|
Note: Large images and
tables on this page may necessitate printing in landscape mode.
Copyright
©2006 The McGraw-Hill Companies. All rights reserved.
Emergency
Medicine Atlas > Part 1. Regional
Anatomy > Chapter 7. Chest and Abdomen > Chest
and Abdominal Trauma >
|
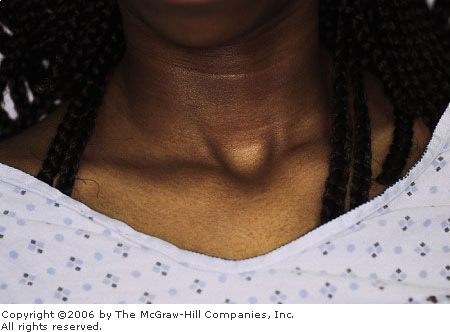
Traumatic Asphyxia
Associated Clinical Features
Traumatic asphyxia is due to a
sudden increase in intrathoracic pressure against a closed glottis. The
elevated pressure is transmitted to the veins, venules, and capillaries
of the head, neck, extremities, and upper torso, resulting in capillary
rupture. Survivors demonstrate plethora, ecchymoses, petechiae (Figs. 7.1
and 7.2), and subconjunctival hemorrhages. Severe cases may produce CNS
injury with seizures, posturing, and paraplegia.
|
|
|

|
|
Traumatic
Asphyxia This 45-year-old male
was pinned when the truck he was working under fell on his chest. He
was unable to breathe for 3 to 4 min until his coworkers rescued him.
The violaceous coloration of the shoulders, face, and upper chest is
apparent. (Courtesy of Stephen Corbett, MD.)
|
|
|
|
|

|
|
Traumatic
Asphyxia A closer view showing
the petechial nature of this rash. The patient was observed in the
hospital overnight and recovered completely. (Courtesy of Stephen
Corbett, MD.)
|
|
Differential Diagnosis
Sudden traumatic compression of
the superior vena cava produces obstruction similar to that seen in the
superior vena cava syndrome. Both demonstrate a violaceous discoloration
of the face and neck. History will confirm the diagnosis.
Emergency Department Treatment
and Disposition
Treatment is supportive, with
attention to other concurrent injuries. Long-term morbidity is related to
the associated injuries.
Clinical Pearls
1. Facial petechiae are known
as Tardieu's spots.
2. Be alert for associated rib
and vertebral fractures.
|
|
Tension Pneumothorax with Needle Thoracentesis
Associated Clinical Features
A tension pneumothorax results
when air is able to enter but not exit the pleural space. Air in the
pleural space accumulates and compresses the ipsilateral lung and vena
cava, with a rapid decrease in cardiac output. The contralateral lung may
suffer ventilation/perfusion ( / / )
mismatch. Subcutaneous air, tracheal deviation, jugulovenous distention
(JVD), and diminished or hyperresonant ipsilateral breath sounds can be
clues. Subcutaneous emphysema may be visible on the neck and chest and is
easily diagnosed by palpation. The released air from a tension
pneumothorax can be heard escaping from a needle thoracostomy. )
mismatch. Subcutaneous air, tracheal deviation, jugulovenous distention
(JVD), and diminished or hyperresonant ipsilateral breath sounds can be
clues. Subcutaneous emphysema may be visible on the neck and chest and is
easily diagnosed by palpation. The released air from a tension
pneumothorax can be heard escaping from a needle thoracostomy.
Differential Diagnosis
Cardiac tamponade, congestive
heart failure with pulmonary edema, esophageal intubation, and
anaphylaxis should be considered.
Emergency Department Treatment
and Disposition
Treatment requires rapid recognition
of the tension pneumothorax, frequently without benefit of chest
radiographs. A large-bore needle (at least 14 gauge) should be placed
over the superior rib surface of the second interspace in the
midclavicular line (Fig. 7.3). A rush of air with improvement of vital
signs confirms the diagnosis. A syringe loaded with sterile saline allows
visualization of air return but is not mandatory. If there is no
immediate improvement, do not hesitate to place a second needle in the
next interspace. A chest tube should be placed as soon as possible.
Ventilation with appropriate inspiratory/expiratory ratio would prevent
further occurrences.
|
|
|

|
|
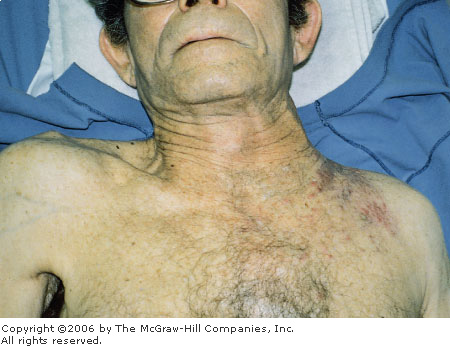
Tension
Pneumothorax A 35-year-old
male with severe asthma suffered respiratory arrest during transport
by ambulance. He was intubated on arrival but soon became hard to
ventilate and developed subcutaneous emphysema followed by hypotension.
Needle thoracostomy produced a rush of air and bubbling from the
needle with stabilization of vital signs. (Courtesy of Stephen
Corbett, MD.)
|
|
Clinical Pearls
1. Do not overventilate
patients with obstructive pulmonary disease. "Stacking" breaths
trap air in the lungs and predispose to bleb rupture and pneumothorax.
The pathophysiology of this disease requires a prolonged expiratory
phase.
2. The diagnosis of a tension
pneumothorax is made clinically and should be treated immediately with a
needle thoracostomy and ultimately a tube thoracostomy.
|
|
Cardiac Tamponade with Pericardiocentesis
Associated Clinical Features
Beck's triad of acute cardiac
tamponade includes jugulovenous distention (JVD) from an elevated central
venous pressure (CVP), hypotension, and muffled heart sounds. In trauma,
only one-third of patients with cardiac tamponade demonstrate this
classic triad, although 90% have at least one of the signs. The
simultaneous appearance of all three physical signs is a late
manifestation of tamponade and usually seen just prior to cardiac arrest.
Other symptoms include shortness of breath, orthopnea, dyspnea on
exertion, syncope, and symptoms of inadequate perfusion.
Differential Diagnosis
Patients with a chronic
pericardial effusion have an elevated CVP and a small, quiet heart but
are relatively asymptomatic and without hypotension.
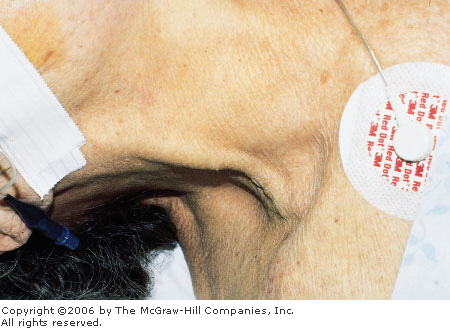
Emergency Department Treatment
and Disposition
The clinical diagnosis of
tamponade requires suspicion and a careful evaluation of the signs and,
when available, imaging techniques. Two-dimensional echocardiography
represents the ultimate standard for diagnosis. ED pericardiocentesis
(Fig. 7.4) is a diagnostic and resuscitative procedure in patients with
suspected cardiac tamponade. Goals of ED pericardiocentesis include
identification of pericardial effusion and removal of blood from the
pericardial space to relieve the tamponade.
|
|
|

|
|
ED
Pericardiocentesis A positive
pericardiocentesis in a patient with a sudden onset of shortness of
breath and electrical alternans. (Courtesy of Lawrence B. Stack, MD.)
|
|
Clinical Pearls
1. An electrical alternans seen
on a 12-lead ECG suggests pericardial effusion.
2. Beck's triad for acute
cardiac tamponade is a late manifestation and is seen in only 30% of
trauma patients.
|
|
Emergency Department Thoracotomy
Associated Clinical Features
ED thoracotomy is a resuscitative
procedure performed in patients with penetrating chest trauma who have
lost signs of life in the presence of prehospital or ED personnel.
Resuscitative thoracotomy (Fig. 7.5) in the ED has specific goals once
the chest is opened: relief of cardiac tamponade, support of cardiac function
(internal cardiac compressions, cross-clamping the aorta to improve
coronary perfusion, and internal defibrillation), and control of
hemorrhage from the heart, pulmonary vessels, thoracic wall, and great
vessels.
|
|
|
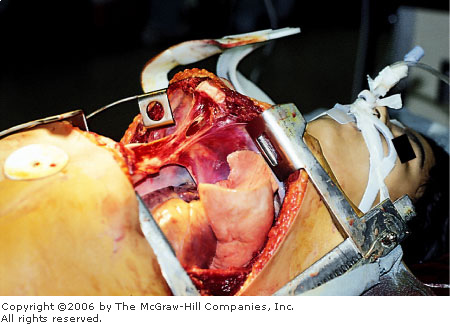
|
|
ED
Thoracotomy An unsuccessful
resuscitative ED thoracotomy with pericardiotomy in a patient with
penetrating chest trauma who lost signs of life in the field after
the paramedics arrived at the scene. (Courtesy of Alan B. Storrow,
MD.)
|
|
Differential Diagnosis
Few conditions present that
require immediate ED thoracotomy. A trauma patient who has lost vital
signs prior to arrival of prehospital personnel is deceased and not a
candidate for this procedure.
Emergency Department Treatment
and Disposition
Patients with penetrating
thoracic trauma who lose their vital signs en route to the ED should
receive an immediate thoracotomy on arrival by the most experienced
provider. Patients with penetrating thoracic trauma whose blood pressure
cannot be maintained above 70 mmHg with aggressive fluid and blood
management should be considered for ED thoracotomy. Patients with blunt
trauma who lose their vital signs en route to the ED should not undergo
an ED thoracotomy, since they rarely survive. Surgical support should be
notified as soon as possible.
Clinical Pearls
1. Injuries potentially
responsive to resuscitative ED thoracotomy include cardiac tamponade,
pulmonary parenchymal and tracheobronchial injuries, large-vessel
injuries, air embolism, and penetrating heart injuries.
2. Resuscitative ED thoracotomy
should be performed immediately once the indications have been met, since
the likelihood of survival is greater when this is performed earlier in
the resuscitation.
|
|
Diagnostic Peritoneal Lavage (DPL)
Associated Clinical Features
Diagnostic peritoneal lavage
(DPL) was introduced in 1965 as a simple, fast, and reliable technique to
identify hemoperitoneum in patients with blunt and penetrating abdominal
trauma. It is performed by placing a catheter into the peritoneum,
aspirating for gross blood, and introducing 1 L of crystalloid if the
initial aspiration is negative (Fig. 7.6). The lavage fluid is then withdrawn
and white and red cell blood counts are obtained. Interpretation of the
results is based on the type of trauma. A "grossly positive"
DPL is evident when 10 mL of blood is obtained on the initial aspiration.
The procedure is considered positive in blunt abdominal trauma when
>100,000 RBC/mm3 or >500 WBC/mm3 are present
in the lavage fluid. In penetrating abdominal trauma, the procedure is
considered positive when >10,000 RBC/mm3 are present (up to
100,000 RBC/mm3 is used by some). Lavage fluid containing
intestinal contents is evidence of perforating bowel injury.
|
|
|
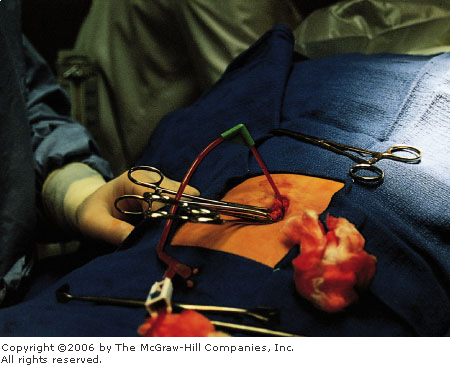
|
|
Positive
DPL DPL fluid obtained from
this patient with blunt trauma was microscopically positive. Initial
aspiration was negative. (Courtesy of Kevin J. Knoop, MD, MS.)
|
|
Indications for DPL in blunt
trauma include equivocal examination with significant abdominal trauma,
unreliable examination (intoxication, spinal trauma, head injury),
unexplained hypotension with suspected abdominal injury, and when serial
examinations are not possible (in patients going to the operating room
for other injuries).
Indications for DPL in
penetrating trauma include patients in whom the need for celiotomy is
unclear, tangential wounds in which peritoneal penetration is uncertain,
stab wounds in which there are no peritoneal signs or signs of peritoneal
penetration, and low chest wounds to identify diaphragmatic injury.
Contraindications to DPL include
any condition in which a celiotomy is clearly indicated, since this would
delay definitive treatment.
Differential Diagnosis
Injuries that may not be
diagnosed with DPL include subcapsular liver or spleen hematomas, injury
to a hollow viscus, ruptured diaphragm, and ruptured bladder.
Retroperitoneal injuries (pancreatic, duodenal) are not diagnosed with
DPL.
Emergency Department Treatment
and Disposition
A positive DPL is an indication
for celiotomy. Patients with negative DPLs are observed or discharged
based on a variety of factors including injury mechanism, comorbid
disease states, and concurrent traumatic injuries.
Clinical Pearls
1. Intraperitoneal blood (30
mL) will typically give a DPL result of  100,000
RBC/mm3. 100,000
RBC/mm3.
2. Controversy exists over the
positive cell count in penetrating abdominal trauma, since the range for
a positive result can vary between centers from 1000 to 100,000 RBC/mm3.
3. If transfer is indicated, a
sample of DPL fluid should accompany the patient.
|
|
Seat Belt Injury
Associated Clinical Features
Seat belts have reduced mortality
and the severity of trauma due to motor vehicle accidents; however, they occasionally
produce injury. Injuries caused by the standard three-point restraint
harness (Fig. 7.7) are most commonly rib fractures. Injuries caused by
the older lap belts include abdominal injuries such as bowel contusion or
perforation and lumbar fractures.
|
|
|

|
|
Seat
Belt Injury Ecchymosis from
the three-point seat belt is clearly seen. The injuries identified
are multiple rib fractures and multiple hematomas of the small bowel
wall. (Courtesy of Stephen Corbett, MD.)
|
|
Differential Diagnosis
A careful primary and secondary
survey identifies most injuries caused by seat belt use. Difficult
diagnosis occurs in the case of bowel perforation or diaphragmatic
rupture, in which signs and symptoms may not occur until hours or days
after the initial injury.
Emergency Department Treatment
and Disposition
Patients with a mechanism for
significant trauma or with other injuries requiring admission should be
admitted for observation or definitive treatment. Patients discharged
home from the ED should be given appropriate precautions to monitor for a
delayed injury presentation.
Clinical Pearls
1. Maintain a high suspicion
for intraabdominal injury when ecchymosis from a seat belt is seen in a
trauma victim.
2. When lap belt bruises are
present, there is a higher incidence of bowel injury.
|
|
Grey-Turner's Sign and Cullen's Sign
Associated Clinical Features
Bluish to purplish periumbilical
discoloration (Cullen's sign) and left flank discoloration (Grey-Turner's
sign) represent retroperitoneal hemorrhage that has dissected through
fascial planes to the skin (Fig. 7.8). Retroperitoneal blood may also
extravasate into the perineum, causing a scrotal hematoma or inguinal
mass. This hemorrhage may represent a hemodynamically significant bleed.
|
|
|

|
|
Grey-Turner's
and Cullen's Signs This
patient displays both flank and periumbilical ecchymoses
characteristic of Grey-Turner's and Cullen's signs. (Courtesy of
Michael Ritter, MD.)
|
|
Differential Diagnosis
Cullen's sign and Grey-Turner's
sign are most frequently associated with hemorrhagic pancreatitis (seen
in 1 to 2% of cases), and typically are seen 2 to 3 days after onset of
acute pancreatitis. These signs may also be seen in ruptured ectopic
pregnancy, severe trauma, leaking or ruptured abdominal aortic aneurysm,
coagulopathy, or any other condition associated with bleeding into the
retroperitoneum.
Emergency Department Treatment
and Disposition
Treatment of patients with
Grey-Turner's sign or Cullen's sign depends on the etiology of the
hemorrhage. Because the hemorrhage may represent a hemodynamically
significant bleed, cardiovascular stabilization after airway
stabilization is of the utmost importance. Once the patient has been
stabilized, the source of bleeding can be elicited by selected laboratory
[complete blood cell count (CBC), amylase, lipase, human chorionic
gonadotropin (HCG)] and diagnostic studies [ultrasound, computed
tomography (CT)]. Because of the severity of diseases associated with
Grey-Turner's and Cullen's signs, these patients are usually admitted to
the hospital.
Clinical Pearls
1. Grey-Turner's sign (flank
discoloration) and Cullen's sign (periumbilical discoloration) are due to
retroperitoneal bleeding that has dissected through fascial planes.
2. These signs are typically
seen 2 to 3 days after the acute event.
3. These signs are seen in only
1 to 2% of patients with hemorrhagic pancreatitis.
|
|
Impaled Foreign Body
Associated Clinical Features
Stab wounds cause injury to
tissue in their path. Stab wounds to the chest, in addition to causing
pneumo- or hemothorax, may also cause life-threatening injuries to the
heart and major blood vessels (Fig. 7.9). One-third of stab wounds to the
abdomen (Fig. 7.10) penetrate the peritoneal cavity. Half of those
injuries that penetrate the peritoneum require surgical intervention. The
path of the stab wound is difficult to determine if the inflicting object
has been removed. The size of the external wound frequently
underestimates the internal injury. Impaled foreign bodies to the chest
or abdomen pose a complex problem. The object inflicting the injury may
also be preventing significant blood loss and therefore should be removed
by the trauma surgeon in the operating room.
|
|
|

|
|
Impaled
Chest Wound This patient was
stabbed in the chest with a butcher knife in a family dispute. The
knife was stabilized by EMS providers at the scene and removed in the
operating room. Injury was isolated to the right atrium. (Courtesy of
Kevin J. Knoop, MD, MS.)
|
|
|
|
|

|
|
Impaled
Abdominal Foreign Body Impaled
knife to the left abdomen. (Courtesy of Ian Jones, MD.)
|
|
Differential Diagnosis
Determining whether the impaled
object has violated the peritoneum or if injury to a significant
structure has occurred can be determined by local wound exploration or
diagnostic peritoneal lavage (DPL), depending on the stability of the
patient and location of the wound (see Fig. 7.13).
Emergency Department Treatment
and Disposition
Initial stabilization of the
patient (intravenous fluid resuscitation, oxygen, monitoring), obtaining
appropriate laboratory studies including blood type and cross-matching,
and resource mobilization (trauma team) are important steps in the
initial management of penetrating chest or abdominal trauma. Prior to
surgical evaluation, stabilization of the impaled foreign object should
be performed to prevent further injury.
Clinical Pearl
1. Impaled chest or abdominal
foreign bodies should be removed only by the trauma surgeon in a
controlled setting.
|
|
Abdominal Evisceration
Associated Clinical Features
Evisceration of abdominal
contents (Fig. 7.11) usually occurs after a stab or slash wound to the
abdomen (Fig. 7.12). It is an indication for celiotomy (laparotomy).
Other indications for celiotomy in penetrating abdominal trauma include
peritoneal injury; unexplained shock; evidence of blood in the stomach,
bladder, or rectum; and loss of bowel sounds.
|
|
|

|
|
Abdominal
Evisceration Self-induced
evisceration with bowel perforation and spillage of food particles is
clearly seen in this photograph. This patient went directly to the
operating room. (Courtesy of Lawrence B. Stack, MD.)
|
|
|
|
|

|
|
Abdominal
Evisceration Evisceration of
small bowel after assault and stab wound to the right lower abdomen.
(Courtesy of Frank Birinyi, MD.)
|
|
Differential Diagnosis
Superficial laceration without
peritoneal penetration, laceration with peritoneal penetration but no
visceral injury, and laceration with peritoneal penetration and visceral
injury may present with a similar mechanism and need to be
differentiated. Consideration of the anatomic boundaries of the abdomen
(Fig. 7.13) is important in differentiating abdominal injuries from
penetrating chest or retroperitoneal injuries.
|
|
|
|
|
Anatomic
Boundaries of the Abdomen Anterior
abdomen: Anterior costal
margins superiorly, laterally by the anterior axillary lines, and
inferiorly by the inguinal ligaments.
Low
chest: Nipple line (fourth
intercostal space) anteriorly and inferior scapular tip (seventh
intercostal space) to inferior costal margins.
Flank: (Shaded blue) Anterior axillary line
anteriorly, posteriorly by the posterior axillary line, inferiorly by
the iliac crest, and superiorly by the inferior scapular tip. The
back is bounded laterally by the posterior axillary lines.
Back: Inferior scapular tip to iliac crest and
posterior axillary lines.
|
|
Emergency Department Treatment
and Disposition
Initial stabilization
(intravenous fluid resuscitation, oxygen, and monitoring), obtaining
appropriate laboratory studies including a blood type and cross-matching,
and resource mobilization (notifying surgical team, operating room, and
anesthesiology) are important steps in the initial management of
penetrating abdominal trauma. In most cases, definitive treatment is
celiotomy.
Clinical Pearls
1. Indications for celiotomy
after penetrating wounds to the abdomen include evisceration; peritoneal
signs; unexplained hypotension; blood in the stomach, bladder, or rectum;
and loss of bowel sounds.
2. Selected patients with stab
wounds to the abdomen and peritoneal penetration may be conservatively
observed for delayed complications.
3. As many as 20% of patients
with stab wounds to the abdomen can be discharged from the ED based on a
negative wound exploration.
|
|
Traumatic Abdominal Hernia
Associated Clinical Features
Blunt traumatic abdominal hernia
is defined as herniation through disrupted musculature and fascia
associated with adequate trauma, without skin penetration, and no
evidence of a prior hernial defect at the site of injury (Fig. 7.14).
This occurs when a considerable blunt force is distributed over a surface
area large enough to prevent skin penetration but small enough to cause a
focal defect in the underlying fascia or muscle wall. Most of these
injuries are due to seat belt injures in motor vehicle crashes; handlebar
injuries are the second most common cause.
|
|
|

|
|

|
|
Traumatic
Abdominal Wall Hernia This
5-year-old boy suffered a traumatic hernia from a handlebar injury.
(Courtesy of Lawrence B. Stack, MD.)
|
|
Differential Diagnosis
Existing hernia, abdominal wall
hematoma, and abdominal wall contusion should be considered in evaluating
a patient with focal blunt trauma to the abdomen and possible hernia.
Abdominal computed tomography (CT) with contrast is the diagnostic
procedure of choice in the evaluation of abdominal trauma (Fig. 7.15).
Ultrasound may play a limited role in the diagnosis of abdominal wall
hernia.
|
|
|

|
|
CT
Scan, Abdominal Wall Hernia
Abdominal contents are seen extruding through a fascial defect.
(Courtesy of Lawrence B. Stack, MD.)
|
|
Emergency Department Treatment
and Disposition
Identification and treatment of
life-threatening associated injuries takes priority over the hernia. The
hernial defect should be repaired after the patient has been stabilized.
Clinical Pearls
1. Abdominal hernia due to
blunt trauma is a rare injury, most frequently due to seat belt injuries
in motor vehicle crashes.
2. CT scan is the diagnostic
procedure of choice for abdominal wall hernia.
|
|
Respiratory Retractions
Associated Clinical Features
Increased respiratory effort may
be manifest by increased respiratory rate, increased chest wall
excursion, and retractions of the less rigid structures of the thorax.
Retractions of the sternum (Fig. 7.16), suprasternal notch (Fig. 7.17),
and intercostal retractions reflect increased respiratory effort. This
may be due to obstructive disease such as asthma or tracheal obstruction,
pneumonia, or restrictive disease. The presence of stridor, wheezing, or
rhonchi will help distinguish the cause.
|
|
|

|
|
Sternal
Retractions Sternal
retractions in a patient with croup. (Courtesy of Stephen Corbett,
MD.)
|
|
|
|
|
|
|
|
|
Suprasternal
Retractions Suprasternal
retractions in an adolescent with severe asthma. (Courtesy of Kevin
J. Knoop, MD, MS.)
|
|
Differential Diagnosis
Asthma, chronic obstructive
pulmonary disease, emphysema, epiglottitis, croup, foreign-body
aspiration, esophageal foreign body, bacterial tracheitis, posterior
pharyngeal abscess, and anaphylaxis are all conditions that must be
considered in a patient with retractions.
Emergency Department Treatment
and Disposition
An aggressive search for the
cause of the retractions is required to direct therapy. Rapid evaluation
of the airway for patency and breathing for oxygenation should be done
immediately on presentation. High-flow oxygen by face mask is appropriate
for patients in respiratory distress. Preparations for securing an airway
should be underway for those patients in severe distress or respiratory
failure. Routine measures for the mildly symptomatic patient depend on
the cause of the retractions. For asthma or exacerbations of chronic
obstructive pulmonary disease (COPD), nebulized  2
agonists and steroid therapy may be appropriate. Patients with croup may
require nebulized normal saline and possibly epinephrine or dexamethasone
as initial therapy. Foreign-body aspiration requires consultation for
confirmation of the suspected diagnosis and removal. 2
agonists and steroid therapy may be appropriate. Patients with croup may
require nebulized normal saline and possibly epinephrine or dexamethasone
as initial therapy. Foreign-body aspiration requires consultation for
confirmation of the suspected diagnosis and removal.
Clinical Pearls
1. Retractions are best
observed with the patient at rest with the chest exposed.
2. Retractions from obstructive
airway disease can be intercostal and supraclavicular and are usually
accompanied by nasal flaring, increased expiratory phase, and increased
respiratory rate.
|
|
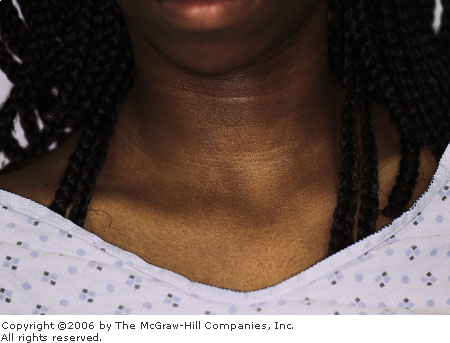
Superior Vena Cava Syndrome
Associated Clinical Features
This symptom complex develops
from obstruction of venous drainage from the upper body, resulting in
increased venous pressure, which leads to dilation of the collateral
circulation. Superior vena cava (SVC) syndrome is most commonly caused by
malignant mediastinal tumors. Dyspnea; swelling of the face, upper
extremities, and trunk; chest pain, cough, or headache may be present.
Physical findings include dilation of collateral veins of the trunk and
upper extremities, facial edema and erythema (plethora), cyanosis, and
tachypnea (Fig. 7.18).
|
|
|

|
|
Superior
Vena Cava Syndrome A
27-year-old man with SVC syndrome. Note the prominent collateral
veins of the chest and neck. (Courtesy of William K. Mallon, MD.)
|
|
Differential Diagnosis
Malignancy, pericarditis,
pericardial tamponade, tuberculosis, and congestive heart failure should
be considered.
Emergency Department Treatment
and Disposition
Radiation therapy is the
treatment of choice for most malignant mediastinal tumors causing SVC
syndrome. Administration of corticosteroids and diuretics initiated in
the ED may provide temporary relief pending definitive therapy.
Clinical Pearls
1. SVC syndrome is most
commonly caused by malignant mediastinal tumors.
2. Treatment of most
mediastinal tumors causing SVC syndrome is radiation therapy.
3. CT scan of the chest is the
diagnostic modality of choice for patients with SVC syndrome.
|
|
Apical Lung Mass
Associated Clinical Features
Pancoast's tumor involves the
apical lung and may affect contiguous structures such as the brachial
plexus, sympathetic ganglion, vertebrae, ribs, superior vena cava, and
recurrent laryngeal nerve (more common for left-sided tumors). Horner's
syndrome, extremity edema, nerve deficits, hoarseness, and superior vena
cava syndrome may result. Erosion of tumor through the chest wall can
cause compression of venous outflow, with resultant jugulovenous
distention (JVD) (Fig. 7.19).
|
|
|
|
|
Apical
Lung Mass This 68-year-old
male cigarette smoker complained of cough and weight loss. A chest
radiograph shows a left apical tumor. There is erosion of the tumor
into the chest wall, with an indurated supraclavicular and
infraclavicular mass. Moderate JVD is apparent, suggesting venous
outflow obstruction. (Courtesy of Stephen Corbett, MD.)
|
|
Differential Diagnosis
Virchow's node of abdominal
carcinoma, lymphoma, vascular abnormalities, and tuberculosis should be
considered.
Emergency Department Treatment
and Disposition
Treatment depends on the staging
and type of tumor. The superior vena cava syndrome can be treated acutely
with radiation and diuretics. Thrombolytic therapy has been used
successfully in some cases of acute vena caval thrombosis.
Clinical Pearls
1. Thrombosis may cause acute
decompensation with edema, plethora, and airway collapse.
2. Prompt radiation therapy can
be lifesaving in cases of vena caval obstruction.
|
|
Jugulovenous Distention
Associated Clinical Features
Central venous (right atrial)
pressure is reflected by distention of the internal or external jugular
veins. Normal pressure is less than 3 cm of distention above the sternal
angle of Louis. Distention greater than 4 cm should be considered
abnormal. Evaluation begins by raising the head of the supine patient 30
to 60 degrees. The highest point of venous pulsation at the end of normal
expiration is measured from the sternal angle of Louis. The presence of
jugulovenous distention (JVD) (Fig. 7.20) should prompt an immediate
search for possible pulmonary or cardiac pathology. The presence of
crackles, murmurs, rubs, percussed hyperresonance, or crepitus may help
disclose the etiology.
|
|
|
|
|
Jugulovenous
Distention An engorged
external jugular vein is noted as it crosses the sternocleidomastoid
muscle into the posterior triangle of the neck and disappears beneath
the clavicle to join the brachiocephalic vein and the superior vena
cava. This patient has severe congestive heart failure requiring
intubation. (Courtesy of Stephen Corbett, MD.)
|
|
Differential Diagnosis
Causes of JVD include right
ventricular failure, left ventricular failure, biventricular failure,
parenchymal lung disease, pulmonary hypertension, pulmonic stenosis,
restrictive pericarditis, superior vena cava syndrome, pulmonary embolus,
tricuspid valve outflow obstruction, tension pneumothorax, increased
circulating blood volume, and atrial myxoma. Temporary venous engorgement
may result from Valsalva maneuver, positive pressure ventilation, and
Trendelenburg position.
Emergency Department Treatment
and Disposition
Treatment varies depending on the
cause. Preload reduction may help in cases of congestive heart disease.
Reversal of a traumatic etiology with needle thoracostomy or
pericardiocentesis may be required.
Clinical Pearls
1. Right-sided myocardial
infarction may produce JVD with clear lung fields.
2. JVD may be absent in the
presence of the above-listed causes if hypovolemia is present.
|
|
Caput Medusae
Associated Clinical Features
Veins of the abdomen normally are
scarcely visible within the abdominal wall. Engorged veins, however, are
often visible through the normal abdominal wall. Engorged veins forming a
knot in the area of the umbilicus are described as a caput medusae (Fig.
7.21). The extent of associated findings depends on the underlying
etiology. It is usually secondary to liver cirrhosis, with subsequent
portal hypertension and development of circulation circumventing the liver.
|
|
|

|
|
Caput
Medusae This elderly female
with alcoholic cirrhosis has engorged abdominal veins in the knotted
appearance consistent with caput medusae. (Courtesy of Gary Schwartz,
MD.)
|
|
Differential Diagnosis
Emaciation, inferior vena caval
obstruction, superior vena caval obstruction, portal vein obstruction,
and superficial abdominal vein thrombosis can cause engorged abdominal
veins.
Emergency Department Treatment
and Disposition
Treatment is directed at the
underlying cause. This finding by itself does not require acute
treatment.
Clinical Pearl
1. Caput medusae has the same
clinical significance as the more common pattern of venous engorgement.
|
|
Abdominal Hernias
Associated Clinical Features
A hernia is a tissue protrusion
through an abnormal body cavity opening. Most abdominal wall hernias
occur at the groin and umbilicus. Incarceration is defined as the inability
to reduce the protruding tissue to its normal position. Strangulation
occurs when the blood supply of the hernia's contents is obstructed and
tissue necrosis ensues. An incisional hernia (Fig. 7.22) may
manifest clinically as a mass or palpable defect adjacent to a surgical
incision and can be reproduced by having the patient perform Valsalva's
maneuver. Obesity and wound infection, which interfere with wound
healing, predispose to the formation of incisional hernias. The defect of
an indirect inguinal hernia (Figs. 7.23, 7.24) is the internal
(abdominal) inguinal ring and may be manifest in either sex by a bulge
over the midpoint of the inguinal ligament that increases in size with
Valsalva's maneuver. A fingertip placed into the external ring through
the inguinal canal may palpate the defect. A direct hernia (Fig.
7.25) may be manifest by a bulge midway adjacent to the pubic tubercle
and may be felt by the pad of the finger placed in the inguinal canal.
The defect is in the posterior wall of the inguinal canal. Direct
inguinal hernias are usually painless and occur in males.
|
|
|

|
|
Incisional
Hernia An incisional hernia in
an obese female. (Courtesy of Stephen Corbett, MD.)
|
|
|
|
|

|
|
Indirect
Inguinal Hernia A recurrent
indirect inguinal hernia in a female patient. (Courtesy of Frank
Birinyi, MD.)
|
|
|
|
|

|
|

|
|
Indirect
Inguinal Hernia This
35-year-old man has an incarcerated indirect inguinal hernia (A) with
small bowel obstruction (B). (Courtesy of Lawrence B. Stack, MD.)
|
|
|
|
|

|
|
Direct
Inguinal Hernia A direct
inguinal hernia. Note the bulge adjacent to the left pubic tubercle.
(Courtesy of Daniel L. Savitt, MD.)
|
|
Nausea and vomiting may be
present if incarceration with bowel obstruction occurs. Strangulation can
lead to fever, peritonitis, and sepsis.
Differential Diagnosis
Tumor, aneurysm, lymphadenopathy,
bowel obstruction, ascites, lipoma, femoral hernia, hydrocele, testicular
torsion, and epididymitis may have similar presentations.
Emergency Department Treatment
and Disposition
When patients present without
clinical evidence of strangulation (fever, leukocytosis, systemic signs
of toxicity), reduction should be attempted. In the presence of these
signs, prompt surgical consultation is warranted for surgical reduction.
Reduction in the ED is facilitated with systemic analgesia (as most
patients present with significant pain), placing the patient in the
supine position, and applying a cold pack to the hernia. Routine
consultation for operative repair is indicated in asymptomatic patients
with reducible hernias.
Clinical Pearls
1. Acutely strangulated or
incarcerated hernias require immediate surgical evaluation.
2. Direct inguinal hernias are
usually painless.
3. Evaluation and treatment of
concomitant exacerbating conditions (cough, constipation, vomiting)
prevent recurrences.
|
|
Umbilical Hernias
Associated Clinical Features
The umbilicus is a common site of
abdominal hernias. Predisposing conditions in adults most commonly
include ascites and prior abdominal surgery. The size of the defect
determines the symptomatology and incidence of incarceration, with
smaller defects resulting in more pronounced symptoms and an increased
incidence of incarceration. Pain is located in the area of the fascial
defect. Contents of the hernia may be palpable and tender. Symptoms of
obstruction (nausea, vomiting, and abdominal distention) may be present.
If the hernia becomes strangulated (Fig. 7.26), erythema of the overlying
skin with fever and hypotension may occur.
|
|
|

|
|
Strangulated
Umbilical Hernia The skin
overlying a strangulated umbilical hernia is erythematous and tender.
(Courtesy of Lawrence B. Stack, MD.)
|
|
Differential Diagnosis
An omphalocele, gastroschisis, or
urachal duct cyst may present as an umbilical mass.
Emergency Department Treatment
and Disposition
Reduction is attempted in the
stable patient without clinical evidence of strangulation. Treatment of
any predisposing conditions (i.e., abdominal paracentesis in the patient
with tense ascites) may cause spontaneous reduction and avoid progression
of the hernia to strangulation. Routine consultation for elective repair
is indicated in asymptomatic patients with reducible hernias.
Clinical Pearls
1. Umbilical hernias in
children usually resolve without treatment.
2. Umbilical hernias in adults
usually become worse and require elective repair.
|
|
Patent Urachal Duct
Associated Clinical Features
When the vestigial urachal duct
is not obliterated during development, drainage can occur from the bladder
to the umbilicus (Fig. 7.27). Cysts can often be palpated between the
umbilicus and pubis. Besides drainage and pain, infection of the duct or
cyst may occur. Rarely, adenocarcinoma may form in these remnants.
|
|
|

|
|
Patent
Urachal Duct This 19-year-old
man presented to the ED with clear fluid (urine) draining from the
umbilicus, suggestive of a patent urachal duct. (Courtesy of Kevin J.
Knoop, MD, MS.)
|
|
Differential Diagnosis
Omphalocele, prune belly
syndrome, exstrophy of the bladder, gastroschisis, and umbilical hernias
are other abdominal wall abnormalities in children.
Emergency Department Treatment
and Disposition
Acute treatment is usually not
required unless an infection is evident. Routine urologic consultation
for surgical revision is indicated. A retrograde study with radiopaque
dye will outline the patent duct.
Clinical Pearl
1. This finding should prompt a
careful search for other urogenital anomalies.
|
|
Sister Mary Joseph's Node (Nodular Umbilicus)
Associated Clinical Features
A Sister Mary Joseph's node is a
metastasis manifesting as periumbilical lymphadenopathy secondary to
abdominal carcinoma (Fig. 7.28). Cancers of the colon may cause pain,
change in bowel habits, anemia, and obstruction. In general, left-sided
cancers cause obstruction, whereas right-sided tumors may have
significant metastases before they create signs and symptoms. These metastases
typically involve peritoneal and omental spread with distant metastases
to the liver. Spread to the umbilicus is colloquially known as the Sister
Mary Joseph's node.
|
|
|

|
|
Sister
Mary Joseph's Node Sister Mary
Joseph's nodule of patient with gastric carcinoma. (Courtesy of
Department of Dermatology, Naval Medical Center, Portsmouth, VA.)
|
|
Differential Diagnosis
Other umbilical masses to
consider include hernias, ascites, and urachal cysts.
Emergency Department Treatment
and Disposition
Prompt referral for staging and
treatment of the tumor is indicated. Other signs and symptoms (from
obstruction, blood loss, malnutrition, and pain) should be addressed and
treated.
Clinical Pearls
1. Virchow's node, presenting
as a supraclavicular mass, also heralds bowel carcinoma.
2. A Sister Mary Joseph's node
is commonly due to gastric carcinoma.
|
|
Abdominal Distention
Associated Clinical Features
Abdominal distention may be a
symptom—often described by the patient as the feeling of being
bloated—or a sign, an obvious protuberance of the patient's abdomen
that may or may not be out of proportion to the rest of the body. Other
findings vary widely, depending on the cause. In obesity, the abdomen is
uniformly rounded while an increase in girth and fat concurrently
accumulates in other parts of the body. In patients with ascites, there
may be shifting dullness, a fluid wave, bulging flanks, or hepatomegaly.
In patients with neoplasms, there may be a palpable mass. In gravid
patients, fetal heart tones may be present and fetal motion may be felt.
In patients with excess gas from bowel obstruction, there may be absent
or high-pitched bowel sounds and absence of bowel movements or flatus.
Differential Diagnosis
Numerous conditions present with
abdominal distention. Obesity, ascites, pregnancy, neoplasms, aneurysm,
tympanites (excess gas), organomegaly, and feces are important etiologies
to consider in the differential.
The profile of the fluid-filled
abdomen of ascites (Fig. 7.29) is a single curve from the xiphoid process
to the pubic symphysis. The umbilicus may be everted, and there may be
prominent superficial abdominal veins. Other physical findings suggestive
of ascites include shifting dullness and a fluid wave.
|
|
|

|
|
Ascites Ascites in an alcoholic man. Note the everted
umbilicus and prominent superficial abdominal veins. (Courtesy of
Alan B. Storrow, MD.)
|
|
The pregnant abdomen profile (Fig. 7.30) shows the
outward curve to be more prominent in the lower half of the abdomen. The
umbilicus may be everted in the last trimester of pregnancy. Prominent
abdominal wall veins may also be seen. The presence of fetal heart tones
confirms the diagnosis.
|
|
|

|
|
Gravid
Abdomen The abdomen of a woman
at 39 weeks' gestation. Note the abdominal wall striae, everted
umbilicus, and prominent superficial abdominal wall veins. (Courtesy
of Stephen Corbett, MD.)
|
|
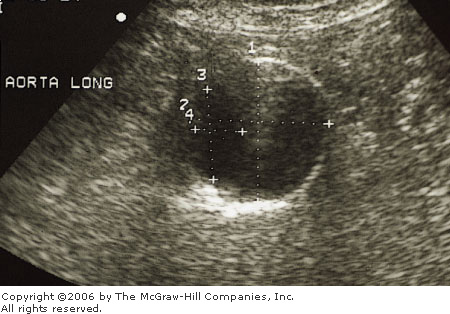
The abdominal profile of a patient with a leaking
abdominal aortic aneurysm (Fig. 7.31) shows a mottled abdominal wall
reflective of hypoperfusion of this structure. There may be a curve of
the midabdomen to either side of the aorta, more often on the left.
Palpation of a pulsatile mass supports the diagnosis. Ultrasound or
computed tomography (CT) of the abdomen will confirm the diagnosis.
|
|
|

|
|
|
|
Abdominal
Aortic Aneurysm A. The abdomen
of a patient with a leaking abdominal aortic aneurysm. Note the mottled
abdominal wall and the prominent curvature of the right side of the
abdomen. (Courtesy of Stephen Corbett, MD.) B. Abdominal aortic
aneurysm seen on ultrasound in another patient. (Courtesy of Sally
Santen, MD.)
|
|
Excess abdominal air (Fig. 7.32) can be located in
the lumen of the stomach or intestines or free in the peritoneum. This
abdominal profile is a single curve from the xiphoid process to the pubic
symphysis. Nausea, vomiting, decreased bowel sounds, and colicky pain are
present in a small bowel obstruction. Large bowel obstruction may be
accompanied by feculent vomiting and absent production of flatus.
|
|
|

|
|
Pseudoobstruction An 85-year-old woman was brought from a
nursing home with a complaint of abdominal distention and pain for 1
to 2 days. An eventual diagnosis of Ogilvie's syndrome, or
pseudoobstruction of the large bowel, was made. This is usually seen
in debilitated patients and can be treated with decompression.
(Courtesy of Stephen Corbett, MD.)
|
|
Emergency Department Treatment
and Disposition
Treatment varies widely depending
on the cause; thus emergent management is directed at determining the etiology.
Life-threatening causes (aneurysm, obstruction, neoplasms) require
stabilization and referral for definitive treatment.
Clinical Pearl
1. The "six f's" can
categorize conditions causing abdominal distention: fat, flatus, fetus,
fluid, feces, fatal growth.
|
|
Intertrigo
Associated Clinical Features
Intertrigo is a dermatitis
occurring on apposed surfaces of skin, such as the creases of the neck,
folds of the groin and armpit, or a panniculus (Fig. 7.33). It is
characterized by a tender, red plaque with a moist, macerated surface. A
candidal infection may result and often becomes secondarily infected with
skin flora. Erythema, fissures, burning, itching, exudates, and fever may
also accompany intertrigo.
|
|
|

|
|
Intertrigo
of the Panniculus Note the
exudate, erythema, and fissures of the abdominal wall. This patient
also had fever, suggesting secondary infection. (Courtesy of Lawrence
B. Stack, MD.)
|
|
Differential Diagnosis
Necrotizing fasciitis of the
abdominal wall, cellulitis, and Candida albicans infection should
be considered.
Emergency Department Treatment
and Disposition
Local care, empiric topical
antifungal treatment, and good personal hygiene are recommended.
Intravenous antibiotics initiated in the ED directed against skin flora
are recommended if there is secondary infection.
Clinical Pearl
1. Consider necrotizing
fasciitis of the abdominal wall if the patient appears septic.
|
|
Abdominal Wall Hematoma
Associated Clinical Features
Mild trauma may produce hematomas
of the rectus sheath (Fig. 7.34). This injury results in intense
abdominal pain, which can mimic an acute abdomen. The diagnosis is made
by physical examination, since the ecchymosis is not always visible.
Palpation of the abdominal wall reveals a tender mass that is accentuated
by contraction of the rectus. Ultrasound and computed tomography (CT) may
confirm the diagnosis.
|
|
|

|
|
Abdominal
Wall Hematoma This 50-year-old
man with chronic obstructive pulmonary disease developed
right-lower-quadrant pain after an episode of coughing. A repeat
examination on the second visit showed clearly visible ecchymosis.
There was no coagulopathy and amylase was normal. A CT scan revealed
a 10- by 8-cm hematoma in the right rectus abdominis sheath.
(Courtesy of Stephen Corbett, MD.)
|
|
Differential Diagnosis
Multiple causes of abdominal pain
must be considered in the differential diagnosis. Careful examination
with supplemental imaging studies, if needed, helps with the diagnosis.
Two classic signs of retroperitoneal bleeding are Grey-Turner's sign
(flank ecchymosis) and Cullen's sign (periumbilical ecchymosis).
Hemorrhagic pancreatitis and ruptured ectopic pregnancy, respectively,
should be considered.
Emergency Department Treatment
and Disposition
Assuming that there is no underlying
blood dyscrasia or coagulopathy, hematomas of the rectus sheath usually
resolve in 1 to 2 weeks.
Clinical Pearl
1. Fothergill's sign is
enhancement of a rectus sheath hematoma when the abdominal wall is
tensed. The mass should not cross the midline and should be easier to
palpate with abdominal muscle contractions. Intraabdominal masses are
more difficult to palpate with such contractions.
|
|
Abdominal Striae (Striae Atrophicae)
Associated Clinical Features
Abdominal striae are linear,
depressed, pink or bluish scar-like lesions (Fig. 7.35) that may later
become silver or white. They are caused by weakening of the elastic
cutaneous tissues from chronic stretching. They most commonly occur on
the abdomen but are also seen on the buttocks, breasts, and thighs.
Striae are commonly seen in obesity, pregnancy, Cushing's syndrome, and
chronic topical corticosteroid treatment. In Cushing's syndrome, a state
of adrenal hypercorticism, the skin becomes fragile and easily breaks
from normal stretching.
|
|
|

|
|
Abdominal
Striae These striae are seen
in a patient with recent weight gain, moon facies, and altered mental
status. The patient was diagnosed with Cushing's syndrome. (Courtesy
of Geisinger Medical Center, Department of Emergency Medicine,
Danville, PA.)
|
|
Differential Diagnosis
Obesity, pregnancy, Cushing's
syndrome, and chronic topical corticosteroid treatment should be considered.
Emergency Department Treatment
and Disposition
This finding seldom presents as a
condition requiring acute treatment; thus, attention is directed to
determining and treating the underlying cause.
Clinical Pearls
1. Recent striae (pink or blue)
with moon facies, hypertension, renal calculi, osteoporosis, and
psychiatric disorders are suggestive of Cushing's syndrome.
2. The striae caused by
pregnancy typically fade with time, unlike those associated with
Cushing's syndrome.
|
|