, tongue, and neck as well as a decrease or loss of
ipsilateral tearing and saliva flow. Hearing in Bell's palsy is
preserved.
The prognosis for facial nerve
palsies is variable. Facial weakness—as compared with complete
paralysis—has a better prognosis for full recovery. Facial palsies
due to herpes zoster have a protracted course, and many do not fully
resolve. In comparison, 80% of patients with Bell's palsy due to other
causes completely recover within 3 months. The recurrence rate of Bell's
palsy is 7 to 10%.
Differential Diagnosis
Acoustic neuromas and central
nervous system masses have gradual progression of symptoms and cause
other neurologic findings. Neurologic disorders—such as
Guillain-Barré syndrome, multiple sclerosis, neurosarcoid, and
cerebrovascular accidents—also cause additional neurologic
sequelae. Temporal bone fractures are associated with trauma. The
differential diagnosis also includes infections (otitis media, otitis
externa, HIV) and parotid tumors.
Emergency Department Treatment
and Disposition
Initial evaluation is directed by
the history. The examination should include a thorough examination of the
ear (including sensorineural or conductive hearing loss), the eye
(including lacrimation), and the cranial nerves. Motor function of the
seventh cranial nerve is evaluated by having the patient raise his or her
eyebrows, smile, pucker, and frown. No single laboratory test is
diagnostic. Screening CT or MRI of the head is of little value in the
absence of additional findings on physical examination.
Most authors empirically
recommend steroids and antiherpetic antivirals for Bell's palsy. A
typical regimen is prednisone, 60 mg a day for 10 days, then tapered, in
combination with acylovir, famcylovir, or valacyclovir. If treated within
the first 3 weeks, steroids may decrease the sequelae of Bell's palsy. In
all facial nerve palsies, eye lubricants and taping or patching of the
eye at night help prevent keratitis and ulceration. Referral to a
specialist should be made for follow-up care.
Clinical Pearls
1. Facial nerve paralysis is a
symptom, not a diagnosis. The etiology of the paralysis must be known
before a diagnosis can be made.
2. If a provisional diagnosis
of Bell's palsy is made and no resolution of symptoms occurs, the
diagnosis must be reconsidered. In patients misdiagnosed with Bell's
palsy, tumors are the most common missed etiology.
3. Lacrimation is tested by the
Schirmer's or litmus test. Asymmetry may indicate a lesion proximal to
the geniculate ganglion.
|
|
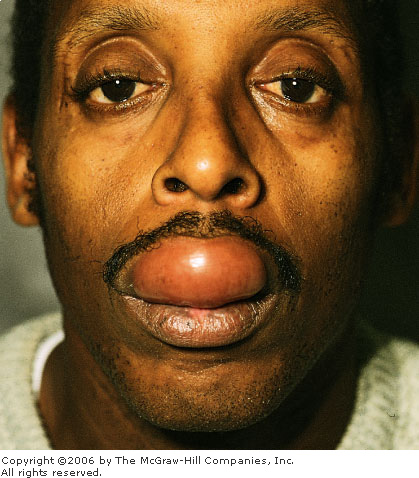
Angioedema
Associated Clinical Features
Angioedema is clinically
characterized by acute onset of well-demarcated cutaneous swelling of the
face, lips, and tongue; edema of the mucous membranes of the mouth,
throat, or abdominal viscera; or nonpitting edema of the hands and feet.
Angioedema is classified as either hereditary, allergic, or idiopathic.
Hereditary angioedema is an autosomal dominant trait associated with a
deficiency of serum inhibitor of the activated first component of
complement (C1). Allergic angioedema can result from medications
[nonsteroidal anti-inflammatory drugs (NSAIDs), contrast agents],
environmental antigens (Hymenoptera), or local trauma. Whatever the
cause, angioedema can be a life-threatening illness. Complications of
angioedema range from dysphagia and dysphonia to respiratory distress,
airway obstruction (Fig. 5.22), and death. Of special interest is angiotensin
converting enzyme (ACE) inhibitor–induced angioedema. Angioedema
due to ACE inhibitors has a predilection for involvement of the lips
(Fig. 5.23), face, tongue, and glottis. Standard treatment practices for
allergic urticaria often fail to improve ACE inhibitor–induced
angioedema; in those who do improve, rebound is frequently seen.
|
|
|

|
|
Angioedema Severe angioedema of the face and tongue
requiring emergent cricothyrotomy. (Courtesy of W. Brian Gibler, MD.)
|
|
|
|
|
|
|
ACE
Inhibitor–Induced Angioedema
Angioedema of the upper lip in a man who had been taking an ACE
inhibitor for 2 years. The patient had no previous episodes.
(Courtesy of Kevin J. Knoop, MD, MS.)
|
|
Differential Diagnosis
Anaphylaxis and asthma occur in
patients with histories of similar events and involve the lower airways.
Patients with epiglottitis, Ludwig's angina, and peritonsillar or
retropharyngeal abscesses often have a preceding pharyngeal or
odontogenic infection and present with systemic symptoms of infection,
such as fever and chills.
Emergency Department Treatment
and Disposition
Initial treatment of angioedema
is airway management. Most patients do not require intervention, but
frequent reassessment of the patient's airway is mandatory. Airway interventions
include nasopharyngeal intubation, endotracheal intubation (often
difficult due to lingual and oral obstruction), or nasotracheal
intubation (either blindly or with fiberoptics), or a cricothyrotomy.
Acute angioedema is treated
similarly to an allergic reaction. Depending on the severity of symptoms,
it can be treated with steroids, antihistamines—both H1
and H2 blockers—and subcutaneous epinephrine. Chronic
angioedema responds better to corticosteroids and H2 blockers,
but airway protection remains the primary focus of emergency treatment.
Hereditary angioedema is more refractory to medical interventions;
epinephrine, corticosteroids, and antihistamines provide little relief.
Disposition depends on the
severity and resolution of symptoms. Patients whose symptoms
significantly improve or show no progression after 4 h of observation may
be discharged home on a short course of oral steroids and antihistamines.
Any medication which may have caused the angioedema should be
discontinued. Angioedema with airway involvement requires admission to a
monitored environment, with surgical airway instruments always at the
bedside.
Clinical Pearls
1. Do not underestimate the
degree of airway involvement; act early to preserve airway patency.
2. Angioedema can also cause
gastrointestinal and neurologic involvement.
3. Early response to medical
intervention does not preclude rebound of symptoms to a greater extent
than at presentation.
4. Patients who have been using
ACE inhibitors for months or years can still develop angioedema.
|
|
Pharyngitis
Associated Clinical Features
Pharyngitis is an inflammation
and frequently an infection of the pharynx and its lymphoid tissues,
which make up Waldeyer's ring. Most causes of pharyngitis are infectious
and self-limited, with viral infections accounting for 90% of all cases.
Common bacterial agents include group A beta-hemolytic streptococci
(GABHS, responsible for up to 50% of bacterial cases), other
streptococci, Mycoplasma pneumoniae, Neisseria gonorrhea, and Corynebacterium
diphtheriae. In immunocompromised patients and patients on
antibiotics, Candida species can cause thrush. Sore throats that
last longer than 2 weeks should increase suspicion for either a
deep-space neck infection or a neoplastic cause.
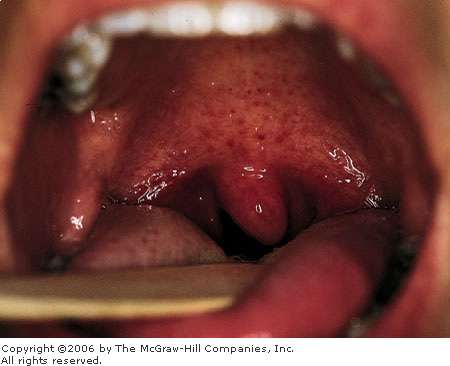
Patients with bacterial and
especially GABHS pharyngitis present with an acute onset of sore throat
and fever and frequently nausea, vomiting, headache, and abdominal
cramping. On examination, they may have a mild to moderate fever, an
erythematous posterior pharynx and palatine tonsils, tender cervical
lymphadenopathy, and palatal petechiae (Fig. 5.24). Classically, the
tonsils have a white or yellow exudate with debris in the crypts;
however, many patients may not have exudate on examination. Viral
pharyngitis is typically more benign, with a gradual onset, lower
temperature, and less impressive erythema and swelling of the pharynx.
Except for infectious mononucleosis, which can take weeks to resolve,
most cases of viral pharyngitis are self-limited, with spontaneous resolution
in a matter of days. Lingual and adenoid tonsillitis may also be present
(Fig. 5.25).
|
|
|
|
|
Palatal
Petechiae Palatal petechiae
and erythema of the tonsillar pillars in a patient with streptococcal
pharyngitis. (Courtesy of Kevin J. Knoop, MD, MS.)
|
|
|
|
|

|
|
Lingual
Tonsillitis This radiograph
shows lingual and adenoid tonsillitis. (Courtesy of Edward C. Jauch,
MD, MS.)
|
|
Differential Diagnosis
Deep-space neck infections,
diphtheria, epiglottitis, infectious mononucleosis, and Ludwig's angina
are other infectious causes of sore throats that should be considered.
Allergic rhinitis, angioedema, and pharyngeal neoplasms are noninfectious
causes of similar pharyngeal symptoms. Foreign bodies and local
pharyngeal trauma produce similar symptoms but usually have an antecedent
event.
Emergency Department Treatment
and Disposition
Treatment is largely symptomatic
except for antibiotics and rehydration. Patients with known or suspected
GABHS require antibiotics primarily to prevent the severe sequelae of the
infection, including rheumatic fever and glomerulonephritis, and
suppurative complications. Current first-line antibiotic therapies remain
a single dose of intramuscular benzathine penicillin or oral penicillin
for 10 days. Patients allergic to penicillin should receive erythromycin
for primary prophylaxis against rheumatic fever. Other suitable
antibiotics include azithromycin or clarithromycin and second-generation
cephalosporins. Analgesics, antipyretics, and throat sprays or gargles can
provide symptomatic relief.
Clinical Pearls
1. The physical examination
should not end at the neck. Auscultation of the chest, palpation of the
abdomen, and examination of the skin are also important.
2. Sore throats or chronic
pharyngitis that lasts more than 2 weeks must be referred for further
evaluation to rule out possible neoplastic or neurologic causes,
especially in patients over 50 years old who have a smoking or chewing
tobacco history.
3. Recurrent tonsillitis in
children merits referral for possible adenoid-tonsillectomy.
4. Amoxicillin should be
avoided if infectious mononucleosis is a possibility, as a diffuse
maculopapular rash will occur in up to 80%.
5. Pharyngitis itself may be a
prodrome for other pathologic conditions, such as measles, scarlet fever,
and influenza.
|
|
Diphtheria
Associated Clinical Features
Diphtheria is a highly contagious
disease caused by the exotoxin-producing bacterium Corynebacterium
diphtheriae. It is transmitted either by direct contact or through
respiratory aerosolization in coughing or sneezing. Many adults are now
susceptible to diphtheria because their vaccine-induced immunity
decreases over time or owing to decreased opportunity for naturally
acquired immunity. Because of this, recent outbreaks have involved
adolescents and adults rather than children.
Prior to the widespread
implementation of childhood vaccines in the 1940s, diphtheria was
associated with significant childhood mortality. While the United States
has only episodic cases of diphtheria, the incidence worldwide is
increasing dramatically because of decreased immunization rates in
developing countries. In the new republics of the former Soviet Union,
over 160,000 new cases and 5000 deaths were reported in the recent
epidemic.
Diphtheria most commonly affects
the mucosa of the upper respiratory tract and less commonly the mucosa of
the nasopharynx, nares, or tracheobronchial tract. Diphtheria typically
produces an ulcerated pharyngeal mucosa with a white to gray inflammatory
pseudomembrane (Fig. 5.26), classically with a "wet mouse"
odor. Patients present with symptoms, in order of frequency, of fever,
sore throat, weakness, pain with swallowing, change in voice, loss of
appetite, neck swelling, difficulty breathing, and nasal discharge.
|
|
|
|
|
Diphtheria
Pharyngitis An exudative
pharyngitis with a gray pseudomembrane is seen in this patient with
diphtheria. (Courtesy of Peter Strebel, MBChB, MPH, and the Journal
of Infectious Diseases.)
|
|
While the organism remains
localized to the mucosa, hematogenous spread of the exotoxin typically
produces myocarditis or peripheral neuropathies. Deaths from diphtheria
occur either from tracheobronchial obstruction by the pseudomembrane
acutely or cardiac complications during the several weeks after the
primary infection.
Differential Diagnosis
The differential diagnosis for
exudative pharyngitis is broad (see "Pharyngitis," above).
Other pathogens that can cause a membranous pharyngitis include Streptococcus
species, Epstein-Barr virus and cytomegalovirus, and Candida.
Emergency Department Treatment
and Disposition
The diagnosis of diphtheria is
initially made clinically. The definitive diagnosis is made by successful
isolation and toxigenicity testing of C. diphtheriae. Cultures
should be taken from beneath the membrane and rapidly placed on a special
culture medium containing tellurite. Histopathologic analysis may also
confirm the disease. The Centers for Disease Control and Prevention (CDC)
is investigating a new polymerase chain reaction (PCR) test for the
presence of the diphtheria toxin gene.
Treatment is dependent on making
the appropriate diagnosis. Antitoxin, only available from the CDC
(telephone: 404-639-2889), is the mainstay of therapy and must be given
before laboratory confirmation. Similarly, erythromycin or penicillin,
the drugs of choice in treating diphtheria, should be given promptly when
diphtheria is suspected. The recommended treatment course for either
agent is 14 days. Antibiotics have been shown to decrease both exotoxin
production and spread of the bacterium.
Many patients require hospital
admission for airway precautions, pulmonary support, and intravenous
hydration and antibiotics. Strict isolation is essential for patients
with diphtheria, along with proper disposal of all articles soiled by a
patient. All cases should reported to local public health officials to
assist in identifying contacts.
Clinical Pearls
1. Outcome is improved with
early treatment; thus the diagnosis of diphtheria must be made clinically
and treatment begun empirically before bacteriologic confirmation.
2. Patients with a membranous
pharyngitis need to be questioned regarding immunization, exposures, and
travel history.
3. All contacts should have a
booster dose of vaccine (TD or Td, depending on age) while nonimmune
contacts should also be given prophylactic antibiotics after a throat
swab.
4. Travelers to endemic areas
must be current with their diphtheria vaccinations.
|
|
Peritonsillar Abscess
Associated Clinical Features
Peritonsillar abscess, or quinsy,
is the most common deep neck infection. Although most occur in young
adults, immunocompromised and diabetic patients are at increased risk.
Most abscesses develop as a complication of tonsillitis or pharyngitis,
but they can also result from odontogenic spread, recent dental
procedures, and local mucosal trauma. They recur in 10 to 15% of
patients.
The pathogens involved are
similar to those causing tonsillitis, especially streptococcal species,
but many infections are polymicrobial and involve anaerobic bacteria.
Patients present with a fever, severe sore throat that is often out of
proportion to physical findings, localization of symptoms to one side of
the throat, trismus, drooling, dysphagia, dysphonia, fetid breath, and
ipsilateral ear pain.
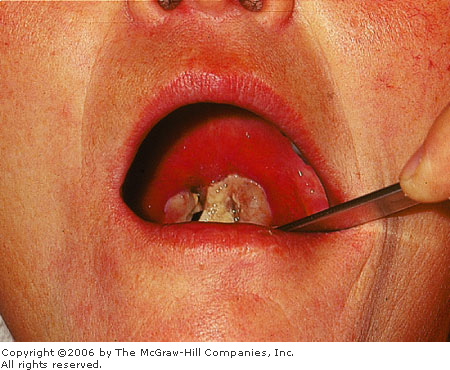
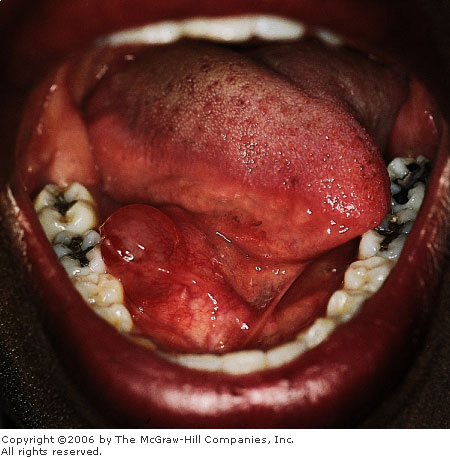
During the early stages, the
tonsil and anterior pillar are erythematous, appear full, and may be
shifted medially. Later, the uvula and soft palate are shifted to the
contralateral side (Fig. 5.27). The tonsillar pillar may feel fluctuant
and tender on palpation.
|
|
|

|
|
Peritonsillar
Abscess Acute peritonsillar
abscess showing medial displacement of the uvula, palatine tonsil,
and anterior pillar. Some trismus is present, as demonstrated by
patient's inability to open the mouth maximally. (Courtesy of Kevin
J. Knoop, MD, MS.)
|
|
Differential Diagnosis
Ludwig's angina, odontogenic neck
infections, peritonsillar cellulitis, and retropharyngeal abscesses can
be confused with peritonsillar abscesses. Angioedema has a rapid onset of
symptoms, whereas oral neoplasms develop slowly.
Emergency Department Treatment
and Disposition
Most patients with signs of an
abscess can have a needle aspiration performed as the sole surgical
drainage procedure and can expect a satisfactory outcome. Alternative
surgical drainage procedures—including incision and drainage and
abscess tonsillectomy—can be performed by an otolaryngologist or
oral surgeon. Most can be managed as outpatients on oral antibiotics
following drainage. Patients who are immunocompromised, have airway involvement,
appear toxic, or cannot tolerate oral intake require admission for
rehydration, parenteral antibiotics, and specialty consultation.
Studies to date are divided on
the incidence of penicillin-resistant organisms in peritonsillar
abscesses. Although penicillin alone is arguably a good first choice,
penicillin and metronidazole, amoxicillin with clavulanate, clindamycin,
or third-generation cephalosporins are also suitable antibiotic choices.
Clinical Pearl
1. The value of culturing
aspirates is questionable, with a review of several studies showing no
clinical benefit from the cultures unless the patient is
immunocompromised.
|
|
Uvulitis
Associated Clinical Features
The uvula is the fleshy midline
extension of the soft palate that hangs from the roof of the mouth.
Except for idiopathic, the two most common causes of uvular enlargement
are infections and angioedema. Most patients complain of a sore throat, a
gagging sensation, or a foreign-body sensation in the back of the mouth.
The infectious etiologies of
uvulitis are bacterial, including Haemophilus influenzae and
streptococci; fungal, such as Candida albicans; and viral.
Infections of the uvula are typically extensions from adjacent
infections, such as epiglottitis, tonsillitis, peritonsillar abscesses,
and pharyngitis.
With infectious uvulitis,
patients note fever, odynophagia, trismus, facial pain, hoarseness, neck
pain, and headache. On examination the uvula is red, firm, swollen, and
very tender to palpation.
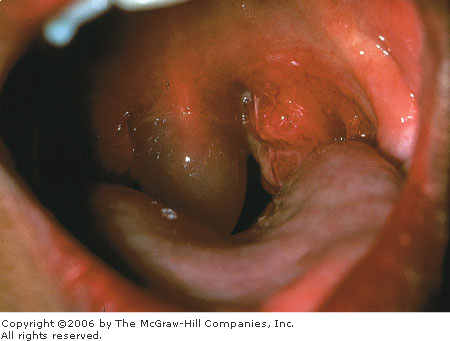
Angioedema of the uvula, known as
Quincke's disease, can be hereditary, acquired, or idiopathic.
Medications, allergens, thermal stimuli, pressure, and iatrogenic or
accidental trauma can initiate angioedema. In addition to the swollen
uvula, patients may note pruritus, urticaria, and wheezing. With uvular
edema, the angioedema may involve the face, tongue, and oropharynx.
Airway compromise is more common in angioedema of the uvula. The uvula
with angioedema appears pale, boggy, and edematous, resembling a large
white grape (uvular hydrops) (Fig. 5.28).
|
|
|
|
|
Uvulitis Angioedema of the uvula, known as Quincke's
disease. (Courtesy of Robin T. Cotton, MD.)
|
|
Differential Diagnosis
Benign polyps and neoplasms cause
asymmetry of the palate or uvula. Cellulitis and peritonsillar abscesses
may also cause uvular distortion.
Emergency Department Treatment
and Disposition
Most cases of uvulitis are benign
and self-limited. Angioedematous uvulitis is treated like any angioedema.
Administration of steroids, antihistamines—both H1 and H2
blockers, and epinephrine, either subcutaneously or nebulized, may
provide symptomatic relief. For infectious uvulitis, antibiotic coverage
is dictated by the primary source of infection. For odontogenic
infections, pharyngitis, or tonsillitis with uvulitis, penicillin,
clindamycin, or amoxicillin with clavulanate are effective. Epiglottitis
associated with uvulitis requires potent H. influenzae coverage,
such as third-generation cephalosporins. Admission is based on severity
of airway compromise and accompanying infections.
Clinical Pearls
1. Although the incidence of
concomitant epiglottitis has decreased dramatically, any airway symptom
dictates an evaluation of the hypopharynx, either by soft tissue lateral
neck radiograph, fiber-optic nasopharyngoscope, or direct laryngoscopy.
2. If the uvula itself is
causing enough airway compromise, uvular decompression by longitudinal
incisions or a partial uvulectomy can be performed.
|
|
Epiglottitis
Associated Clinical Features
Epiglottitis or supraglottitis is
an infection of the supraglottic structures including the epiglottis,
aryepiglottic folds, arytenoids, and periepiglottic soft tissues. Bacterial
epiglottitis, a rare but potentially fatal infection, is caused primarily
by Haemophilus influenzae, but Streptococcus pneumoniae,
Staphylococcus aureus, and  -hemolytic
streptococcus have been isolated. The advent of the H. influenzae B
vaccination for infants has changed what used to be a disease primarily
of children, with a peak age range from 2 to 6 years, to one found
increasingly in adults. Bacterial epiglottitis occurs most commonly in
the winter and spring but may appear at any time. -hemolytic
streptococcus have been isolated. The advent of the H. influenzae B
vaccination for infants has changed what used to be a disease primarily
of children, with a peak age range from 2 to 6 years, to one found
increasingly in adults. Bacterial epiglottitis occurs most commonly in
the winter and spring but may appear at any time.
Patients, especially children,
with acute epiglottitis appear quite ill. They present with sore throat,
fever, drooling, severe dysphagia, dyspnea, muffled or hoarse voice, and
occasionally inspiratory stridor. Patients with severe respiratory
distress assume the "tripod" position: sitting upright with the
neck extended, arms supporting the trunk, and the jaw thrust forward.
This position maximizes airway patency and caliber. Adults typically have
an indolent course with a prodromal viral illness, but many children have
a sudden onset and rapid progression to respiratory distress.
Differential Diagnosis
Croup, bacterial tracheitis,
lingual tonsillitis, and retropharyngeal abscesses are other infectious
causes of respiratory distress. Angioedema and foreign bodies cause a
sudden onset of acute respiratory distress without antecedent illnesses.
Acquired and congenital
subglottic stenosis and intrinsic and extrinsic masses may produce
similar airway symptoms.
Emergency Department Treatment
and Disposition
Airway management is paramount.
Even prior to diagnosis, children should be calmed, comforted by a
parent, and allowed to assume whatever position they feel is most comfortable.
Anesthesiology and ENT should be consulted immediately. Indications for
intubation are clinical, but severe stridor and respiratory distress are
clear reasons to intervene. Nasotracheal intubation in children is
preferred but not when performed blindly. Needle cricothyrotomy can
provide temporary oxygenation until a surgical airway is provided.
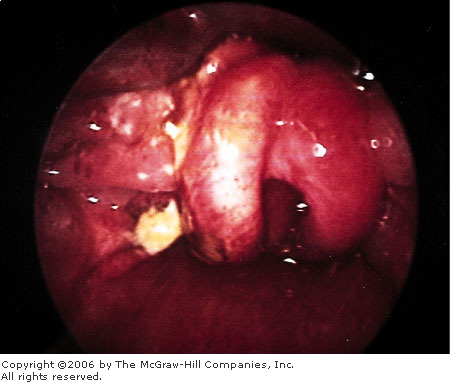
Radiographs of the neck may
reveal the classic "thumb" sign, a thickened epiglottis on the
lateral soft-tissue neck radiograph (Fig. 5.29). Visualization of the
epiglottis is possible in the stable adult patient via direct and
indirect laryngoscopy and fiberoptic nasopharyngoscopy (Fig. 5.30). The
airway orifice may be difficult to see because of the extreme distortion
of tissues. In children, the top of the swollen epiglottis may be
visualized on careful oral examination, whereas pharyngoscopy is
typically reserved for an experienced anesthesiologist or
otolaryngologist in a controlled setting.
|
|
|

|
|
Adult
Epiglottitis Soft-tissue
lateral neck radiograph of an adult with epiglottitis demonstrating
the classic "thumb" sign of a swollen epiglottis. (Courtesy
of Kevin J. Knoop, MD, MS.)
|
|
|
|
|
|
|
|
|
Adult
Epiglottitis Fiberoptic
laryngoscopy showing a red, edematous epiglottis and glottic area
with marked airway compromise in an adult with epiglottitis.
(Courtesy of Timothy L. Smith, MD.)
|
|
The mainstay of epiglottitis
treatment is antibiotics. Second- and third-generation parenteral
cephalosporins and ampicillin with sulbactam have proven efficacy in
treating epiglottitis.
Steroids or epinephrine, either
nebulized or subcutaneous, may provide some improvement in edema.
Recently, helium and oxygen gas mixtures—which, owing to their
lower density compared with air, improve the work of breathing and flow
rates—have shown promise in delaying or even preventing intubation
in some patients.
In addition to airway compromise,
complications of epiglottitis include epiglottic abscesses, meningitis,
pulmonary edema, pneumonia, and empyema (associated with H. influenzae).
Clinical Pearls
1. Transport of patients with
suspected epiglottitis must be done by an experienced transport team. The
airway must be secured before transport of all but the most stable
patients.
2. During intubation, pushing
on the patient's chest may cause a bubble to form at the airway orifice,
guiding placement of the tube.
3. Failure to intervene prior
to loss of the airway carries a sixfold increase in mortality.
|
|
Mucocele (Ranula)
Associated Clinical Features
Ranulas are mucoceles (mucous
retention cysts) that develop in the floor of the mouth, arising from
obstructed sublingual or submandibular ducts or smaller minor salivary
glands. At first the cysts are small and barely noticeable, but over time
they can expand outward or deeper into the neck (plunging ranula). Large
cysts can displace the tongue forward and upward, making the patient
uncomfortable. Unlike those with sialolithiasis, patients with ranulas
may not always notice an increase in swelling associated with eating.
Physical examination reveals a soft, minimally tender, translucent cyst
with dilated veins running over its surface (Fig. 5.31). Unlike
carcinomas, no ulceration is noted with ranulas, and they are generally
softer.
|
|
|
|
|
Ranula Sublingual ranula, or mucocele, lateral to
Wharton's duct. The patient was asymptomatic except for being aware
of the lesion. (Courtesy of Kevin J. Knoop, MD, MS.)
|
|
Differential Diagnosis
Torus mandibularis is a hard bony
growth off the lingual surface of the mandible. Obstruction of major
salivary glands is often painful and intermittent. Carcinomas of the
mouth are slower-growing and firm. Abscesses and local cellulitis also
produce sublingual swelling.
Emergency Department Treatment
and Disposition
Recognition by the physician is
essential for proper referral. Definitive treatment is excision or
marsupialization, although needle aspiration of the cyst can provide
temporary relief. Unless there is a secondary infection, no antibiotic
coverage is required.
Clinical Pearls
1. Most ranulas are painless
and are incidental findings on routine examinations.
2. Ranulas often recur,
requiring total excision of the offending salivary gland.
|
|
Sialoadenitis
Associated Clinical Features
Sialoadenitis is a general
term describing inflammation of any salivary gland. The three major
salivary gland pairs are the parotid, submandibular, and sublingual.
There are also numerous smaller salivary glands that empty into the oral
cavity and all are capable of becoming inflamed. Salivary gland disorders
have a broad spectrum of causes, including acute and chronic infections;
metabolic, systemic, and endocrine disorders; infiltrative processes;
obstructions; allergic inflammation; and neoplastic diseases. Key
features in the history are the duration and course of the symptoms,
complaints of pain, and unilateral or bilateral location.
Both viral and bacterial
infections of the salivary gland can lead to enlarged, swollen, painful
masses. Suppurative sialoadenitis is most commonly caused by Staphylococcus
aureus and is found in patients who are elderly, diabetic, or have
poor oral hygiene. It may also follow episodes of dehydration, such as
those due to surgery or debilitation. Viral sialoadenitis, such as mumps
parotitis, is the most common cause. It occurs with a concomitant viral
illness and is usually bilateral, whereas bacterial infections are
primarily unilateral.
Obstructive sialoadenitis occurs
from a stone or calculus in the salivary gland or duct, most commonly in
the submandibular gland. The flow of saliva is obstructed, causing
swelling, pain, and firmness. Patients with sialolithiasis note general
xerostomia and recurrent worsening of swelling and pain during mealtime.
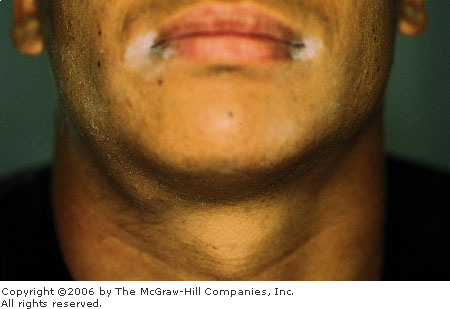
A thorough head and neck
examination is essential, especially a bimanual examination of the major
salivary glands. In suppurative sialoadenitis, purulent drainage may be
expressed from the submandibular duct (Wharton's) or parotid duct
(Stensen's), and the glands are very tender and painful to examination
(Figs. 5.32, 5.33). Sialolithiasis can manifest as enlargement of the
ducts with minimal saliva expressed on stripping and, rarely, a palpable
or visible stone (Fig. 5.34) or duct thickening. Facial radiographs are
of limited utility. Ultrasound or CT may be useful to detect abscesses.
|
|
|

|
|
Suppurative
Parotid Sialoadenitis Painful
swelling over the right parotid initially had clear saliva from
Stensen's duct. (Courtesy of Kevin J. Knoop, MD, MS.)
|
|
|
|
|

|
|
Suppurative
Parotid Sialoadenitis After applying
firm pressure on the cheek, purulent discharge is seen coming from
Stensen's duct. (Courtesy of Kevin J. Knoop, MD, MS.)
|
|
|
|
|
|
|
Suppurative
Submandibular Sialoadenitis
Unilateral submandibular swelling. (Courtesy of Jeffery D. Bondesson,
MD.)
|
|
Differential Diagnosis
Tumors of the face and
oropharynx, particularly primary salivary neoplasms and secondary lymphatic
metastases, develop slowly and produce firm, minimally tender nodules and
clear saliva. Cutaneous and odontogenic infections, angioedema variants,
and lymphadenitis may mimic sialoadenitis.
Emergency Department Treatment
and Disposition
Treatment of suppurative
sialoadenitis (Figs. 5.34, 5.35) requires antibiotics with coverage of Staphylococcus
and oral flora, rehydration, proper oral hygiene, sialogogues, local
heat, and occasionally surgical irrigation and drainage of abscesses.
Obstructive sialoadenitis is rarely an emergency. Most salivary stones
(Fig. 5.36) pass spontaneously without complication, and patients can be
discharged home on lozenges to stimulate salivary secretions and expel
the stone. Prompt follow-up of sialoadenitis is essential to prevent
possible morbidity and mortality associated with infections or neoplasms.
|
|
|

|
|
Suppurative
Submandibular Sialoadenitis
After applying firm pressure, purulent discharge is seen coming from
Wharton's duct. (Courtesy of Jeffery D. Bondesson, MD.)
|
|
|
|
|

|
|
Sialolithiasis A stone is seen at the orifice of Wharton's
duct. (Courtesy of David P. Kretzschmar, DDS, MS.)
|
|
Clinical Pearls
1. Examine secretions of both
mouth and eyes and elicit any history of dry eyes, keratoconjunctivitis,
cutaneous lesions, or rheumatoid arthritis to establish the diagnosis of
a systemic disorder.
2. Medications such as
antihistamines, psychotropic drugs, and those possessing atropine-like
side effects can cause xerostomia.
3. Lack of improvement on
antibiotics suggests an abscess or multiple loculated abscesses that
require drainage.
|
|
Sinusitis
Associated Clinical Features
Sinusitis is an inflammation of
the paranasal sinuses. Sinusitis can be classified as acute, subacute, or
chronic; purulent or sterile; and allergic or nonallergic. All share an
impairment of mucus clearance. Most cases of bacterial sinusitis are
associated with antecedent viral upper respiratory tract infection.
Maxillary sinusitis is the most
common form of sinusitis and is associated with paranasal facial pain,
maxillary dental pain, purulent rhinorrhea (Fig. 5.37), retroocular pain,
and conjunctivitis. Ethmoid sinusitis is more common in children and
produces a low-grade fever and periorbital pain. Frontal sinusitis can cause
a severe headache above the eyes, which is exacerbated by leaning
forward; a low-grade fever; upper lid edema; and rhinorrhea. Sphenoid
sinusitis is fortunately rare. Patients classically complain of a vertex
headache and retroocular pain. Owing to its intracranial location,
sphenoid sinusitis can involve several cranial nerves, the pituitary
gland, and the cavernous sinus. Involvement of all sinus cavities is
referred to as pansinusitis. Important complications of sinusitis include
periorbital and orbital cellulitis, cavernous sinus thrombosis, and
intracranial abscess (Figs. 5.38 and 5.39).
|
|
|

|
|
Sinusitis Purulent drainage from the maxillary sinus
ostium in a patient with maxillary sinusitis. Drainage may not always
be apparent, since the ostium may be occluded from swelling and
inflammation. (Courtesy of Robin T. Cotton, MD.)
|
|
|
|
|
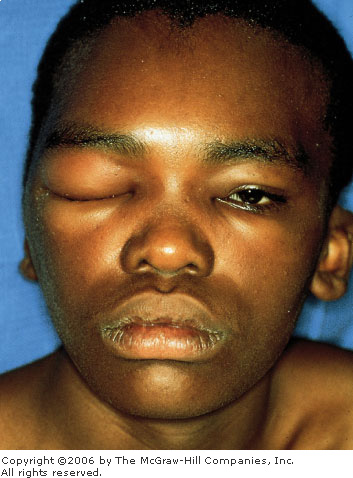
|
|
Sinusitis Adolescent with pansinusitis complicated by
periorbital cellulitis. The patient was also found to have
osteomyelitis of the frontal cortex (Pott's puffy tumor). (Courtesy
of Robin T. Cotton, MD.)
|
|
|
|
|

|
|
Sinusitis Waters view of the patient in Fig. 5.37
showing an air-fluid level in the right frontal and bilateral
maxillary sinuses. (Courtesy of Robin T. Cotton, MD.)
|
|
Patients with Pott's puffy tumor
(a rare osteomyelitis of the cranium from direct extension of a frontal
sinusitis) present with a boggy, tender swelling above the eye.
A careful history is important in
patients presumed to have sinusitis. Recent steroid use, prodromal viral
illness, dental work, and facial trauma are important temporal events. A
history of septal deviation or defects, cystic fibrosis, smoking, and
cocaine use also increases the risk of sinusitis.
Imaging modalities include
transillumination of the maxillary sinuses, plain radiographs, CT, and
MRI. CT is the most sensitive and specific technique and allows for
better delineation of the sphenoid and ethmoid sinuses.
Common bacterial isolates are Haemophilus
influenzae, Streptococcus pneumoniae (together representing 60 to 70%
of all bacterial causes), Streptococcus pyogenes, Staphylococcus
aureus, and Moraxella catarrhalis. Immunocompromised patients
are susceptible to fungal infections, including Aspergillus and Mucor
species.
Differential Diagnosis
Other infections—including
facial cellulitis, early herpes zoster, odontogenic infections, and
otitis media—may produce similar signs and symptoms. Neoplasms and
trigeminal neuralgia should also be considered.
Emergency Department Treatment
and Disposition
For acute bacterial sinusitis,
amoxicillin, macrolides, and trimethoprim-sulfamethoxazole are
appropriate agents. Refractory cases or immunocompromised patients
require broader-spectrum antibiotics such as amoxicillin with
clavulanate, clarithromycin, second- or third-generation cephalo-sporins,
or the newer fluoroquinolones. Treatment for up to 3 weeks may be
necessary.
Decongestants reduce local edema,
increase air movement within the sinuses, and decrease local secretions.
A short course of topical oxymetazoline or phenylephrine as well as oral
pseudoephedrine for 10 days helps minimize secretions and assists in
maintaining ostia patency. Humidified air, steam, or saline nasal sprays
also facilitate drainage. Patients should be strongly encouraged to stop
smoking.
Parenteral steroids are not used
in acute or recurrent sinusitis. Inhaled steroids, such as triamcinolone,
have a role in allergic and chronic sinusitis.
Referral or follow-up by an
otolaryngologist or primary care provider should be made for all patients
within 3 weeks for routine cases. Patients with comorbid illnesses or
more complicated sinusitis should be admitted for parenteral antibiotic
therapy and supportive care.
Clinical Pearls
1. Chronic sinusitis may be due
to mucoid retention cysts, deviated septum, or polyps, which are often
visible on plain radiographs. Refer these patients for possible surgery.
2. Physicians must consider
fungal etiologies in patients with comorbid illnesses.
|
|