|
Note: Large images and
tables on this page may necessitate printing in landscape mode.
Copyright
©2006 The McGraw-Hill Companies. All rights reserved.
Emergency
Medicine Atlas > Part 1. Regional
Anatomy > Chapter 6. Mouth > Oral
Trauma >
|
Tooth Subluxation
Associated Clinical Features
Tooth subluxation refers to the
loosening of a tooth in its alveolar socket. Traumatic oral injury is a
common mechanism by which dental subluxation occurs; however, infection
and chronic periodontal disease may also produce loosening of teeth.
Gingival lacerations and alveolar fractures are commonly associated with
dental subluxations. Subluxated, or loosened, teeth are diagnosed by
applying gentle pressure to the teeth with a tongue blade or fingertip.
Mild displacement may also be noted (Fig. 6.1). Blood along the crevice
of the gingiva, where the tooth meets the gingiva, is also a sign of
subluxation. Various degrees of tooth mobility may be noted on
examination.
|
|
|

|
|
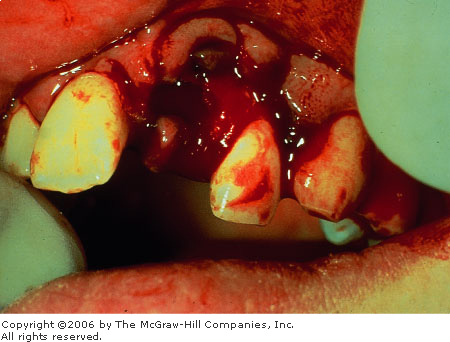
Tooth
Subluxation Note the presence
of blood along the crevice of the gingival margin of both central
incisors—an indication of subluxation following trauma. Mild
displacement of the subluxated teeth is noted. (Courtesy of James F.
Steiner, DDS.)
|
|
Differential Diagnosis
Dental impaction and alveolar
ridge fracture should be considered and ruled out clinically and with
radiographs.
Emergency Department Treatment
and Disposition
1. Primary teeth:If the
subluxated tooth is forced into close proximity to the underlying
permanent tooth, extraction by a dentist or oral surgeon is indicated.
Otherwise, the patient should be instructed to follow a soft diet for 1
to 2 weeks, allowing the tooth to reimplant.
2. Permanent teeth:If
the tooth is unstable, it should be temporarily immobilized. This may be
accomplished with gauze packing, a figure-eight suture around the tooth
and an adjacent tooth, aluminum foil, or a special periodontal dressing
(Coe-Pak). The patient should be referred for dental follow-up.
Clinical Pearls
1. Any evidence of tooth
mobility following trauma is a subluxation by definition.
2. Always consider the
possibility of an associated underlying alveolar fracture.
3. Clinically subluxated teeth
may actually represent an occult root fracture.
|
|
Tooth Impaction (Intrusive Luxation)
Associated Clinical Features
Impacted or intruded teeth result
when a tooth is forced deeper into the alveolar socket or surrounding
tissues as a result of trauma (Fig. 6.2). The force causing the impaction
may be directly on the incisal or occlusal surface of the tooth. The tooth
appears shorter than its contralateral partner. The primary dentition is
more prone to impaction than permanent teeth. An impacted tooth may be
partially visible or completely hidden by the gingiva and buried in the
alveolar process. Completely impacted teeth may erroneously be considered
avulsed until a radiograph demonstrates the intruded position. The apex
of a completely impacted permanent central incisor may be driven through
the alveolar bone into the floor of the nostril, causing a nosebleed. The
apex of the incisor may be noted on examination of the nostril floor.
Primary dentition apices tend to be driven into the thin vestibular bone.
Other associated injuries include possible alveolar fractures, dental
crown or root fractures, as well as oral mucosal and gingival
lacerations. Dental pulp necrosis occurs in 15 to 50% of cases.
|
|
|

|
|
Tooth
Intrusion This impaction
injury with multiple anterior maxillary tooth involvement shows
various degrees of tooth impaction. Also note the complete absence of
a central incisor. This may indicate a complete intrusion into the
alveolar socket or an avulsion of the tooth. Radiographic studies are
required when a tooth's location is in question. (Courtesy of James
F. Steiner, DDS.)
|
|
Differential Diagnosis
Tooth avulsions and fractures
should be considered in the differential diagnosis because of a similar
mechanism of injury. Completely impacted teeth may simulate an avulsed
tooth in appearance. Lateral luxation may result in teeth that appear
shortened and angulated or may simulate a partial impaction. Traumatic
injury to gingiva around a normal erupting tooth may be mistaken for an
impaction. Impacted teeth tend to emit a high metallic sound on
percussion testing with a metallic instrument, similar to ankylosed
teeth. Normal teeth do not produce a metallic sound, whereas subluxated
teeth produce a dull sound on percussion. Radiographs also aid in
differentiating these dental injuries.
Emergency Department Treatment
and Disposition
Primary teeth that are impacted
usually reerupt and reposition spontaneously within 1 to 3 months.
Surgical intervention is indicated if spontaneous reduction does not
occur within this time frame. Any intruded primary tooth whose apex is
displaced toward or impacts on the follicle of its permanent successor
should be extracted. These patients should have dental follow-up and be
monitored clinically and radiographically for 1 year. Permanent teeth do
not reerupt. Surgical reduction is indicated to prevent complications
such as external root resorption and loss of supporting bone. Orthodontic
repositioning and splinting is generally carried out over 3 to 4 weeks.
Follow-up for a minimum of 1 year is recommended.
Clinical Pearls
1. An undiagnosed impacted
tooth is predisposed to infection and can have a poor cosmetic result.
2. The maxillary incisors are
the most commonly affected teeth.
3. Only the immature primary
teeth will reerupt; the permanent teeth will not.
|
|
Tooth Avulsion
Associated Clinical Features
Avulsion is the total
displacement of a tooth from its socket (Fig. 6.3). There is usually a
history of trauma; however, infectious etiologies can also cause an
avulsion. Complete disruption of the periodontal ligament fibers from the
affected tooth occurs as a result. Various degrees of bleeding from the
socket and surrounding gingiva may be noted. Depending on the mechanism
of injury, there may be an associated underlying alveolar fracture.
Prompt inquiry into the location of any unaccountable tooth is indicated.
Radiographic evaluation to rule out aspiration or soft tissue entrapment
is indicated when the tooth's location is in question.
|
|
|
|
|
Tooth
Avulsion Avulsion injury with
angulation and displacement of teeth from the alveolar socket.
(Courtesy of James F. Steiner, DDS.)
|
|
Differential Diagnosis
Complete tooth impactions may
appear to be an avulsion. Dental fractures with retained tooth fragments
in the alveolar socket may also simulate an avulsion. Radiographs should
be taken to rule out an intrusion or dentoalveolar fracture.
Emergency Department Treatment
and Disposition
Permanent teeth should be
replaced in their sockets as soon as possible. The tooth should first be
rinsed with saline but not scrubbed, and the root should not be handled.
Successful reimplantation depends on the survival of periodontal ligament
fibers, which are attached to the root of the avulsed tooth. The tooth
should be placed in the socket and emergent dental consultation obtained.
Antibiotics against mouth flora (penicillin, clindamycin) should be
administered, as well as tetanus prophylaxis. If not replaced, the
avulsed tooth should be stored in the mouth of the patient or parent or
in a container of milk. Normal saline can be used, but water should not
be used. Hank's solution is the ideal storage medium for the avulsed
tooth until reimplantation. Primary teeth are not reimplanted, but
follow-up should be obtained, as a procedure may be needed to maintain
tooth spacing until the permanent tooth erupts.
Clinical Pearls
1. Reimplantation of primary
avulsed teeth in patients younger than 6 years may interfere with
eruptions of permanent teeth because of ankylosing and fusion to the
bone.
2. Successful reimplantation of
an avulsed tooth is best achieved within the first 30 min after an avulsion.
3. Storage and transport media
in decreasing order for preserving tooth viability include Hank's
balanced salt solution or a tissue culture medium (Save-A-Tooth), cool
low-fat or skim milk, saline, and saliva.
|
|
Tooth Fractures
Associated Clinical Features
Anatomically, each tooth has
crown and root portions. Externally, the crown is covered with white
enamel and the root portion with cementum. The cementoenamel junction
(cervical line) is where the crown and root meet. The yellow-to-tan
dentin is the second innermost layer and composes the bulk of the tooth.
The red-to-pink pulp tissue is located in the center of the tooth and
furnishes the neurovascular supply to the tooth. The Ellis classification
system, while considered by some as inadequate, is still commonly used to
describe tooth fractures above the cervical line in anterior teeth (Fig.
6.4):
|
|
|
|
|
Tooth
Fractures Enamel, dentin, and
pulp are the anatomic landmarks used in the Ellis classification of
tooth fractures.
|
|
Ellis class I: Involves the
enamel only (Fig. 6.5).
Ellis class II: Involves the
enamel plus exposure of the dentin (Fig. 6.6). The patient may complain
of temperature sensitivity.
Ellis class III: Fracture
extends into the pulp. A pink or bloody discoloration on the fracture
surface is diagnostic of this type of fracture (Fig. 6.7). The patient
may have severe pain but may also have no pain due to loss of nerve
function.
Tooth fractures may also occur
below the cementoenamel junction. These dental root fractures are
commonly missed on initial evaluation. Bleeding may be observed at the
gingival crevice with associated tooth tenderness on percussion.
|
|
|

|
|
Ellis
Class I Tooth Fracture Note
the fracture of the left upper central incisor. The sole involvement
of the enamel is consistent with an Ellis type I injury. (Courtesy of
James F. Steiner, DDS.)
|
|
|
|
|

|
|
Ellis
Class II Tooth Fractures
Bilateral maxillary central incisor injuries with exposed enamel and
dentin consistent with an Ellis class II fracture. (Courtesy of James
F. Steiner, DDS.)
|
|
|
|
|

|
|
Ellis
Class III Tooth Fracture A
fracture demonstrating blood at the exposed dental pulp. This sign is
pathognomonic for an Ellis class III fracture. (Courtesy of Kevin J.
Knoop, MD, MS.)
|
|
Differential Diagnosis
Subluxation, alveolar fracture,
avulsion, or a traumatic impaction are in the differential. Dental
fractures may also be occult and occur below the gum line or at the level
of root. Radiographic evaluation will aid in differentiating these
conditions.
Emergency Department Treatment
and Disposition
Ellis class I: Pain control
should be initiated. Rough tooth edges may be smoothed with an emery
board. Immediate dental referral within 24 h is indicated when soft
tissue injury is caused by sharp pieces of the tooth.
Ellis class II: Patients
under 12 years of age have less dentin than older patients and are at
risk for infection of the pulp. They should have a calcium hydroxide
dressing placed, coverage with gauze or aluminum foil, and see a dentist
within 24 h. Older patients should be advised to see a dentist within 24
to 48 h.
Ellis class III: This is
considered a dental emergency, and immediate dental consultation is
indicated. Delay in treatment may result in severe pain and abscess
formation.
Root Fractures: Early
reduction, immobilization, and splinting are indicated once diagnosed. A
commercial stabilizing compound (Coe-Pak) is available for this purpose.
Dental referral is advised within 24 to 48 h. Most teeth sustaining root
fractures maintain pulpal vitality and tend to heal.
Clinical Pearls
1. Check for tooth mobility on
initial examination to aid in differentiating mobility involving the
entire tooth from involvement of only the incisal segment.
2. Consider nonaccidental
trauma when dental injuries occur in young children.
|
|
Alveolar Ridge Fracture
Associated Clinical Features
The alveolus is the tooth-bearing
segment of the mandible and maxilla. Fracture of the alveolar process
tends to occur more often in the thinner maxilla than in the mandible.
However, the most common type of mandibular fracture is an alveolar
fracture. The anterior alveolar processes are at greatest risk for
fracture due to more direct exposure to trauma (Fig. 6.8). Exposed pieces
of bone may be noted in alveolar fractures. Various degrees of tooth
mobility and gingival bleeding may be noted. Both subluxation and
avulsion of teeth may be associated with underlying alveolar fractures of
the mandible or maxilla.
|
|
|

|
|
Alveolar
Ridge Fracture Note the
exposed alveolar bone segment and associated multiple tooth
involvement. Attempts should be made to maximally preserve all viable
tissue. (Courtesy of Alan B. Storrow, MD.)
|
|
Differential Diagnosis
Fractures of the mandible and
maxilla may both present with pain, deformity, malocclusion, and
bleeding, which may resemble an alveolar fracture. Gingival lacerations
with significant tissue damage may be associated with an underlying
fracture and should be considered.
Emergency Department Treatment
and Disposition
Preservation of as much viable
tissue as possible is important. Do not remove any segment of alveolus
firmly attached to the mucoperiosteum. Significant cosmetic deformity may
result from alveolar bone loss. The involved alveolar segment should have
a saline-soaked gauze applied with gentle direct pressure. Any avulsed
teeth should also be preserved. The patient's tetanus status should be
addressed. Antibiotic therapy with penicillin, clindamycin, or a
cephalosporin should also be considered, particularly if bony fragments
are exposed. Oral surgery consultation should be obtained for possible
wire stabilization, arch bar fixation, and follow-up.
Clinical Pearls
1. Always consider the
possibility of an associated cervical spine injury when evaluating
patients with facial trauma.
2. If an avulsed tooth is
associated with an alveolar fracture, the clinician should inquire about
its location. If unaccounted for, consider the possibility of aspiration
or soft tissue entrapment.
|
|
Temporal Mandibular Joint (TMJ) Dislocation
Associated Clinical Features
Dislocation generally results
from direct trauma to the chin while the mouth is open or, more commonly,
in predisposed individuals after a vigorous yawn. Opening the mouth
excessively wide while eating or laughing may also result in dislocation.
Acute dislocation occurs when the mandibular condyles displace forward
and become locked anterior to the articular eminence. Muscle spasm
contributes to prevention of spontaneous relocation. Weakness of the
temporomandibular ligament, an overstretched joint capsule, and a shallow
articular eminence are predisposing factors. Patients usually present
with an inability to close an open mouth (Fig. 6.9). Other associated
symptoms include pain, discomfort, and facial swelling near the
temporomandibular joint (TMJ). Difficulty speaking and swallowing is
common. Anterior dislocations are most common; however, posterior
dislocation may occur with significant force in association with a
basilar skull fracture. Unilateral dislocation results in deviation of
the mandible to the unaffected side (Fig. 6.10).
|
|
|
|
|
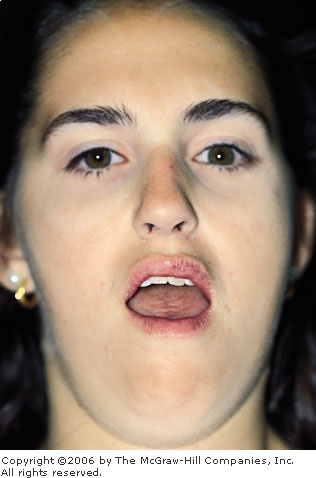
TMJ
Dislocation (Bilateral) This
patient awoke from sleep with the inability to close her mouth. Note
the dry lips and tongue secondary to prolonged exposure. Symmetric
dislocations are more common than unilateral injury. (Courtesy of
Warren K. Russell, MD.)
|
|
|
|
|

|
|
TMJ
Dislocation (Unilateral) Note
the asymmetric jaw deviation toward the unaffected side. Always
consider the possibility of an associated underlying fracture or
cervical spine injury. (Courtesy of Frank Birinyi, MD.)
|
|
Differential Diagnosis
TMJ hemarthrosis, dystonic
reactions, and hysterical dislocation can mimic the true process of TMJ
dislocation. Unilateral or bilateral mandibular fractures should also be
strongly considered, particularly if there is a history of facial trauma.
Emergency Department Treatment
and Disposition
Acute reduction of pain, muscle
spasm, and anxiety is achieved using reassurance, analgesics, and muscle
relaxants. Panorex or TMJ x-ray films (pre- and postreduction) are
obtained to exclude a fracture (Fig. 6.11). The patient is typically
treated in the sitting position. While facing the patient, the physician
grasps the angles of the mandible with both hands. The thumbs are wrapped
in gauze for protection and rest on the occlusive surfaces of the molars
while downward and backward pressure is applied until the condyle slides
back into the articular eminence. Instruct the patient to avoid
excessively wide mouth opening while eating and yawning for 3 to 4 weeks.
Apply warm compresses to the TMJ areas. A soft diet for 1 week is advised,
as is the use of nonsteroidal anti-inflammatory drugs as needed. Dental
follow-up should be arranged.
|
|
|

|
|

|
|
TMJ
Dislocation A. Radiographic
demonstration of an anterior TMJ dislocation. The location of the
condyle is indicated by the open arrow. The position of the
mandibular notch is indicated by the closed arrow. B. Postreduction
radiograph showing normal positioning of the condyle in the
mandibular notch. (Courtesy of Edwin D. Turner, MD.)
|
|
Clinical Pearls
1. Approximately 70% of the general
population can subluxate the mandible partially and then spontaneously
reduce it.
2. TMJ dysfunction secondary to
a neuroleptic or antipsychotic medication–related dystonic reaction
is treated with diphenhydramine or benztropine.
3. When trauma is the cause of
TMJ dislocation, maintain a high index of suspicion for cervical spine
injury.
|
|
Tongue Laceration
Associated Clinical Features
Tongue lacerations are usually
the result of oral trauma and tongue biting (Fig. 6.12). Injuries to the
tongue or mouth floor can cause serious hemorrhage and potential airway
compromise. Careful examination of the oral cavity for associated
injuries is necessary. Specifically, the injury or absence of teeth
should be ascertained. Dorsal tongue lacerations may be associated with a
concurrent ventral laceration sustained from the mandibular teeth.
Closely inspect the wound for possibly entrapped dental elements.
|
|
|
|
|
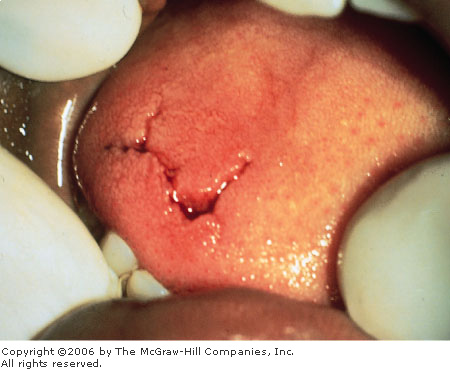
Tongue
Laceration A stellate tongue
laceration that does not require suturing is shown. The ventral
aspect of the tongue should be examined for additional lacerations
sustained from the mandibular teeth. (Courtesy of James F. Steiner,
DDS.)
|
|
Differential Diagnosis
Superficial tongue abrasions,
oral mucosal, and gingival lacerations may all bleed profusely and cause
difficulty localizing the exact source. Any of the aforementioned
lacerations may also accompany a tongue laceration. A detailed
examination of the entire oral cavity is indicated.
Emergency Department Treatment
and Disposition
Most lacerations to the tongue do
not mandate surgical repair. A generous blood supply results in
spontaneous repair of most tongue defects. An exception to this rule is
lacerations involving the tip, where rapid healing may produce a
"forked tongue." Lacerations greater than 1 cm in length that
gape widely, actively bleed, or those involving a lateral margin are best
stabilized by a few well-placed sutures; 4-0 black silk or preferably
absorbable suture (such as chromic gut) should be used. Place sutures
using large bites to include both mucosa and muscle. Laceration repair,
if opted for in children, is best carried out in a controlled environment
under appropriate anesthesia. Anesthesia of the anterior two-thirds of
the tongue is obtained using a regional inferior alveolar nerve block
(blocks the lingual nerve on the ipsilateral side). Local anesthesia may
also be used. Tongue lacerations involving the floor of the mouth or
having persistent bleeding may result in tongue swelling and airway
compromise. Consultation for admission with airway surveillance may be
indicated.
Clinical Pearls
1. If repair is elected, use an
absorbable or braided suture material. Multiple well-secured knots should
be placed, as tongue motion tends to untie suture material.
2. Extensive complex tongue
lacerations are at risk for infection and should be prophylactically
treated with antibiotics for oropharyngeal flora.
|
|
Vermilion Border Lip Laceration
Associated Clinical Features
Anatomically, the vermilion
border of the lips represents a transition area from mucosal tissue to
skin. Lip lacerations involving the vermilion border (Fig. 6.13) present
a unique clinical situation, since inadequate repair may cause an
unacceptable cosmetic result. Marked tissue edema is frequently noted
with most lip trauma, which may distort the anatomy. Vermilion border
lacerations may be partial or full thickness through the lip to the
mucosal surface. An associated underlying gingival or dental injury is a
common finding.
|
|
|

|
|
|
|
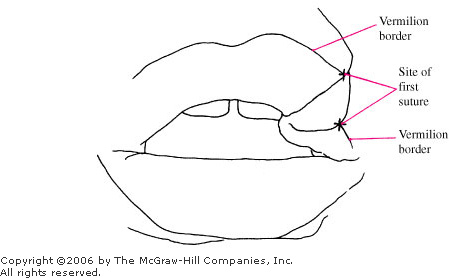
Vermilion
Border Lip Laceration A lip
laceration with disruption of the vermilion border. Wound repair
begins at the vermilion-skin junction for a good cosmetic result.
(Courtesy of Kevin J. Knoop, MD, MS.)
|
|
Differential Diagnosis
Vermilion border lip hematomas,
abrasions, and soft tissue swelling may mimic a true laceration involving
the vermilion border. Careful examination of the facial and mucosal
surfaces of the lip help differentiate these entities.
Emergency Department Treatment
and Disposition
Accurate vermilion margin
reapproximation is the goal of lip repairs. An unapproximated vermilion
margin of 2 mm or greater results in a cosmetic deformity and
occasionally a puckering defect. A regional block of the mental or
infraorbital nerve is recommended for anesthesia to avoid additional
tissue edema and anatomic distortion produced by local infiltration.
After closure of the deeper tissue, the first skin suture is always
placed at the vermilion border to reestablish the anatomic margin. Using
5-0 or 6-0 nylon, suturing should continue along the vermilion surface
until the moist mucous membrane is noted. Deep or through-and-through
lacerations involving the vermilion border should be closed in layers.
The deep muscular and dermal layer may be closed with 3-0 or 4-0 chromic
or Vicryl sutures, and the skin with 6-0 nylon sutures. Mucosal layers
are loosely reapproximated with 4-0 absorbable suture or silk. The
patient should be given wound care instructions. Follow-up for wound
evaluation and possible suture removal in 5 to 7 days should be arranged.
Clinical Pearls
1. A vermilion border with as
little as 2 mm of malalignment may produce a cosmetically noticed defect.
2. Always place the first skin
suture in the vermilion border in any lip laceration involving this area.
|
|
Gingival Abscess (Periodontal Abscess)
Associated Clinical Features
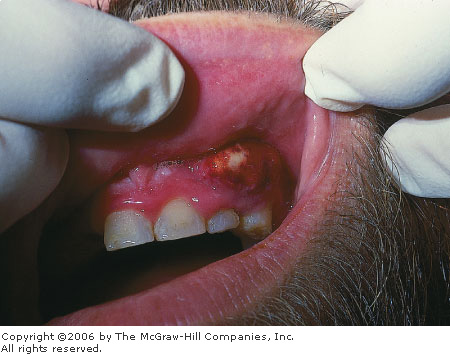
Gingival abscesses tend to
involve the marginal gingiva and result from entrapment of food and
plaque debris in a gingival pocket with subsequent staphylococcal,
streptococcal, anaerobic, or mixed bacterial overgrowth, leading to
abscess formation. Localized swelling, erythema, tenderness, and possible
fluctuance in the space between the tooth and the gingiva (the so-called
pocket) is the usual location. There may be spontaneous purulent drainage
from the gingival margin, or an area of pointing may be seen. In cases of
acute gingival abscess formation, pus may be expressed from the gingival
margin by gentle digital pressure. When the gingival abscess involves the
deeper supporting periodontal structures, it is referred to as a
periodontal abscess (Fig. 6.14). This may present as a fluctuant
vestibular abscess or with a draining sinus that opens onto the gingival
surface.
|
|
|

|
|
Periodontal
Abscess Localized gingival
swelling, erythema, and fluctuance are seen in this periodontal
abscess with spontaneous purulent drainage. (Courtesy of Kevin J.
Knoop, MD, MS.)
|
|
Differential Diagnosis
Periapical abscesses are deep and
not obvious on inspection. They usually present as tenderness to
percussion or pain with chewing over the involved tooth. A parulis may
also simulate a gingival abscess; however, a parulis represents the
cutaneous manifestation of a deeper periapical abscess. Unlike a parulis
or periapical abscesses, gingival abscesses are not usually associated
with dental caries or fillings. Pericoronal abscesses tend to involve the
gingiva overlying a partially erupted third molar.
Emergency Department Treatment
and Disposition
The initial management is a small
incision with drainage and warm saline irrigation. Removal of entrapped
food and debris is performed. Oral antibiotic therapy with penicillin,
clindamycin, tetracyclines, or macrolides is recommended. Analgesics
should be provided along with dental follow-up. The patient's tetanus
status should be addressed.
Clinical Pearls
1. Patients with gingival
abscesses are usually afebrile.
2. Consider more extensive
abscess formation and oral disease processes in the febrile
toxic-appearing patient.
3. Patients with chronic, deep
periodontal abscesses complain of dull, gnawing pain as well as a desire
to bite down on and grind the tooth.
|
|
Periapical Abscess (Dentoalveolar Abscess)
Associated Clinical Features
Acute pain, swelling, and mild
tooth elevation is characteristic of a periapical abscess. Exquisite
sensitivity to percussion or chewing on the involved tooth is a common
sign. The involved tooth may have had a root canal treatment, a filling,
or a dental carie. Periapical abscesses may enlarge over time and
"point," internally on the lingual or buccal mucosal surfaces
or extraorally with swelling and redness of the overlying skin (Fig.
6.15). Occasionally these lesions may tract up to the alveolar periosteum
and gingival surface to form a parulis ("gumboil") (Fig. 6.16).
Radiographically, these abscesses appear as well-circumscribed areas of
radiolucency at the dental apex or along the lateral aspect of the root
(Fig. 6.17). Early acute periapical abscesses may not demonstrate any
radiographic changes. Both deep periodontal and periapical abscesses may
have sinuses draining purulent material onto the gingival surface. If the
infection is allowed to progress, it can erode through the nearest
cortical bone, manifesting itself in a variety of locations (Fig. 6.18).
|
|
|

|
|
Periapical
Abscess This periapical
abscess points externally, to the overlying skin. (Courtesy of Robin
Cotton, MD.)
|
|
|
|
|
|
|
"Gumboil"
(Parulis) This lesion is an
extension of a periapical abscess. It is differentiated from a
periodontal abscess by tenderness to percussion. (Courtesy of Alan B.
Storrow, MD.)
|
|
|
|
|

|
|

|
|
Periapical
Abscess A. Note the
well-defined radiolucent area at the apex and lateral root of the
tooth in this radiograph. (Courtesy of James L. Kretzschmar, DDS, MS.)
B. This panorex film shows several areas consistent with periapical
abscesses. (Courtesy of David P. Kretzschmar, DDS, MS.)
|
|
|
|
|

|
|
Odontogenic
Abscesses As infection
progresses from the pulp at the tooth apex, it erodes through the
bone and can express itself in a variety of places. This illustration
notes several possible locations or spaces. (Adapted with permission
from Cummings C, Schuller D (eds): Otolaryngology Head and Neck
Surgery. Chicago: Mosby-Year Book; 1986.)
|
|
Differential Diagnosis
Gingival or deep periodontal
abscess, buccal space abscess, and unilateral sublingual, parapharyngeal,
and submandibular space abscesses should all be considered in the
differential diagnosis. All the aforementioned may present with oral
pain, tenderness, facial swelling, and possible fever. Panorex films,
dental radiographs, or a computed tomography (CT) scan may aid in making
the diagnosis.
Emergency Department Treatment
and Disposition
Nonsteroidal anti-inflammatory
drugs (NSAIDs) or oral narcotics for pain should be administered as well
as oropharyngeal antibiotic therapy. A regional nerve block may be
performed with a local anesthetic agent for more immediate temporary
relief. Administer tetanus toxoid if indicated. Dental consultation or
follow-up in 1 to 2 days is recommended for endodontic evaluation or
possible extraction of the involved tooth. Incision and drainage along
with saline irrigation and prompt referral constitutes the initial
treatment of a parulis.
Clinical Pearls
1. More than one tooth may be
involved simultaneously.
2. Exquisite tenderness and
pain on tooth percussion is a key feature on physical examination and
identifies the involved tooth.
3. Periapical abscesses are
almost always associated with carious or nonviable teeth.
|
|
Pericoronal Abscess
Associated Clinical Features
A partially erupted or impacted
third molar (wisdom tooth) is the most common site of pericoronitis and
pericoronal abscesses. The accumulation of food and debris between the
overlying gingival flap and crown of the tooth sets up the foci for
pericoronitis and subsequent abscess formation. The gingival flap becomes
irritated and inflamed. The area is also repeatedly traumatized by the
opposing molar tooth and may interfere with complete jaw closure as
swelling and tenderness increase. The inflamed gingival process may
eventually become infected and form a fluctuant abscess (Fig. 6.19). Foul
taste, inability to close the jaw, and fever may occur. Swelling of the
cheek and angle of the jaw as well as localized lymphadenopathy are also
characteristic. More advanced disease may spread posteriorly to the base
of the tongue and oropharyngeal area. Potential spread into the deep
cervical spaces is also an important concern with extensive processes.
|
|
|
|
|
Pericoronal
Abscess Note the inflammed
fluctuant gingival tissue approximating the incompletely erupted
third molar. (Courtesy of James F. Steiner, DDS.)
|
|
Differential Diagnosis
Ludwig's angina, peritonsillar
abscess, gingival abscess, buccal space abscess, and a severe periapical
abscess may all present similarly to a pericoronal abscess. Ludwig's
angina and peritonsillar abscesses are, in fact, potential sequelae of
acute pericoronitis and pericoronal abscesses.
Emergency Department Treatment
and Disposition
Superficial incision and drainage
with warm saline irrigation may be performed initially in the ED.
Adequate analgesia and antibiotic coverage should be provided.
Consultation or referral to an oral maxillofacial surgeon for follow-up
is indicated for possible extraction of the involved teeth.
Clinical Pearls
1. Pericoronitis and abscess
formation rarely occur in the pediatric population and tend to be late
adolescent and adult processes.
2. The mandibular third molar
is the most commonly involved tooth.
3. Airway compromise is a
potential complication with posterior extension of a pericoronal abscess.
|
|
Buccal Space Abscess
Associated Clinical Features
The buccal space lies
anatomically between the buccinator muscle and the overlying superficial
fascia and skin. The maxillary second and third molars are the usual
source of infection contributing to buccal space abscesses. Infection
from the involved teeth erodes through the maxillary alveolar bone
superiorly into the buccal space (Fig. 6.20). Rarely, the third
mandibular molar may be the source. In this instance, the infection
erodes through the mandibular alveolar bone inferiorly into the buccal
space. These patients present with unilateral facial swelling, redness,
and tenderness to the cheek (Fig. 6.21). Trismus is generally not
present.
|
|
|
|
|
Buccal
Space Anatomy The buccal space
lies between the buccinator muscle and the overlying skin and
superficial fascia. This potential space may become involved by
maxillary or mandibular molars. (Adapted with permission from
Cummings C, Schuller D (eds): Otolaryngology Head and Neck
Surgery, 2d ed. Chicago: Mosby-Year Book; 1993.)
|
|
|
|
|

|
|
Buccal
Space Abscess Note the ovoid
cheek swelling with sparing of the nasolabial fold. This finding,
along with accompanying redness and tenderness, helps to identify
buccal space abscess formation. (Courtesy of Michael J. Nowicki, MD.)
|
|
Differential Diagnosis
Canine space abscess,
parapharyngeal abscess, facial cellulitis, Ludwig's angina, and
masticator space abscess formation are all conditions that may resemble
buccal space abscesses. Parotid gland enlargement due to mumps and
suppurative bacterial parotitis should also be considered. The former
lacks erythema and warmth of the overlying skin, while the latter is
accompanied by trismus and the ability to express pus from Stensen's
duct. Inspection of all the maxillary and third mandibular molar teeth is
essential to help make the diagnosis. CT scan can aid in localizing the
space involved.
Emergency Department Treatment
and Disposition
Parenteral antibiotic therapy
with penicillin, clindamycin, or a third-generation cephalosporin is
recommended. Antibiotic coverage for anaerobic organisms may also be
added to the treatment regimen. NSAIDs or mild oral narcotic analgesics
should be provided as indicated. Dental or oral surgical consultation is
necessary for intramural abscess drainage and endodontic therapy versus
extraction of the involved molar teeth.
Clinical Pearls
1. Ovoid cheek swelling with
sparing of the nasolabial fold helps to identify buccal space abscesses
and differentiates it from canine space abscesses.
2. Odontogenic infections of
the second or third maxillary molars is the most common source for buccal
space abscesses.
|
|
Canine Space Abscess
Associated Clinical Features
The canine space lies between the
anterior surface of the maxilla and levator labii superioris muscle of
the face. The origin of these abscesses can be from upper anterior teeth
and bicuspids, although it is almost exclusively from the maxillary
canine tooth. Erosion of maxillary tooth infection through the alveolar
bone into the canine space leads to abscess formation, although cutaneous
infections from the upper lip and nose are a rare source. Unilateral
facial redness, pain, and swelling lateral to the nose with obliteration
of the nasolabial fold is characteristic (Fig. 6.22). Severe upper lip
and lower eyelid swelling may cause eye closure and drooling at the
corner of the mouth.
|
|
|

|
|
Canine
Space Abscess Unilateral
facial swelling lateral to the nose with associated redness and the
typical loss of the nasolabial fold is shown. The maxillary canine
tooth is usually the source of this process. (Courtesy of Frank
Birinyi, MD.)
|
|
Differential Diagnosis
Buccal space infection, facial
cellulitis, and maxillary sinusitis may present with various clinical
features similar to canine space abscesses. Examination of the anterior
maxillary teeth may provide very helpful clues to the origin and
diagnosis of canine space abscesses. CT scan and sinus x-rays may aid in
defining these lesions.
Emergency Department Treatment
and Disposition
Parenteral antibiotic therapy to
include anaerobic coverage is indicated for treatment. Dental or oral
surgical consultation for intramural incision and drainage represents the
most definitive treatment for canine space abscesses. Extraction or
endodontic treatment of the involved anterior maxillary teeth is usually
necessary.
Clinical Pearls
1. The maxillary canine
(cuspid) teeth are the most common source for canine space abscesses.
2. Although these patients may
drool when significant upper lip swelling is present, they typically do
not have trismus, dysphagia, or odynophagia.
3. Loss of the nasolabial fold
is characteristic of canine space abscesses.
|
|
Ludwig's Angina
Associated Clinical Features
Ludwig's angina is defined as
bilateral cellulitis of the submandibular and sublingual spaces (see Fig.
6.18) with associated tongue elevation (Figs. 6.23 and 6.24). A
characteristic painful, brawny induration is present rather than
fluctuance in the involved tissue. The posterior mandibular molars
represent the usual odontogenic origin for the infection. Streptococcus,
Staphylococcus, and Bacteroides species are the most common
offending pathogens. Affected individuals are usually 20 to 60 years old,
with a male predominance. These patients are usually febrile and may
demonstrate impressive trismus, dysphonia, and odynophagia. Dysphagia and
drooling are secondary to tongue displacement and oropharyngeal swelling.
Potential airway compromise or spread of the infection to the deep
cervical layers and the mediastinum is possible. The presence of dyspnea
or cyanosis is a later, more ominous sign, which indicates impending
airway closure.
|
|
|

|
|
Ludwig's
Angina Note the diffuse
submandibular swelling and fullness. Direct palpation of this area
would reveal a characteristic brawny induration. Potential airway
compromise is a key concern in all patients with Ludwig's angina.
(Courtesy of Jeffrey Finkelstein, MD.)
|
|
|
|
|

|
|
Ludwig's
Angina Note the presence of
subcutaneous gas in the abscessed submandibular area on this
radiograph of a patient with Ludwig's angina. (Courtesy of Edward C.
Jauch, MD, MS.)
|
|
Differential Diagnosis
Peritonsillar abscesses,
epiglottitis, and parapharyngeal and retropharyngeal abscesses all have
clinical features similar in presentation to Ludwig's angina.
Oropharyngeal examination is often uncomfortable and difficult in all the
aforementioned conditions. Caution should be used if epiglottitis is
suspected.
Emergency Department Treatment
and Disposition
Acute laryngospasm with airway
compromise is a potentially life-threatening complication and concern
with Ludwig's angina; therefore, plans for definitive airway management
should be prepared. Up to one-third require intubation or surgical airway
placement. Parenteral antibiotic therapy can be initiated with penicillin
or a third-generation cephalosporin. Coverage for anaerobic organisms
should also be provided with clindamycin or metronidazole. The role of
steroids is controversial and ill defined for potential airway edema in
this setting. Parenteral analgesic should be given as needed. The
definitive treatment is intraoperative surgical drainage of the abscess.
Computed tomography (CT) or magnetic resonance imaging (MRI) can be used
to identify abscess location. Admission to the intensive care unit is
indicated for airway surveillance and management. Oral and maxillofacial
surgical or otolaryngologic consultation is prudent.
Clinical Pearls
1. The second mandibular molar
is the most common site of origin for Ludwig's angina.
2. Admission of these patients
to the intensive care unit is almost always indicated because of the
potential for airway compromise.
3. Intraoperative surgical
incision and drainage is the definitive treatment.
4. Brawny submandibular
induration and tongue elevation are common and characteristic clinical
findings.
5. Acute laryngospasm with
sudden total airway obstruction may be precipitated by attempts at oral
or blind nasal intubation.
|
|
Parapharyngeal Space Abscess
Associated Clinical Features
The parapharyngeal space is also
known as the lateral pharyngeal or pharyngomaxillary space. Anatomically
it is a pyramid-shaped space with its apex at the hyoid bone and base at
the base of the skull. Laterally it is bound by the internal pterygoid
muscle and parotid gland with the superior pharyngeal constrictor muscle
medially. The posterior aspect of this space is in close proximity with
the carotid sheath and cranial nerves IX through XII. Presenting symptoms
include fever, dysphagia, odynophagia, drooling, and ipsilateral otalgia.
Unilateral neck and jaw angle facial swelling, in association with
rigidity and limited neck motion, is common (Fig. 6.25). Potentially
disastrous complications that have been associated with infections of
this space include cranial neuropathies, jugular vein septic
thrombophlebitis, and erosion into the carotid artery. The origin of
parapharyngeal abscesses may be from infected tonsils, sinuses and teeth,
or lymphatic spread.
|
|
|

|
|
Parapharyngeal
Space Abscess Unilateral
facial, jaw angle, and neck swelling is seen in this patient. Nuchal
rigidity may also be present. (Courtesy of Sara-Jo Gahm, MD.)
|
|
Differential Diagnosis
Buccal space abscess, Ludwig's
angina, peritonsillar and retropharyngeal abscesses, and parotitis
represent clinical conditions to consider. A CT scan provides more
specific information and aids in making the diagnosis.
Emergency Department Treatment
and Disposition
Preparations for definitive
airway management via endotracheal intubation or surgery is vital. Early
recognition and anticipation of other potentially disastrous
complications should be considered and managed appropriately.
Broad-spectrum antibiotic coverage for mixed aerobic and anaerobic
infections should be initiated. Radiologic modalities used to assess
parapharyngeal and other deep space neck infections include
contrast-enhanced CT, ultrasound, plain radiography, and MRI.
Otolaryngologic or oral surgical consultation is warranted for definitive
intraoperative incision and drainage of the abscess.
Clinical Pearls
1. Suspected oropharyngeal
abscesses in association with neuropathy in cranial nerves IX through XII
is pathognomonic of parapharyngeal abscesses.
2. Bacterial pharyngitis
represents the most common source of parapharyngeal abscesses.
|
|
Trench Mouth (Acute Necrotizing Ulcerative
Gingivitis)
Associated Clinical Features
Painful, severely edematous interdental
papillae is characteristic of acute necrotizing ulcerative gingivitis
(ANUG). Other associated features include the presence of ulcers with an
overlying grayish pseudomembrane and "punched out" appearance
(Fig. 6.26). The inflamed gingival tissue is very friable, necrotic, and
represents an acute destructive disease process of the periodontium.
Fever, malaise, and regional lymphadenopathy are commonly associated
signs. Patients may also complain of foul breath and a strong metallic
taste. Poor oral hygiene, emotional stress, smoking, and
immunocompromised states (e.g., HIV, steroid use, diabetes) all may
contribute to predisposition for ANUG. Anaerobic Fusobacterium and
spirochetes are the predominate bacterial organisms involved. The
anterior incisor and posterior molar gingival regions are the most
commonly affected oral tissue.
|
|
|

|
|
Acute
Necrotizing Ulcerative Gingivitis
Note the inflamed, friable, and necrotic gingival tissue. An
overlying grayish pseudomembrane or punched out ulcerations of the
interdental papillae are pathognomonic. (Courtesy of David P.
Kretzschmar, DDS, MS.)
|
|
Differential Diagnosis
Acute herpetic gingivostomatitis,
aphthous stomatitis, desquamative gingivitis, gonococcal and
streptococcal gingivostomatitis, and chronic periodontal disease all
represent oral diseases that may mimic ANUG. Differentiating these oral
conditions from one another is based primarily on history and a thorough
oropharyngeal examination.
Emergency Department Treatment
and Disposition
Initial management includes warm
saline irrigation. Systemic analgesics and topical anesthetics such as
viscous lidocaine may facilitate oral hygiene measures. Antibiotic
treatment is initiated immediately with oropharyngeal coverage. Dilute
1.5 to 2% hydrogen peroxide or chlorhexidine oral rinses are also
helpful. Follow-up with a dentist or periodontist in 1 to 2 days is
recommended. Patients with more advanced disease may require admission
and oral surgical consultation.
Clinical Pearls
1. Dramatic relief of symptoms
within 24 h of initiating antibiotics and supportive treatment is
characteristic.
2. Periodontal abscesses and
underlying alveolar bone destruction are common complications of ANUG and
require dental follow-up.
3. There is no evidence that
ANUG is a communicable disease.
4. Gingivitis is a nontender
inflammatory disorder.
5. Consider HIV testing in
patients with ANUG refractory to antibiotic therapy.
|
|
Acid Tooth Erosion (Bulimia)
Associated Clinical Features
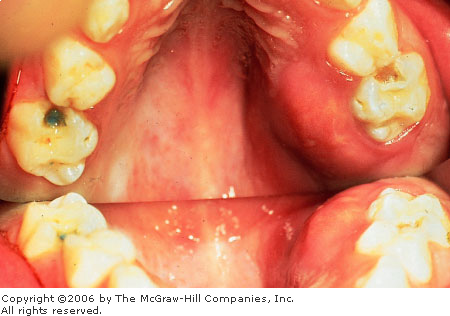
Bulimia nervosa is an eating
disorder—thought to be psychological in origin—with
significant associated physical complications. It is characterized by
binge eating with self-induced vomiting, laxative use, dieting, and
exercise to prevent weight gain. Patients with bulimia are at significant
risk for damage to the dental enamel and dentin as a result of repeated
episodes of vomiting. Chronic exposure to regurgitated acidic gastric
contents represents the main mechanism of injury, which is aggravated by
tongue movement. The lingual dental surfaces are most commonly affected
(Fig. 6.27). In severe cases, all surfaces of the teeth may be affected.
Buccal dental surface erosions may be noted as a result of excessive
consumption of fruit (i.e., lemons) and juices by some bulimic patients.
Trauma to the oral and esophageal mucosa may also result from induced
vomiting. The quantity, buffering capacity, and pH of both the resting
and stimulated saliva are found to be reduced. Salivary gland
enlargement, most commonly the parotid, may occur in bulimic persons as
well. Unexplained elevation of serum amylase, hypokalemia, esophagitis,
menstrual irregularities, and fluctuating weight are other complications
noted with bulimia.
|
|
|

|
|
Acid
Tooth Erosion (Bulimia)
Erosive dentin exposure of the maxillary teeth secondary to chronic
vomiting. The involvement of the lingual dental surfaces is
characteristic of bulimia. (Courtesy of David P. Kretzschmar, DDS,
MS.)
|
|
Differential Diagnosis
Included in the differential
diagnosis of acid tooth erosion are conditions that involve vomiting,
such as pregnancy, stricture or spasm of the esophagus, and disturbances
of gastrointestinal tract peristalsis. Xerostomia is a condition of
excessive mouth dryness (associated with Sjögren's syndrome) and can also
accelerate the process of enamel loss. Conditions resulting in short-term
episodes of vomiting do not have severe destructive effects on the
dentition. Dental abrasions and erosions, singly or in combination, may
result in a considerable loss of tooth structure. Tooth erosions may be
brought about by the use of chewing tobacco (Fig. 6.28), eating betel
nuts, dentifrice, bruxism, abnormal swallowing, and clenching.
|
|
|

|
|
Acid
Tooth Erosion (Snuff User)
Note the typical dentin exposure on the buccal dental surfaces
resulting from prolonged snuff use and its accompanying acid erosion.
(Courtesy of David P. Kretzschmar, DDS, MS.)
|
|
Emergency Department Treatment
and Disposition
Dental treatment should begin
with vigorous oral hygiene to prevent further destruction of tooth
structures. Regular professional fluoride treatments to cover exposed
dentin should be instituted, as well as pain treatment. With the
exception of temporary cosmetic procedures, definitive dental treatment
should be deferred until the patient is adequately stabilized
psychologically. The initial ED management of patients with bulimia
should address any medical complication of the disorder like hypokalemia,
metabolic acidosis, and its associated cardiac, renal, and central
nervous system effects. Hospitalization to stabilize medical
complications and provide nutritional support may be indicated. A
multidisciplinary team approach is necessary and should involve
psychiatry, internal medicine, and dental consultation as needed.
Clinical Pearls
1. The lingual surfaces of the
teeth are the most commonly involved tooth surfaces.
2. Attrition or bruxism tends
to cause enamel loss from occlusal and incisal dental surfaces.
3. The labial and buccal
surfaces of the teeth tend to show enamel loss from repeat or prolonged
chemical contact (e.g., lemon sucking or tobacco products).
|
|
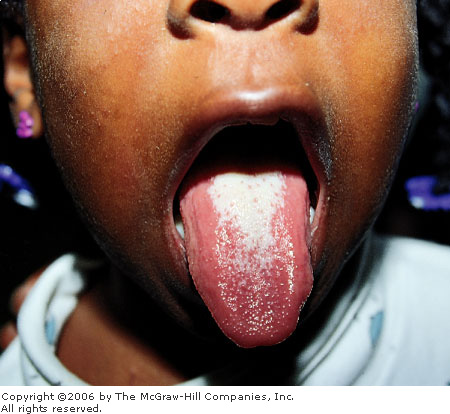
Thrush (Oral Candidiasis)
Associated Clinical Features
White, flaky, curd-like plaques
covering the tongue and buccal mucosa with an erythematous base is
typical of thrush (Fig. 6.29). These lesions tend to be painless;
however, painful inflammatory erosions or ulcers may be noted,
particularly in adults. Decreased oral intake secondary to pain is
common. Colonization of surface epithelium by Candida may be
opportunistic as a result of an altered oral milieu. Predisposing factors
include antibiotic use, corticosteroids, radiation to the head and neck,
extremes of ages, patients with immunologic deficiencies, and chronic
irritation (e.g., denture use and xerostomia).
|
|
|

|
|
Oral
Candidiasis (Thrush) Whitish
plaques are seen here on the buccal mucosa. These plaques are easily
removed with a tongue blade, differentiating them from lichen planus
or leukoplakia. (Courtesy of James F. Steiner, DDS.)
|
|
Differential Diagnosis
Hairy leukoplakia, lingual lichen
planus, flecks of milk or food debris, and liquid antacid adhering to the
tongue may be confused with candidiasis. Hairy leukoplakia cannot be
brushed off with a tongue depressor. This helps differentiate this
process from thrush or residue from ingested materials. Microscopic
examination of the removed specimen for the presence of hyphae in
potassium hydroxide mount will aid in the identification of Candida.
Emergency Department Treatment
and Disposition
Nystatin oral tablets, nystatin
suspension, or clotrimazole oral troches are usually adequate therapy.
Topical analgesic cocktails may also provide comfort for patients (e.g.,
Maalox, diphenhydramine, viscous lidocaine oral rinse).
Clinical Pearls
1. Thrush is most common in
premature infants and immunosuppressed patients.
2. In young adults, thrush may
be the first sign of AIDS; a history of HIV risk factors should be
elicited.
3. Failure of oral candidiasis
to respond to topical antifungal agents may suggest an immune deficiency.
|
|
Oral Herpes Simplex Virus (Cold Sores)
Associated Clinical Features
Oral herpes simplex may present
acutely as a primary gingivostomatitis or as a recurrence. Painful
vesicular eruptions on the oral mucosa, tongue, palate, vermilion borders,
and gingiva are highly characteristic (Figs. 6.30, 6.31). A 2- to 3-day
prodromal period of malaise, fever, and cervical adenopathy is common.
The vesicular lesions rupture to form a tender ulcer with yellow crusting
and an erythematous margin. Pain may be severe enough to cause drooling
and odynophagia, which can discourage eating and drinking, particularly
in children. The disease tends to run its course in a 7- to 10-day period
with resolution of the lesions without scarring. Recurrent herpes labialis
may present with an aura of burning, itching, or tingling prior to
vesicle formation. Oral trauma, sunburn, stress, and any variety of
febrile illnesses can precipitate this condition.
|
|
|

|
|
Herpes
Simplex Virus (HSV) Stomatitis
Note the vermilion border and lingual lesions that are common in this
condition. A prodromal period of fever, malaise, and cervical
adenopathy may herald the onset of these painful ulcerations.
(Courtesy of James F. Steiner, DDS.)
|
|
|
|
|

|
|
HSV
Stomatitis Extensive vesicular
lesions along the vermilion border and surrounding tissues are
consistent with HSV infection. (Courtesy of Frank Birinyi, MD.)
|
|
Differential Diagnosis
Oral erythema multiforme or
Stevens-Johnson syndrome, aphthous lesions, oral pemphigus, and
hand-foot-mouth (HFM) syndrome are in the differential diagnosis. It
should be noted that aphthous ulcers tend to occur on movable oral mucosa
and rarely on immovable mucosa (i.e., hard palate and gingiva). The
vermilion border is a characteristic location for herpes labialis as
opposed to aphthous lesions. Posterior oropharyngeal ulcerations with
associated hand and foot lesions help to define HFM syndrome. Painful
hemorrhagic oral ulcers in association with anorectal and conjunctival
lesions aid in identifying erythema multiforme or Stevens-Johnson
syndrome. Oral pemphigus is commonly found in elderly patients. Cutaneous
skin bullae and several weeks of vague constitutional symptoms are also
characteristic of pemphigus. A thorough history is invaluable in
differentiating the aforementioned disorders.
Emergency Department Treatment
and Disposition
Supportive care with rehydration
and pain control are the mainstays of therapy. Temporary pain relief may
be achieved with topical analgesics. Viscous lidocaine, 2%, may be used
as an oral rinse, 5 mL every 3 to 4 h. Oral antiviral agents may be
useful in adults with primary infections. Topical acyclovir ointment may
also be of use by preventing viral spreading and acting as a lubricant to
prevent lip cracking and bleeding. Secondary infection of herpetic
lesions should be treated with oral penicillin or erythromycin.
Clinical Pearls
1. Oral herpetic lesions tend
to occur on the vermilion border, gingiva, and hard palate.
2. Fatal viremia and systemic
involvement may occur in infants and children with herpetic
gingivostomatitis.
3. Primary acute oral herpetic
infection occurs most commonly in children and young adults.
4. Corticosteroid use is
contraindicated in herpetic gingivostomatitis because of potential
worsening of the condition.
|
|
Aphthous Ulcers (Canker Sores)
Associated Clinical Features
Aphthous ulcers are painful
mucosal lesions varying in size from 1 to 15 mm. A prodromal burning
sensation in the affected area may be noted 2 to 48 h before an ulcer is
noted. The initial lesion is a small white papule that ulcerates and
enlarges over the subsequent 48 to 72 h (Fig. 6.32). The lesions are
typically round or ovoid with a raised yellow border and surrounding
erythema. Multiple aphthous ulcers may occur on the lips, tongue, buccal
mucosa, floor of the mouth, or soft palate (Fig. 6.33). Spontaneous
healing of lesions occurs in 7 to 10 days without scarring. The exact
etiology of aphthous lesions is unknown. Deficiencies of vitamin B12,
folic acid, and iron as well as viruses have been implicated. Stress,
local trauma, and immunocompromised states have all been cited as
possible precipitating factors.
|
|
|

|
|
Aphthous
Ulcer (Single Lesion) Raised
yellow borders with surrounding erythema are typical of aphthous
ulcers. (Courtesy of James F. Steiner, DDS.)
|
|
|
|
|

|
|
Aphthous
Ulcerations Note the multiple
ulcers of various sizes located on the lip and gingival mucosa. These
lesions rarely occur on the immobile oral mucosa of the gingiva or
hard palate. (Courtesy of James F. Steiner, DDS.)
|
|
Differential Diagnosis
Primary or recurrent herpetic
oral lesions may present with an almost identical prodrome and similar
appearance to aphthous ulcerations. Herpetic lesions, unlike aphthous
ones, tend to occur on the gingiva, hard palate, and vermilion border.
Oral erythema multiforme may also present similarly to aphthous
stomatitis; however, like oral herpes, it may tend to present with
multiple vesicles in the early stages. Stevens-Johnson syndrome
represents a severe form of erythema multiforme characterized by
hemorrhagic anogenital and conjunctival lesions as well as oral lesions.
Herpangina results from coxsackie and echoviruses with oral ulcerations
typically involving the posterior pharynx. Oral pemphigus should also be
considered in the differential. Behçet's syndrome can present with
recurrent oral lesions, genital ulcers and uveitis.
Emergency Department Treatment
and Disposition
Supportive care, rehydration, and
pain control constitutes the focus of therapy. A topical anesthetic agent
such as 2% viscous lidocaine as an oral rinse every 3 to 4 h is
palliative. Oral rinses containing antihistamines and liquid antacid
mixtures provide comfort. Use of oral antimicrobial rinses containing 0.12%chlorhexidine
(Peridex) or tetracycline is effective in promoting healing. Protective
dental paste (Orabase) may be applied every 6 h to prevent irritation of
lesions. Triamcinolone acetonide in an emollient dental paste applied
three to four times daily may also reduce pain and promote healing of the
lesions.
Clinical Pearls
1. Aphthous ulcers may be
associated with Crohn's disease.
2. Women are more commonly
affected by aphthous lesions than men.
3. The first aphthous episode
occurs most commonly in the second decade of life.
4. Aphthous lesions almost
never occur on the gums or hard palate.
|
|
Strawberry Tongue
Associated Clinical Features
Reddened, hypertrophied lingual
papillae, called strawberry tongue, is associated primarily with scarlet
fever, which is caused by group A streptococcus. The tongue initially
appears white with the erythematous papillae sticking through the white
exudate. After several days, the white coating is lost and the tongue
appears bright red (Fig. 6.34). Other signs of group A streptococcal
infection include fever, an exudative pharyngitis, a scarlatiniform rash,
and the presence of Pastia's lines (petechial linear rash in the skin
folds (see Fig. 14.30)).
|
|
|
|
|
Strawberry
Tongue Note the white exudate
with bulging red papillae. The white coating is eventually lost after
several days, and the tongue then appears bright red. (Courtesy of
Michael J. Nowicki, MD.)
|
|
Differential Diagnosis
Kawasaki syndrome may also
present with an injected pharynx and an erythematous strawberry-like
tongue. It is essential to make the distinction between streptococcal
infection and Kawasaki syndrome, since the latter is associated with a
high incidence of coronary artery aneurysm if left untreated. Also
consider toxic shock syndrome (TSS), in which one-half to three-fourths
of patients tend to have pharyngitis with a strawberry-red tongue.
Patients with TSS also have skin rashes, as with scarlet fever; however,
the rash in TSS is macular and "sunburn-like." Erythema
multiforme can also be associated with fever, pharyngeal erythema, and
lingual lesions; however, it has a more distinct pathognomonic cutaneous
rash (called target or iris lesions).
Emergency Department Treatment
and Disposition
Penicillin or a macrolide is the
drug of choice for group A streptococci. Pharyngeal cultures are useful
for confirming the diagnosis. Antistreptolysin O (ASO) titers can be used
for confirmation in the convalescent stage if the diagnosis is in
question. Rapid streptococcal immunoassay testing may help expedite the
diagnosis.
Clinical Pearls
1. A coarse, palpable,
sandpaper-like rash of the skin is highly characteristic of scarlet
fever.
2. Strawberry tongue initially
appears white in color, with prominent red papillae bulging through the
white exudate. After several days, the tongue becomes completely beefy
red.
3. Erythrogenic toxin
elaborated by the streptococcal organism is responsible for producing the
exanthem and enanthem of scarlet fever.
|
|
Torus Palatinus
Associated Clinical Features
Tori are benign nodular
overgrowths of the cortical bone. Although their physical appearance can
be somewhat alarming to those unfamiliar with this entity, there is
generally no need for concern. These bony protuberances occur in the
midline of the palate where the maxilla fuses (Fig. 6.35). Tori may also
be located on the mandible, typically on the lingual aspect of the molar
teeth. Tori are covered by a thin epithelium, which is easily traumatized
and ulcerated. These ulcerations tend to heal very slowly because of the
poor vascularization of the tori. Torus palatinus, in particular, is
slow-growing and may occur at any age; however, it is most commonly noted
prior to age 30 in adults. Torus palatinus affects women twice as
frequently as men.
|
|
|

|
|
Torus
Palatinus Note the nodular
appearance and characteristic central palatal location. Abrasions and
ulcerations can occur on the thin overlying epithelium secondary to
trauma by food and oral objects. (Courtesy of Kevin J. Knoop, MD,
MS.)
|
|
Differential Diagnosis
There are a variety of oral
conditions that may be confused with mandibular or palatal tori. Gingival
fibromatosis, fibroma formation secondary to irritation, granulomas,
abscesses, and oral neurofibromatosis located on the palate may all be
similar in appearance to torus palatinus. Nodular bony enlargement in the
oral cavity may also result from fibrous dysplasia, osteomas, and Paget's
disease. Oral malignancies may also manifest themselves on the palate as
primary lesions. Biopsies, oral radiographs, and CT scans may aid in
differentiating these conditions.
Emergency Department Treatment
and Disposition
Tori are normal structural
variants and do not represent any inflammatory or neoplastic process.
Therefore, they are of no clinical significance and require no treatment
unless associated with a complication. Tori may enlarge enough to
interfere with eating or speaking and impair proper fitting of dental
prosthesis. For some patients the mere presence of torus palatinus may be
bothersome and undesirable. Oral and maxillofacial consultation is
indicated for suspected malignancies or lesions of questionable origin.
Clinical Pearls
1. Torus palatinus almost
always occurs in the midline of the hard palate.
2. Both torus palatinus and
torus mandibularis are nontender and otherwise asymptomatic.
|
|
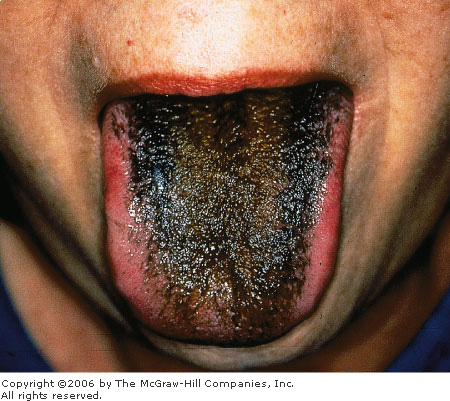
Black Hairy Tongue
Associated Clinical Features
Black hairy tongue represents a
benign reactive process characterized by hyperplasia and dark
pigmentation of the tongue's filiform papillae (Fig. 6.36). The elongated
filiform papillae may reach up to 2 cm in length and vary in actual
degree of pigmentation from light tan to black. Predisposing factors may
include excessive smoking, poor oral hygiene, and the use of
broad-spectrum oral antibiotics. Pigment from consumed food, beverages,
and tobacco products stains the entrapped food debris and desquamated
papillary keratin. Some antibiotics may alter normal oral microflora and
promote the growth of chromogenic organisms, also contributing to the
tongue's discoloration. The darkly pigmented filament-like papillae give
the tongue a black, hairy appearance. Males are more often affected than
females; this condition very rarely occurs in children. Alteration of
taste perception and halitosis may be a consequence of this disorder.
|
|
|
|
|
Black
Hairy Tongue Hyperplasia of
the filiform papillae on the dorsum of the tongue accompanied by deposition
of dark pigment is characteristic of black hairy tongue. (Courtesy of
the Department of Dermatology, National Naval Medical Center,
Bethesda, MD.)
|
|
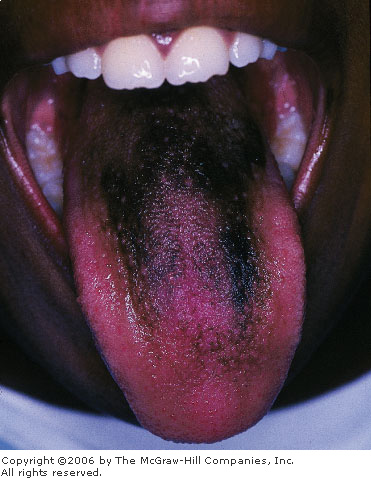
Differential Diagnosis
Geographic tongue and orolingual
candidiasis may resemble more lightly pigmented forms of black hairy
tongue (BHT). Similarly, dark discoloration of normal tongue papillae may
also mimic BHT clinically. This exogenous pigmentation of normal papillae
may come from ingested food dyes and certain medications, such as
bismuth-containing compounds (Fig. 6.37), ketoconazole, and
azidothymidine. The lack of hyperplastic filiform papillae with
additional pigmentation of other oral mucosal surfaces may aid in
distinguishing these conditions.
|
|
|
|
|
Black
Tongue Deposition of black
pigment secondary to bismuth ingestion. This patient ingested
Pepto-Bismol. (Courtesy of Kevin J. Knoop, MD, MS.)
|
|
Emergency Department Treatment
and Disposition
Improved oral hygiene with gentle
tongue brushing and a reduction in the ingestion of exogenous
pigment-containing substance represent the cornerstone of treatment.
Removal of other predisposing factors (e.g., antibiotic withdrawal and
smoking cessation) will also promote resolution of this condition. The
use of topically applied retinoid preparations and antifungal agents has
been advocated for more refractory instances.
Clinical Pearls
1. BHT always involves the
dorsal aspect of the tongue anterior to the circumvallate papillae.
2. This is a benign condition
and is rarely symptomatic.
3. The tongue is not always
black and can be as light as a tan or yellow color.
|
|
Acknowledgments
The authors acknowledge Sara-Jo
Gahm, MD, for portions of this chapter written for the first edition of
this book.
|
|