|
Note: Large images and
tables on this page may necessitate printing in landscape mode.
Copyright
©2006 The McGraw-Hill Companies. All rights reserved.
Emergency
Medicine Atlas > Part 1. Regional
Anatomy > Chapter 8. Urologic Conditions >
|
Testicular Torsion
Associated Clinical Features
These patients are most often
young men (average age 16 to 17.5 years) who present complaining of the
sudden onset of pain in one testicle. The pain is then followed by
swelling of the affected testicle, reddening of the overlying scrotal
skin, lower abdominal pain, nausea, and vomiting. An examination reveals
a swollen, tender, retracted testicle (Fig. 8.1) that often lies in the
horizontal plane (bell-clapper deformity) (Figs. 8.2 and 8.3). The
spermatic cord is frequently swollen on the affected side. In delayed
presentations, the entire hemiscrotum may be swollen, tender, and firm
(Fig. 8.4). The urine is usually clear with a normal urinalysis. In
one-third of cases there is a peripheral leukocytosis.
|
|
|

|
|
Testicular
Torsion Swollen, tender
hemiscrotum, with erythema of scrotal skin and retracted testicle.
(Courtesy of Stephen Corbett, MD.)
|
|
|
|
|
|
|
Bell-Clapper
Deformity A bell-clapper
deformity in testicular torsion results from the twisting of the
spermatic cord and causes the testis to be elevated, with a
horizontal lie. The lack of fixation of the tunica vaginalis to the
posterior scrotum predisposes the freely movable testis to rotation
and subsequent torsion. An elevated testis with a horizontal lie may
be seen in asymptomatic patients at risk for torsion.
|
|
|
|
|

|
|
Testicular
Torsion A retracted testicle
consistent with early testicular torsion is seen. (Courtesy of David
W. Munter, MD, MBA.)
|
|
|
|
|

|
|
Testicular
Torsion Swollen, tender
scrotal mass. (Courtesy of Patrick McKenna, MD.)
|
|
Differential Diagnosis
Alternative diagnoses that should
be considered include acute epididymitis, torsion of the testicular
appendix (Fig. 8.5), trauma, acute orchitis (mumps), hydrocele,
spermatocele, varicocele, hernia, and tumor. A good history and physical
examination helps narrow the diagnosis.
Emergency Department Treatment
and Disposition
Urologic consultation should be
obtained immediately and preparations made to go to the operating room
without delay. Doppler ultrasound or technetium scanning may be helpful
if these procedures will not delay surgery. In the interim, detorsion may
be attempted if the patient is seen within a few hours of onset: the
affected testicle should initially be opened like a book, that is, the
right testicle turned counterclockwise when viewed from below and the
left testicle turned clockwise when viewed from below. Pain relief should
be immediate. Decreased pain should prompt additional turns (as many as
three) to complete detorsion; increased pain should prompt detorsion in
the opposite direction. Ancillary studies should not delay operative intervention,
since testicular infarction will occur within 6 to 12 h after torsion.
Clinical Pearls
1. The cremasteric reflex is
almost always absent in testicular torsion.
2. Patients may report similar,
less severe episodes that spontaneously resolved in the recent past.
3. Half of all torsions occur
during sleep.
4. Abdominal or inguinal pain
is sometimes present without pain to the scrotum.
5. The age of presentation has
a bimodal pattern, since torsion is also more prevalent during infancy
and adolescence.
|
|
Torsion of a Testicular or Epididymal Appendix
Associated Clinical Features
Small vestigial remnants in the
embryology of the scrotum are often found on the superior portions of the
testicle or the epididymis. These appendages, which have no known
function, are occasionally on a stalk that is subject to torsion. This
most commonly occurs in boys up to 16 years of age but has been reported
in adults. The patient will complain of sudden pain around the superior
pole of the testicle or epididymis as the appendix undergoes necrosis and
inflammation. Early in the course, palpation of a firm, tender nodule in
this area will confirm the diagnosis.
Differential Diagnosis
Later in the course of
appendiceal torsion, swelling and pain generalize to the rest of the
scrotum. At this point the condition may be difficult to differentiate
from testicular torsion, acute epididymitis, or acute orchitis.
Hydrocele, spermatocele, varicocele, hernia, and tumor must also be
considered.
Emergency Department Treatment
and Disposition
Urologic consultation should be
obtained immediately. Differentiating from the more emergent testicular
torsion is the key responsibility. Ancillary studies are generally not
helpful in making this diagnosis unless it presents very early in its
course. A urinalysis is generally normal. The characteristic physical
signs of a small, tender, upper-pole nodule along with a color Doppler
ultrasound showing good flow to the testicle may mitigate the need for
emergent surgery. With later presentations or an equivocal ultrasound,
the diagnosis may not be made with confidence before surgery. Necrotic
appendices are excised if found during an exploration to rule out
testicular torsion. If surgery is not deemed necessary by the urologic
consultant, analgesics and rest are all that is required. The appendix
will involute and calcify in 1 to 2 weeks.
Clinical Pearls
1. Stretching of the scrotal
skin across the necrotic nodule will occasionally reveal a bluish
discoloration of the nodule, called the "blue-dot sign" (Fig.
8.5). This is pathognomonic for torsion of the appendix.
2. A reactive hydrocele may
accompany appendiceal torsion. When the hydrocele is transilluminated,
the blue-dot sign may be revealed.
|
|
|

|
|
Blue-Dot
Sign A blue-dot sign is caused
by torsion of the testicular appendix. It is best seen with the skin
held taut over the testicular appendix. (Courtesy of Javier A.
Gonzalez del Rey, MD.)
|
|
|
|
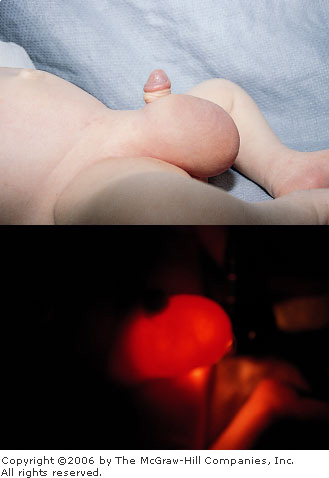
Hydrocele
Associated Clinical Features
Most hydroceles occur in older
patients and develop gradually without any significant symptoms. A
hydrocele generally presents as a soft, pear-shaped, fluid-filled cystic
mass anterior to the testicle and epididymis that will transilluminate
(Fig. 8.6). However, it can be tense and firm and will transilluminate
poorly if the tunica vaginalis is thickened. Almost all hydroceles in
children are communicating, resulting from the same mechanism that causes
inguinal hernia. A persistent narrow processus vaginalis acts like a
one-way valve, thus permitting the accumulation of dependent peritoneal
fluid in the scrotum. Acute symptomatic hydroceles are more rare and can
occur in association with epididymitis, trauma, or tumor.
|
|
|
|
|
Hydrocele Painless swelling in the scrotum of a young
boy (top). Transillumination of the swelling (bottom)
identifies the hydrocele. (Courtesy of Michael J. Nowicki, MD.)
|
|
Differential Diagnosis
Painless masses that must be
differentiated from hydrocele include spermatocele, varicocele, inguinal
hernia, and tumor. Painful masses to be differentiated include traumatic
hematocele, epididymitis, orchitis, and torsion.
Emergency Department Treatment
and Disposition
In an acute hydrocele, treatment
must be directed at discovering a possible underlying cause. A positive
urinalysis may point toward an infectious etiology. Transillumination
helps demonstrate whether the mass is cystic or solid. Ultrasound can be
very helpful in imaging the scrotal contents and delineating the
composition of the mass. Acute hydroceles should not be considered benign
and require referral to a urologist to rule out tumor or infection.
Chronic accumulations are referred to a urologist on a more routine basis
for elective drainage.
Clinical Pearls
1. Ten percent of testicular
tumors have a reactive hydrocele as the presenting complaint.
2. An inguinal hernia with a
loop of bowel in it may emit bowel sounds.
3. Hydroceles are almost never
symptomatic.
4. Acute reactive hydroceles
may be caused by infection, trauma, or torsion.
|
|
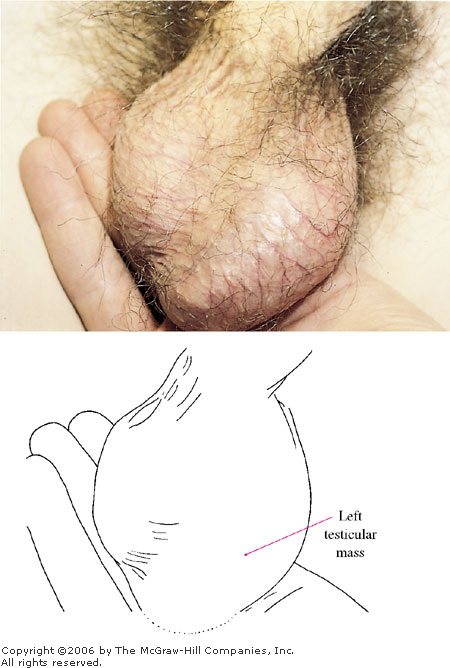
Testicular Tumor
Associated Clinical Features
In testicular tumor, a painless,
firm testicular mass (Fig. 8.7) is palpated, with the patient often
complaining of a "heaviness" of his testicle. If the patient
presents early, the mass will be distinct from the testis, whereas later
presentations will have generalized testicular or scrotal swelling. These
lesions occasionally present with pain due to infarction of the tumor.
|
|
|
|
|
Testicular
Tumor This painless left
testicular mass is highly suspicious for tumor, as proved to be the
case in this patient. (Courtesy of Patrick McKenna, MD.)
|
|
Differential Diagnosis
Epididymitis is the most frequent
misdiagnosis, which unfortunately may delay surgical intervention. When
the tumor presents with infarction pain, differentiation from
epididymitis or torsion can be difficult. In some cases, ultrasound can
help differentiate these entities.
Emergency Department Treatment
and Disposition
Patients should be promptly
referred to a urologist for surgical exploration.
Clinical Pearls
1. Acute hydroceles and
hematoceles should prompt the physician to consider a tumor as the cause.
2. Pain from tumor infarction
is usually not as severe as pain due to torsion or epididymitis.
3. Findings of an unexplained
supraclavicular lymph node, abdominal mass, or chronic nonproductive
cough resistant to conventional therapy should prompt a testicular
examination for tumor.
|
|
Scrotal Abscess
Associated Clinical Features
A scrotal abscess is a
suppurative mass with surrounding erythema involving the superficial
layers of the scrotal wall (Fig. 8.8). The usual history is of
progressive swelling of a small pustule or papule followed by increasing
pain and induration or fluctuance. Constitutional symptoms and fever are
generally absent.
|
|
|

|
|
Scrotal
Abscess Suppurative mass on
the scrotum. (Courtesy of David Effron, MD.)
|
|
Differential Diagnosis
An apparently superficial scrotal
abscess must be distinguished from a deep scrotal abscess or early
Fournier's gangrene. In the latter two cases, patients tend to appear
quite ill. The erythema of the skin overlying an abscess should not be
mistaken for an urticarial reaction, erythema multiforme, or drug
eruption.
Emergency Department Treatment
and Disposition
Using local anesthesia, simply
make a stab incision and drain the abscess. The patient is then
instructed to use a sitz bath and to change the dressing frequently. An
alternative method of treatment is to unroof the abscess by
circumferential excision. This ensures that there is adequate wound drainage.
Immunocompromised patients may require intravenous antibiotics and
admission.
Clinical Pearl
1. If the patient appears ill
out of proportion to the superficial appearance, suspect that this mass
is the point of a deep scrotal abscess.
|
|
Fournier's Gangrene
Associated Clinical Features
Fournier's gangrene most
frequently occurs in a middle-aged diabetic male who presents with
swelling, erythema, and severe pain of the entire scrotum (Fig. 8.9), but
it is also known to occur in females (Fig. 8.10). In males, the scrotal
contents often cannot be palpated because of the marked inflammation. The
patient has constitutional symptoms with fever and frequently is in
shock. There is often a history of recent urethral instrumentation, an
indwelling Foley catheter, or perirectal disease. A localized area of
fluctuance cannot be appreciated.
|
|
|

|
|
Fournier's
Gangrene Markedly swollen,
necrotic, tender scrotum, perineum, and adjacent thighs are seen.
(Courtesy of David Effron, MD.)
|
|
|
|
|

|
|
Fournier's
Gangrene Swollen, tender,
erythematous labia, perineum, and inner thighs in a female patient
with Fournier's gangrene. (Courtesy of Daniel L. Savitt, MD.)
|
|
Differential Diagnosis
The differential diagnosis
includes cellulitis, superficial scrotal abscess, edema due to heart
failure or lymphatic obstruction, allergic reaction, and
epididymoorchitis with skin fixation.
Emergency Department Treatment
and Disposition
These patients require aggressive
fluid resuscitation and early surgical consultation for immediate
debridement and surgical drainage. Broad-spectrum antibiotics effective
against gram-positive, gram-negative, and anaerobic organisms should be
given as soon as possible in the ED. There is anecdotal experience that
treatment is enhanced by hyperbaric oxygen.
Clinical Pearls
1. Pain out of proportion to
the clinical findings may represent an early presentation of Fournier's
gangrene.
2. A plain pelvic radiograph
may reveal subcutaneous air.
3. Fournier's gangrene is
usually quite painful but has been known to present with only a mildly
uncomfortable necrosis of the scrotal wall and exposed testis.
|
|
Paraphimosis
Associated Clinical Features
Paraphimosis is the entrapment of
a retracted foreskin that cannot be reduced behind the coronal sulcus (Fig.
8.11). Pain, swelling, and erythema are common. If severe, the
constriction causes edema and venous engorgement of the glans, which can
lead to arterial compromise with subsequent tissue necrosis.
|
|
|

|
|
Paraphimosis Moderate edema of retracted foreskin, which is
entrapped behind the coronal sulcus. (Courtesy of Alan C. Heffner,
MD.)
|
|
Differential Diagnosis
In contrast to paraphimosis,
phimosis is the inability to retract the foreskin (Fig. 8.12), usually a
chronic condition. Other diagnoses to consider include superficial
balanitis, hair tourniquet, contact dermatitis, and urticaria.
|
|
|
|
|
Phimosis In phimosis, the foreskin cannot be retracted,
often due to meatal stenosis and scarring.
|
|
Emergency Department Treatment
and Disposition
Squeezing the glans firmly for 5
min to reduce the swelling can lead to successful reduction of the
foreskin. Local infiltration of anesthesia with vertical incision of the
constricting band should be performed by a urologist if manual reduction fails.
Clinical Pearls
1. In the presence of arterial
compromise, if a urologist is not immediately available, the emergency
physician should incise the constricting band.
2. The patient should be
referred to a urologist for circumcision if successfully reduced.
3. Phimosis is
"physiologic" in young males (generally less than 5 to 6 years
old).
4. Phimosis, if
"reduced" (retracted proximally over the glans), can cause a
paraphimosis—a true emergency.
|
|
Priapism
Associated Clinical Features
These patients present with
persistent, usually painful erection due to pathologic engorgement of the
corpora cavernosa (Fig. 8.13). Patients may present within several hours
or several days of their first symptoms. The glans penis and corpus
spongiosum are generally not engorged and remain flaccid. The physiology
is either arterial, which is generally traumatic, or venoocclusive.
Reversible causes of venoocclusive disease include sickle cell disease,
direct injection of erectile agents, and leukemic infiltration. Nonreversible
causes include idiopathic ones—the most common, spinal cord
lesions, and a variety of medications.
|
|
|

|
|
Priapism A painful persistent erection due to
pathologic engorgement of the corpora cavernosa is seen in this
patient with sickle cell disease. The glans penis and corpus
spongiosum are not engorged (Courtesy of Kevin J. Knoop, MD, MS.)
|
|
Differential Diagnosis
Priapism is confirmed when there
is a prolonged erection with a flaccid glans and corpus spongiosum. The
history and physical examination should be directed toward signs of
trauma, infection, medications, drug use, and the diseases that
predispose to priapism. Traumatic priapism is more flaccid and generally
less painful than the venoocclusive form.
Emergency Department Treatment
and Disposition
The diseases that are associated
with reversible priapism should be treated. Ice packs to the perineum
have traditionally been recommended but are frequently unsuccessful.
Terbutaline given orally or subcutaneously occasionally reverses
priapism. Aspiration of blood from the corpus cavernosum can lead to
detumescence and should be followed by a compressive dressing. Injectable
erectile agents can be reversed by aspiration followed by intracavernous
injection of alpha-adrenergic agents such as phenylephrine. Urologic
consultation should be obtained immediately for traumatic or persistent
priapism despite initial treatment, with close urologic follow-up for
those that are successfully reversed in the ED. Patients with persistent
priapism despite treatment must frequently undergo surgery.
Clinical Pearls
1. Patients should be advised
that impotence is a frequent complication of priapism, regardless of the
length of the symptoms or the success of any treatment.
2. Although the glans penis and
corpus spongiosum are generally not affected, urinary retention often
accompanies priapism.
|
|
Urethral Rupture
Associated Clinical Features
Urethral injury is rarely an
isolated event; it is often associated with multiple trauma. Anterior
urethral injuries are most often the result of a straddle injury and may
present late (many patients are still able to void), with a local infection
or sepsis from extravasated urine. Posterior urethral injuries occur in
motor vehicle and motorcycle accidents and are usually the result of
pelvic fractures. Patients have blood at the urethral meatus (Fig. 8.14),
cannot void, and have perineal bruising. In males, the prostate is often
boggy or free-floating or may not be palpable at all if there is a
retroperitoneal hematoma between the prostate and the rectum.
|
|
|

|
|
Urethral
Rupture Blood at the urethral
meatus in a patient with urethral rupture secondary to trauma.
(Courtesy of David Effron, MD.)
|
|
Differential Diagnosis
Bladder rupture, higher urinary
tract injuries, urethritis, and penile fracture may all present with
blood at the meatus.
Emergency Department Treatment
and Disposition
Urethral instrumentation such as
Foley catheterization should not occur prior to a retrograde urethrogram
with highly concentrated water-soluble contrast. If there is only a
partial anterior tear, a gentle attempt at catheterization can be made if
it is abandoned at the first sign of resistance. If catheterization is
unsuccessful and whenever there is a posterior tear, a suprapubic
catheter should be placed in the ED with a trocar if relief of bladder
distention is required prior to operative repair.
Clinical Pearls
1. Foley catheter insertion is
contraindicated in patients with a suspected urethral injury prior to a
retrograde urethrogram.
2. Urethral injury should be
suspected in the multiple trauma patient who is unable to void or has
blood at the meatus, a high-riding prostate, or perineal trauma.
3. Vaginal lacerations due to
trauma in females should prompt consideration of a urethral tear.
4. Occasionally urine from an
anterior urethral tear will extravasate into the scrotum, causing marked
swelling.
5. Posterior injuries are
frequently associated with other intraabdominal injury.
|
|
Fracture of the Penis
Associated Clinical Features
Patients usually present
complaining of trauma during sexual arousal and often relate experiencing
a sudden "snapping" sound or sensation, pain, and deformity,
which is caused by a tearing of the tunica albuginea. The shaft of the
penis is swollen and often angulated at the fracture site (Fig. 8.15).
|
|
|

|
|
Fractured
Penis A swollen, ecchymotic
penis is shown. Note the angulation at the midshaft of the penis,
indicating the "fracture" site. Blood at the meatus, as
shown here, is further evidence of a urethral injury. (Courtesy of
Kevin J. Knoop, MD, MS.)
|
|
Differential Diagnosis
Penile fracture can be confused with
penile trauma without tear of the tunica albuginea, urethral injury,
Peyronie's disease (dorsal contracture), priapism, or foreign bodies.
Emergency Department Treatment
and Disposition
If the patient cannot urinate, a
retrograde urethrogram may be required to rule out urethral injury (Fig.
8.16). These patients require admission and referral to a urologist, who
frequently takes them immediately to the operating room for repair.
|
|
|

|
|
Fractured
Penis Retrograde urethrogram
showing urethral injury from the fractured penis in Fig. 8.15.
(Courtesy of David W. Munter, MD.)
|
|
Clinical Pearls
1. Patients sometimes concoct
elaborate, non-sexually-related stories surrounding the circumstances of
injury, but penile fracture most commonly occurs during sexual arousal.
2. Penile implants are also
subject to injury in a similar fashion.
|
|
Straddle Injury
Associated Clinical Features
In straddle injury, the patient
has pain, swelling, contusion, and hematoma of the perineum or scrotum
following direct blunt trauma (Figs. 8.17 and 8.18). This injury is
commonly caused by a fall onto a bicycle frame cross-tube, playground
equipment, or a toilet seat. Swelling can be severe enough to interfere
with urination. Scrotal contents can also be contused or crushed with
this injury.
|
|
|

|
|
Straddle
Injury Ecchymosis, swelling,
and contusion of the perineum in a 3-year-old female who tripped and
fell on a large plastic toy. (Courtesy of James Mensching, MD.)
|
|
|
|
|

|
|
Straddle
Injury Contusion of the
scrotum and lower abdomen in a young boy consistent with a straddle
injury. (Courtesy of David W. Munter, MD.)
|
|
Differential Diagnosis
Fournier's gangrene, cellulitis,
and urticaria are similar in appearance but without the history of
trauma. Sexual or physical abuse should be considered.
Emergency Department Treatment
and Disposition
Treatment is supportive and
includes cold packs, elevation, rest, and analgesics. If unable to void,
the patient may require catheterization.
Clinical Pearls
1. Laceration of the perineum
can be obscured by swelling if a careful examination is not performed.
2. Pelvic radiographs should be
obtained in all perineal injuries.
3. Males and females are at
high risk for urethral injuries with this type of injury.
4. Straddle injury is
differentiated from abuse with a good history from a reliable caregiver
that matches the injury.
|
|
Balanoposthitis
Associated Clinical Features
Balanoposthitis is an infection
and inflammation of the glans penis that also involves the overlying
foreskin (prepuce) (Fig. 8.19). Balanitis is isolated to the
glans, whereas posthitis involves only the prepuce. Pain, erythema,
and edema of the affected parts of the penis are typically present.
Patients may refrain from urination secondary to dysuria, or the edema
may induce meatal occlusion, leading to urinary retention or obstruction.
Common etiologies include overgrowth of normal bacterial flora secondary
to poor hygiene (pediatric patients), sexually transmitted diseases
(adolescents and adults), and candidal infections (the elderly or
immunocompromised) (Fig. 8.20).
|
|
|

|
|
Balanoposthitis Note the erythema, localized edema, and
significantly constricted preputial orifice of the distal penis.
(Courtesy of Lawrence B. Stack, MD.)
|
|
|
|
|

|
|
Balanitis Candidal balanitis in an elderly patient with
no other complaints. New-onset diabetes was diagnosed. (Courtesy of
Kevin J. Knoop, MD, MS.)
|
|
Differential Diagnosis
The diagnosis is usually
straightforward; however, the underlying etiology often must also be
addressed. Examples are sexually transmitted diseases in healthy adults
and diseases associated with immunocompromise (e.g. diabetes mellitus,
AIDS, alcoholism). Phimosis occurs when chronic infection due to poor
hygiene causes fibrosis and contracture of the preputial opening. Other
diagnoses to consider include contact dermatitis, fixed drug eruptions,
lichen sclerosus et atrophicus, and squamous cell carcinoma.
Emergency Department Treatment
and Disposition
Treatment is directed at the
suspected etiology. Warm soaks and topical antibiotics (bacitracin) are
the mainstay of therapy for infectious etiologies owing to poor hygiene.
Parents should be counseled about proper cleansing and handling of the
prepuce. Oral or intravenous antibiotics may be indicated if there is an
accompanying cellulitis. If urinary obstruction is present,
catheterization may be attempted using a small catheter. If
catheterization is unsuccessful, urologic consultation for emergent
surgical correction of the prepuce is required. Candidal infections are
treated with meticulous hygiene and topical antifungal agents. Routine
urologic referral is indicated for suspected lichen sclerosus et
atrophicus and squamous cell carcinoma.
Clinical Pearls
1. The inability to retract the
foreskin completely is normal in young males up to age 4 or 5. Attempting
to do so could cause a paraphimosis, a true emergency.
2. Placing the child in a
bathtub with warm water will help alleviate difficulty with micturition
assuming that no obstruction is present.
3. Candidal balanitis or
balanoposthitis may be associated with an undiagnosed immunocompromised
state.
4. Suspected sexually
transmitted diseases require treatment for the partners as well.
|
|