|
Note: Large images and
tables on this page may necessitate printing in landscape mode.
Copyright
©2006 The McGraw-Hill Companies. All rights reserved.
Emergency
Medicine Atlas > Part 1. Regional
Anatomy > Chapter 9. Sexually Transmitted Diseases and
Anorectal Conditions > Sexually Transmitted Diseases >
|
Primary Syphilis
Associated Clinical Features
Lesions of primary syphilis
generally appear after an incubation period of 2 to 6 weeks, but they may
appear up to 3 months after exposure. The patient usually presents with a
solitary round to oval painless genital ulcer (Figs. 9.1 and 9.2).
However, the ulcer may be slightly painful, and several lesions are
sometimes seen. The base of the genital ulcer is dry in males, moist in
females; purulent fluid in the base is uncommon. The borders of the ulcer
are often indurated. Patients may develop ulcers at any site of
inoculation on the body. Bilateral, nontender, nonfluctuant adenopathy is
common. Lesions resolve spontaneously in 3 to 12 weeks without treatment
as the infection progresses to the secondary stage. Patients with primary
syphilis are at risk for concurrent infection with other sexually transmitted
diseases.
|
|
|

|
|
Primary
Chancre—Male This
dry-based, painless ulcer with indurated borders is typical for a primary
chancre in a male patient. (Courtesy of A. Wisdom: Sexually
Transmitted Diseases. London: Mosby-Wolfe; 1992.)
|
|
|
|
|

|
|
Primary
Chancre—Female A
solitary, painless genital chancre with a clean base in a patient
with primary syphilis. (Courtesy of the Department of Dermatology,
Naval Medical Center, Portsmouth, VA.)
|
|
Differential Diagnosis
Behçet's disease, fixed drug
eruption, recurrent genital herpes, chancroid, squamous cell carcinoma,
and lesions caused by trauma can have a similar appearance.
Emergency Department Treatment
and Disposition
Treat with benzathine penicillin
G, 2.4 million units IM once. Penicillin-allergic patients should be
given doxycycline, 100 mg PO bid for 2 weeks. Other alternatives include
tetracycline, 500 mg PO qid for 2 weeks; erythromycin base, 500 mg PO qid
for 2 weeks; or ceftriaxone, 250 mg IM once daily for 10 days. An RPR or
VDRL should be checked. Partners within the last 90 days should be
treated presumptively; partners over the last 90 days should be treated
on the basis of their serologic testing results. This is a reportable
disease, and appropriate paperwork should be filed.
Clinical Pearls
1. Lesions are usually painless
and solitary, but they may be slightly painful; two or three lesions may
also be seen.
2. Consider dark-field
examination of the lesion to rapidly confirm the diagnosis.
3. Chancres of primary syphilis
can occur anywhere on the body at the site of inoculation.
4. Evaluate patients with
primary syphilis for concurrent sexually transmitted diseases and treat
accordingly.
|
|
Secondary Syphilis
Associated Clinical Features
The rash of secondary syphilis
often occurs 2 to 10 weeks after resolution of the primary lesions. It
begins as a nonpruritic macular rash that evolves into a papulosquamous
rash involving primarily the trunk, palms, and soles (Figs. 9.3, 9.4,
9.5). The rash is often annular in shape. Diffuse, painless
lymphadenopathy is also seen at this stage. Mucous patches represent
mucous membrane involvement of the tongue and buccal mucosa (Fig. 9.6).
Condyloma lata (Fig. 9.7) can be seen during this stage, as can patchy
alopecia. The manifestations of this stage resolve without treatment in
several months.
|
|
|

|
|
Secondary
Syphilis—Trunk Rash on
trunk in secondary syphilis. (Courtesy of A. Wisdom: Sexually
Transmitted Diseases. London: Mosby-Wolfe; 1992.)
|
|
|
|
|

|
|
Secondary
Syphilis—Palms
Papulosquamous rash of secondary syphilis. Note the annular
appearance of the palmar rash. (Courtesy of H. Hunter Handsfield: Atlas
of Sexually Transmitted Diseases. New York: McGraw-Hill; 1992.)
|
|
|
|
|

|
|
Secondary
Syphilis—Soles
Hyperkeratotic plantar rash in a patient with secondary syphilis.
(Courtesy of H. Hunter Handsfield: Atlas of Sexually Transmitted
Diseases. New York: McGraw-Hill; 1992.)
|
|
|
|
|
|
|
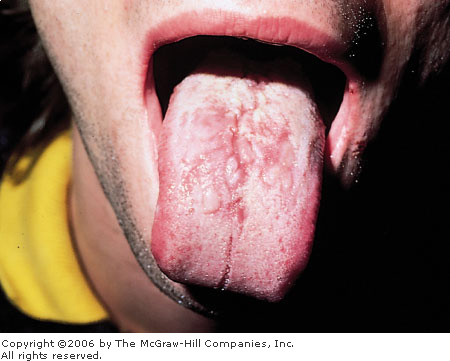
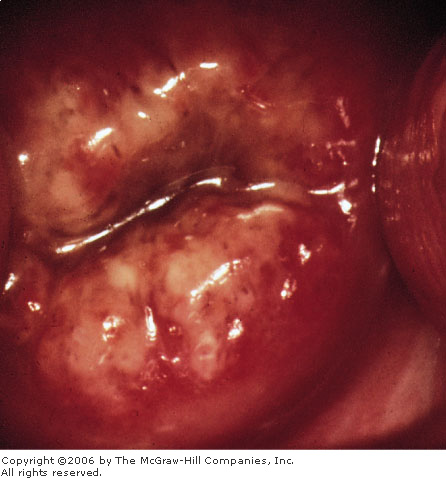
Mucous
Patches Oral involvement in
secondary syphilis manifest by mucous patches. These lesions are very
infectious, and dark-field examination is often positive for
spirochetes. (Courtesy of Morse, Moreland, Thompson: Atlas of
Sexually Transmitted Diseases. London: Mosby-Wolfe; 1990.)
|
|
|
|
|

|
|
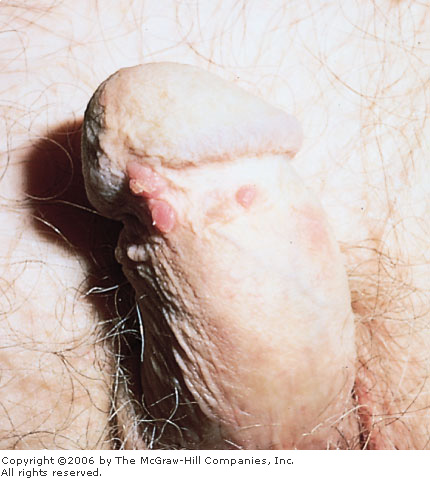
Condyloma
Lata Typical appearance of the
verrucous, heaped up lesions of condyloma lata, a manifestation of
secondary syphilis. (Courtesy of H. Hunter Handsfield: Atlas of
Sexually Transmitted Diseases. New York: McGraw-Hill; 1992.)
|
|
Differential Diagnosis
The differential diagnosis
depends on the site involved:
Rash: Pityriasis
rosea, psoriasis, lichen planus, Reiter's syndrome, viral syndrome, allergic
rash
Mucous patches: Apthous
ulcerations, thrush
Condyloma lata: Condyloma
accuminata, squamous cell carcinoma, granuloma inguinale
Emergency Department Treatment
and Disposition
Benzathine penicillin G, 2.4
million units IM once; penicillin allergic patients should receive
doxycycline, 100 mg PO bid for 2 weeks. RPR or VDRL should be sent and
titers followed to determine adequate response to therapy. Suspected and
confirmed cases of syphilis must be reported to public health officials.
Clinical Pearls
1. Lesions of secondary
syphilis are very infectious. It is prudent to always wear gloves when
examining a patient with a rash that may be due to secondary syphilis.
2. Consider using dark-field
examination of scrapings of the rash, mucous patches, and condyloma lata
to make a rapid diagnosis.
3. Patients should be warned
about the potential development of the Jarish-Herxheimer reaction after
they are treated. This syndrome, characterized by fever, headache,
malaise, and myalgias, occurs within 24 h of treatment and is caused by
massive release of pyrogens by the dying spirochetes.
|
|
Gonorrhea
Associated Clinical Features
Gonorrhea often becomes manifest
after a short incubation period of 2 to 5 days. In men, urethritis is
characterized by purulent, usually copious urethral discharge (Fig. 9.8)
with dysuria; however, up to 10% of men are asymptomatic. Women may also
develop urethritis (Fig. 9.9) and complain of dysuria. Cervicitis is
often asymptomatic. If symptomatic, women may complain of increased vaginal
discharge or vaginal spotting, particularly after intercourse. On
speculum examination, the cervix is friable, with a mucopurulent
endocervical exudate (Fig. 9.10). Patients with gonococcal conjunctivitis
have chemosis and copious purulent exudate (Fig. 9.11); untreated, these
patients can develop endophthalmitis and perforation of the globe.
Untreated gonorrhea may disseminate and more commonly does so in women.
Disseminated gonococcal infection (DGI) typically presents with a
monoarticular septic arthritis usually involving the knees, ankles,
elbows, or wrists. Skin lesions are necrotic pustules on an erythematous
base; they may ulcerate and are more commonly found on the distal
extremities (Figs. 9.12, 9.13).
|
|
|
|
|
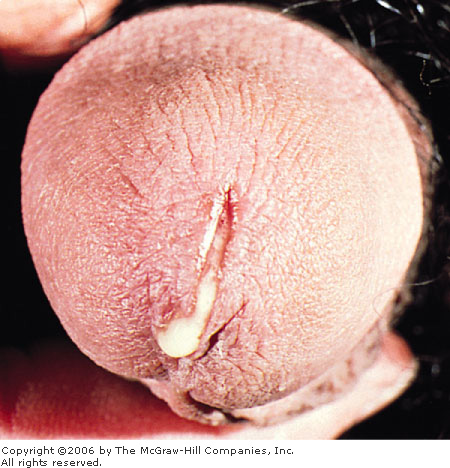
Male
Urethritis Purulent, copious
urethral discharge in a patient with gonococcal urethritis. (Courtesy
of H. Hunter Handsfield: Atlas of Sexually Transmitted Diseases. New
York: McGraw-Hill; 1992.)
|
|
|
|
|

|
|
Female
Urethritis Gonococcal
urethritis in a female patient. Note the purulent urethral discharge.
(Courtesy of Morse, Moreland, Thompson: Atlas of Sexually
Transmitted Diseases. London: Mosby-Wolfe; 1990.)
|
|
|
|
|
|
|
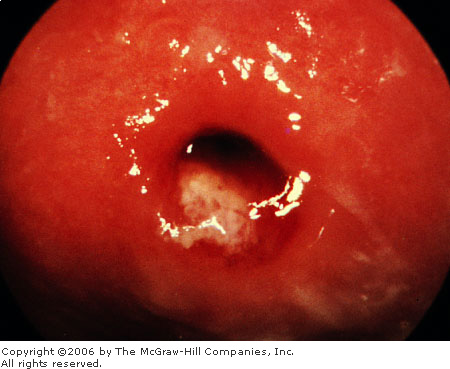
Cervicitis Endocervical purulent exudate in an
asymptomatic patient with gonococcal cervicitis. The cervix is very
friable. (Courtesy of King K. Holmes, MD, from H. Hunter Handsfield: Atlas
of Sexually Transmitted Diseases. New York: McGraw-Hill; 1992.)
|
|
|
|
|

|
|
Conjunctivitis Chemotic conjunctiva and copious purulent
exudate in a patient with gonococcal conjunctivitis. (Courtesy of H.
Hunter Handsfield: Atlas of Sexually Transmitted Diseases. New
York: McGraw-Hill; 1992.)
|
|
|
|
|

|
|
Skin
Lesions Small pustules with
hemorrhage suggestive of the skin lesions of disseminated gonococcal
infection. (Courtesy of H. Hunter Handsfield: Atlas of Sexually
Transmitted Diseases. New York: McGraw-Hill; 1992.)
|
|
|
|
|

|
|
Bartholin's
Cyst Enlarged, fluctuant,
tender Bartholin's abscess of the labia, usually but not always a
result of gonorrhea. (Courtesy of A. Wisdom: Sexually Transmitted
Diseases. London: Mosby-Wolfe; 1992.)
|
|
Differential Diagnosis
The differential diagnosis
depends on the site involved:
Urethritis and cervicitis:
Chlamydia, Mycoplasma, Ureaplasma
Conjunctivitis: Bacterial
conjunctivitis, chemical conjunctivitis
Arthritis: Septic
arthritis, rheumatic fever, hepatitis B prodrome, immune complex disease,
Reiter's syndrome, systemic lupus erythematosus
Skin lesions:
Folliculitis, subacute bacterial endocarditis (septic emboli)
Emergency Department Treatment
and Disposition
Treatment is dependent on the
site of infection:
Urethritis and cervicitis: Ceftriaxone,
125 mg IM once; cefixime, 400 mg PO once; ciprofloxacin, 500 mg PO once;
ofloxacin, 400 mg PO once.
Conjunctivitis: Ceftriaxone
1 g IM once; eye irrigation.
Disseminated gonococcal
infection: Ceftriaxone, 1 g IV or IM daily for 7 to 10 days; may
treat with 1 to 2 days of IM ceftriaxone and then change to cefixime, 400
mg PO bid, or ciprofloxacin, 500 mg PO bid, to complete a 7- to 10-day
course. Sexual partners should be notified and treated. Gonorrhea is a
reportable disease.
Clinical Pearls
1. Patients with gonorrhea need
to be treated for concurrent infection with Chlamydia. Coinfection
with these organisms is seen in 30% of men with urethritis and 50% of
women with cervicitis.
2. Gonococcal arthritis is the
most common cause of monoarticular arthritis in young, sexually active
patients.
3. Suspect gonococcal
conjunctivitis in patients with copious eye discharge and chemosis.
4. Cultures are the gold
standard for confirming the diagnosis of gonorrhea. Selective media
should be used when specimens are obtained from the cervix, pharynx,
urethra, or rectum. Nonselective medium (blood agar) should be used in
culturing joint fluid, blood, or cerebrospinal fluid.
|
|
Chlamydial Infection
Associated Clinical Features
After an incubation period of 1
to 3 weeks, males with urethritis may present with a thin, often clear
urethral discharge and dysuria (Fig. 9.14). Up to 10% of these men may be
asymptomatic. Women may also develop urethritis, which may only cause
dysuria and be misdiagnosed as a urinary tract infection. Cervicitis in
women (Fig. 9.15) is almost always asymptomatic. Women may develop pelvic
inflammatory disease with upper genital tract infection. Men may develop
epididymitis.
|
|
|
|
|
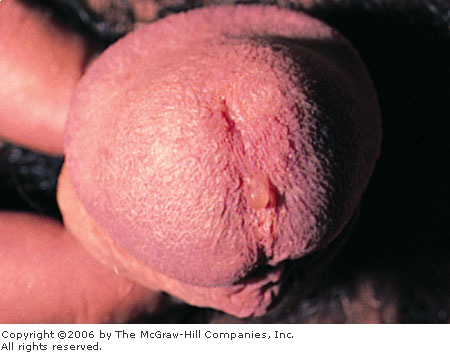
Male
Urethritis Thin urethral
discharge of chlamydial urethritis. (Courtesy of Walter Stamm, MD,
from H. Hunter Handsfield: Atlas of Sexually Transmitted Diseases.
New York: McGraw-Hill; 1992.)
|
|
|
|
|

|
|
Cervicitis Mucopurulent cervicitis from chlamydial
infection. (Courtesy of H. Hunter Handsfield: Atlas of Sexually
Transmitted Diseases. New York: McGraw-Hill; 1992.)
|
|
Differential Diagnosis
For urethritis and cervicitis, Neisseria
gonorrhoeae, Mycoplasma, and Ureaplasma should be considered.
Emergency Department Treatment
and Disposition
The preferred treatment consists
of azithromycin, 1 g PO once, or doxycycline 100 mg PO bid for 7 days.
Alternatives include ofloxacin, 500 mg PO bid for 7 days. Pregnant women
should receive erythromycin base, 500 mg, or erythromycin ethylsuccinate
800 mg PO qid for 7 days. Partners should be examined and treated
appropriately.
Clinical Pearls
1. Chlamydial infection often
accompanies gonococcal infection, and patients being treated for
gonorrhea should also be treated for chlamydial infection.
2. Women with chlamydial
infections may be completely asymptomatic for long periods of time.
3. Consider syphilis serologic
testing and HIV testing in patients presenting with sexually transmitted
diseases.
|
|
Lymphogranuloma Venereum
Associated Clinical Features
Lymphogranuloma venereum (LGV) is
caused by a serotype of Chlamydia trachomatis and is primarily a
disease of lymphatic tissue. Initially, LGV is often a painless genital
ulceration that is not noticed by the patient more than 90% of the time.
Patients often present with painful, nonfluctuant inguinal adenopathy,
which is often but not always unilateral (Fig. 9.16). Lymph-adenopathy
may lie above and below the inguinal ligament, causing the "groove
sign" suggestive of this diagnosis. The lesion of lymphadenopathy
may spontaneously open into draining sinus tracts to the skin.
|
|
|

|
|
Lymphogranuloma
Venereum Unilateral left
lymphadenopathy in a patient with lymphogranuloma venereum. (Courtesy
of Lawrence B. Stack, MD.)
|
|
Differential Diagnosis
Chancroid, granuloma inguinale,
lymphoma, pyogenic or mycobacterial infection, syphilis, and cat-scratch
disease may have a similar appearance.
Emergency Department Treatment
and Disposition
Doxycycline, 100 mg PO bid for 3
weeks. Rarely, patients may need needle aspiration of the lymph nodes if
they become fluctuant. Serologic testing is needed to confirm the
diagnosis.
Clinical Pearls
1. Patients rarely note the
evanescent ulcer associated with LGV.
2. The lymphadenopathy of LGV
progresses over several weeks.
3. Treatment for LGV requires 3
weeks of therapy for a cure.
|
|
Genital Herpes
Associated Clinical Features
Herpes genitalis presents in
several ways: symptomatic primary infection, first-episode nonprimary
infection, and recurrent infection. Symptomatic primary infection occurs
when the patient develops symptoms upon first acquiring the virus. Some
patients may be asymptomatic when primarily infected with the virus,
however, and present at a later time with their first symptomatic episode
of nonprimary genital herpes. Patients with either symptomatic primary
infection or first-episode nonprimary infection may develop recurrences.
Symptomatic primary genital
herpes is characterized by multiple vesicles that quickly ulcerate into
shallow, painful ulcers (Figs. 9.17, 9.18). The ulcers may coalesce. The
lesions are accompanied by a viral syndrome with low-grade fever and
myalgias. Up to 10% of patients may develop aseptic meningitis. Women may
develop sacral autonomic dysfunction and require urinary catheterization
because of urinary retention. The lesions last up to 3 weeks and heal
without scarring.
|
|
|

|
|
Primary
Lesions—Female Multiple
coalescing superficial ulcerations of primary genital herpes.
(Courtesy of Lawrence B. Stack, MD.)
|
|
|
|
|

|
|
Primary
Lesions—Male Multiple
genital vesicles of primary genital herpes. (Courtesy of H. Hunter
Handsfield: Atlas of Sexually Transmitted Diseases. New York:
McGraw-Hill; 1992.)
|
|
First-episode nonprimary genital herpes and recurrent
genital herpes are less dramatic (Fig. 9.19). Patients with first-episode
nonprimary genital herpes do not have systemic symptoms, have solitary to
several painful lesions, and resolve their symptoms in 1 to 2 weeks.
Recurrences of genital herpes are often heralded by a warning prodrome of
tingling or numbness in the perineal area. Vesicles and their subsequent
ulcers are often solitary. The duration of symptoms is often several days
and usually less than a week.
|
|
|

|
|
Recurrent
Lesions—Female Solitary,
minimally painful lesion of recurrent genital herpes. (Courtesy of H.
Hunter Handsfield: Atlas of Sexually Transmitted Diseases. New
York: McGraw-Hill; 1992.)
|
|
Differential Diagnosis
Pustular psoriasis, chancroid,
erythema multiforme, fixed drug eruption, Behçet's disease,
Stevens-Johnson syndrome, pyoderma gangrenosum, syphilis, and pyodermic
infection may have a similar appearance.
Emergency Department Treatment
and Disposition
Primary genital herpes: Acyclovir,
200 mg PO five times daily for 7 to 10 days or until symptoms resolve;
400 mg PO tid may be substituted for patient convenience.
Recurrent genital herpes: Acyclovir,
200 mg PO five times daily; 400 mg PO tid for 5 to 7 days; or
Famciclovir, 125 mg PO bid for 5 days.
Clinical Pearls
1. Women with genital herpes
must be counseled to inform their obstetrician of this history of herpes
when they become pregnant.
2. Genital herpes is the most
common cause of ulcerating genital lesions.
3. Patients may initially
present with full-blown primary genital herpes symptoms or may have their
first clinical presentation as a recurrence of an asymptomatically
acquired infection (Fig. 9.20).
|
|
|
|
|
Herpes
Simplex Virus—Cervix
Erosive ulcerations of the cervix in a patient with genital herpes
infection. This patient may be completely asymptomatic and may
transmit the disease. (Courtesy of A. Wisdom: Sexually Transmitted
Diseases. London: Mosby-Wolfe; 1992.)
|
|
|
|
Chancroid
Associated Clinical Features
Chancroid is caused by Haemophilus
ducreyi. After an incubation period of 2 to 10 days, this disease
presents with multiple, painful, nonindurated genital ulcerations that
are often deep and undermined and may have a purulent base (Fig. 9.21).
Inguinal adenopathy may develop and becomes fluctuant, large, and painful
(Fig. 9.22). Infected lymph nodes may rupture spontaneously. Systemic
symptoms are uncommon.
|
|
|

|
|
Chancroid
Lesions Multiple painful, deep
ulcerations of chancroid. (Courtesy of H. Hunter Handsfield: Atlas
of Sexually Transmitted Diseases. New York: McGraw-Hill; 1992.)
|
|
|
|
|

|
|
Chancroid
Lesions and Inguinal Nodes
Chancroid lesions with an enlarged lymph node. On examination, this
node is tender and fluctuant. (Courtesy of H. Hunter Handsfield: Atlas
of Sexually Transmitted Diseases. New York: McGraw-Hill; 1992.)
|
|
Differential Diagnosis
Lymphogranuloma venereum,
granuloma inguinale, herpes simplex virus, and syphilis should be
considered.
Emergency Department Treatment
and Disposition
Ceftriaxone, 250 mg IM once, or
azithromycin, 1 g PO once. Alternatives include amoxicillin and
clavulanic acid, 500 mg and 125 mg PO tid for 7 days or ciprofloxacin,
500 mg PO bid for 3 days. Large, fluctuant nodes should be aspirated to
prevent rupture; incision and drainage should be avoided to prevent
development of chronic draining sinus tracts. Partners should be notified
of exposure to the disease.
Clinical Pearls
1. Chancroid is usually found
in high-risk populations: drug-abusing, inner-city.
2. Chancroid is a diagnosis of
exclusion, as culturing H. ducreyi requires a special medium not
readily available. Genital herpes and syphilis must be ruled out.
3. The lymphadenopathy of
chancroid is often very tender and fluctuant.
4. Chancroid lesions are very
tender and usually multiple.
|
|
Pediculosis
Associated Clinical Features
Pediculosis can be caused by
either the body louse or the crab louse. Body lice (Fig. 17.21) are not
sexually transmitted and tend to cluster around the waist, shoulders,
axillae, neck, and head. They are extremely itchy; patients may present
with excoriations and intense pruritus. The lice are very small and may
not be easily seen. The larval form of the louse, the nit, may be
mistaken for dandruff in the hair. Unlike dandruff, however, the nits are
extremely adherent to the hair shaft and cannot be brushed out of the
hair. The adult lice and their eggs are often found in the seams of
clothing.
Pubic infestation is caused by Phthirus
pubis, the crab louse (Figs. 9.23, 21.20). Patients may present with
intense itching in the pubic area; however, as many as half of patients
with this infestation may be asymptomatic. Patients may notice the lice
or may note tiny rust-colored spots on their underwear, which represent
bleeding from the sites of louse bites. Nits may be found at the base of
pubic hairs and hatch in 5 to 10 days.
|
|
|

|
|
Pediculosis
Pubis—on Hairs Phthirus
pubis, or the crab louse, in the pubic hair of a patient
complaining of itching. Note also the nits attached to the hairs.
(Courtesy of Morse, Moreland, Thompson: Atlas of Sexually
Transmitted Diseases. London: Mosby-Wolfe; 1990.)
|
|
Differential Diagnosis
Tinea, contact dermatitis,
scabies, and heat rash may have a similar appearance.
Emergency Department Treatment
and Disposition
Lindane shampoo (Kevell) should
be lathered into the pubic, perineal, and perianal hair, or lindane
lotion applied in the affected areas and left on for 10 min and rinsed
off. Synergized pyrethrins (RID), or synthetic pyrethrins (NIX, Elmite),
may also be used. Since lindane may be toxic, pyrethrins are preferred in
pregnant women and children. Treatment should be repeated in 1 week to
treat any nits that may have hatched. Clothing worn or linen used in the
preceding 24 h should be washed. Mechanical removal of nits attached to
hairs should be attempted. Petroleum jelly or any bland ophthalmic
ointment can be applied to the eyelashes twice daily for a week to treat
infestation of the eyelashes (Fig. 9.24). Sexual contacts should be
examined.
|
|
|

|
|
Pediculosis
Pubis—on Eyelashes Phthirus
pubis lice noted in the eyelashes. (Courtesy of Spalton,
Hitchings, Hunter: Atlas of Clinical Ophthalmology, 2d ed.
London: Mosby–Year Book Europe; 1994.)
|
|
Clinical Pearls
1. Nits are easier to find on
examination than are mature lice; the average number of lice in an
infestation is only 10.
2. Patients with pediculosis
pubis should be considered at risk for other sexually transmitted
diseases and examined.
3. Lindane shampoo or lotion
should not be used in infants under 1 year of age or in pregnant women.
|
|
Condyloma Acuminata (Genital Warts)
Associated Clinical Features
Caused by human papillomavirus
(HPV), these flesh-colored lesions may be flat, sessile, or pedunculated
(Figs. 9.25, 9.26). They often have a cauliflowerlike appearance and are
usually asymptomatic but may be seen or felt by patients or their sexual
partners. They range in size from 1 to 4 mm to masses that may be several
centimeters large (giant warts, Figs. 9.27, 9.28).
|
|
|

|
|
Genital
Warts—Female Verrucous
lesions of the posterior fourchette in a patient with condyloma
acuminata. (Used with permission from H. Hunter Handsfield: Atlas
of Sexually Transmitted Diseases. New York: McGraw-Hill; 1992.)
|
|
|
|
|
|
|
Genital
Warts—Male Typical
appearance of condyloma acuminata of the glans penis. (Courtesy of
Morse, Moreland, Thompson: Atlas of Sexually Transmitted Diseases.
London: Mosby-Wolfe; 1990.)
|
|
|
|
|

|
|
Giant
Warts—Female Giant warts
of a female patient with extensive condyloma acuminata. (Courtesy of
Morse, Moreland, Thompson: Atlas of Sexually Transmitted Diseases.
London: Mosby-Wolfe; 1990.)
|
|
|
|
|

|
|
Giant
Warts—Male Giant warts
in a male patient with extensive condyloma acuminata. (Courtesy of A.
Wisdom: Sexually Transmitted Diseases. London: Mosby-Wolfe;
1992.)
|
|
Differential Diagnosis
Condyloma lata due to secondary
syphilis is the primary alternative diagnosis (Fig. 9.7). Bowen's
disease, molluscum contagiosum, and carcinoma may have a similar
appearance.
Emergency Department Treatment
and Disposition
Local caustic agents (e.g.,
podophyllin) are used to treat the lesions; multiple treatment is often
needed, and recurrence is common. Other therapies include cryotherapy,
electrocautery, and trichloracetic acid. Laser therapy or surgery may be
needed in cases of giant warts.
Clinical Pearls
1. Evidence suggests that HPV
is linked with increased risk of cervical cancer.
2. Women with genital warts
need to have a Pap smear to rule out coexisting carcinoma in situ.
3. Large lesions should be
biopsied to rule out cancer.
4. Patients should be advised
that it may take several to many visits to completely eradicate the
condyloma.
5. In cases where the diagnosis
is not obvious, rule out condyloma lata (secondary syphilis) by sending
serologic studies.
|
|
Anal Fissure
Associated Clinical Features
An anal fissure is a longitudinal
tear in the skin of the anal canal and usually extends from the dentate
line to the anal verge. Fissures are thought to be caused by the passage
of hard or large stools with constipation, but they may also be seen with
diarrhea. The fissures are typically a few millimeters wide and occur in
the posterior midline (Fig. 9.29), but they can occur elsewhere. An anal
fissure that is off the midline may have a secondary cause, such as
inflammatory bowel disease or sexually transmitted infection. Although
often seen in infants, this condition is found mostly in young and
middle-aged adults. Patients present with the complaint of intense sharp,
burning pain during and after bowel movements. They may also note bright
red blood at the time or shortly after the passage of stool. Gentle
examination with separation of the buttocks usually provides good
visualization (Fig. 9.29). Anoscopy should be performed, if possible.
|
|
|

|
|
Anal
Fissure A typical anal fissure
located in the posterior midline. (Courtesy of Paul J. Kovalcik, MD.)
|
|
Differential Diagnosis
The diagnosis of inflammatory
bowel disease, ulcerative colitis, or Crohn's disease should be
considered, particularly if the fissure is atypical. Anal fissures may be
the result of a sexually transmitted disease such as Chlamydia, gonorrhea,
herpes, and syphilis. Tuberculosis, anal neoplasms, and sickle cell
disease can also present as an anal fissure. An anal abscess and
thrombosed hemorrhoids may cause similar symptoms but can usually be
ruled out on physical examination.
Emergency Department Treatment
and Disposition
Acute treatment of anal fissures
consists of anal hygiene, bulk fiber diet supplements to soften stools,
warm sitz baths, and topical anesthetics. Oral pain medication and muscle
relaxants such as diazepam may be required in certain patients.
Clinical Pearls
1. Pain and involuntary
sphincter spasm may preclude a routine digital or anoscopic examination
and require an examination under anesthesia.
2. A proctoscopic examination
should be done at some point to rule out secondary causes.
3. Most anal fissures heal
spontaneously, but refractory cases may require surgical repair.
|
|
Perianal-Perirectal Abscesses
Associated Clinical Features
The perianal abscess is the most
common anorectal abscess. It is associated with pain in the anal area
that is exacerbated by bowel movements, straining, coughing, or
palpation. On examination, a fluctuant and possibly erythematous mass is
found at the perianal region (Fig. 9.30). Perianal abscesses are usually
fairly superficial and easy to drain with local anesthesia. The patient
may notice swelling or a pressure sensation. Perirectal abscesses tend to
be more complex and are named according to the involved space:
ischiorectal, intersphincteric, or supralevator (Fig. 9.31). These are
fluctuant masses that are usually palpable along the rectal wall.
Patients may complain of pain, fever, and mucous or bloody discharge with
bowel movement.
|
|
|

|
|
Perianal
Abscess Swelling and erythema
around the anus consistent with a perianal abscess. (Courtesy of the
American Society of Colon and Rectal Surgeons.)
|
|
|
|
|
|
|
Perianal-Perirectal
Abscesses The anatomy of
perianal and perirectal abscesses is illustrated. Also shown are anal
fissure and internal and external hemorrhoids.
|
|
Differential Diagnosis
Crohn's disease should be
considered, because 36% of Crohn's patients have a perianal abscess at
the presentation of their disease. An underlying process may exist, such
as diabetes mellitus, leukemia, or other malignancy.
Emergency Department Treatment
and Disposition
Incision and drainage of perianal
abscesses should be performed with a small radial or cruciate incision
lateral to the external sphincter. For an uncomplicated abscess, this can
be accomplished under local anesthesia. The cavity should be cleared of
loculations and then loosely packed with iodoform gauze, which should be
removed in 24 to 48 h. All patients require outpatient follow-up.
Antibiotic therapy is not indicated unless there is underlying disease
affecting the patient's immunologic function or the patient appears
septic. Surgical consultation should be obtained for treatment of
perirectal abscesses under anesthesia.
Clinical Pearls
1. Surgical consultation and
treatment may be required in the patient with a large or complicated
perianal abscess or where adequate analgesia cannot be obtained.
2. Consider admission for
debilitated, elderly, febrile, obese, or otherwise ill-appearing
patients.
3. All patients warrant
follow-up referral due to the high incidence of fistulae with anorectal
abscesses.
|
|
Internal-External Hemorrhoids
Associated Clinical Features
External hemorrhoids result from
the dilatation of the venules of the inferior hemorrhoidal plexus below
the dentate line. They have a covering of skin, or anoderm, versus
internal hemorrhoids, which have a mucosal covering. Hemorrhoids commonly
present with an episode of rectal bleeding of bright red blood after
defecation. This results from the passage of the fecal mass over the thin-walled
venules, causing abrasions and bleeding. Symptoms from external
hemorrhoids include complaints of swelling and burning rectal pain.
Numerous associated factors exist, such as constipation, family history,
pregnancy, portal hypertension, or increased intraabdominal pressure.
Hemorrhoids are commonly found at three anatomic locations: right
anterior, right posterior, and left lateral positions (Fig. 9.32). A
thrombosed external hemorrhoid contains intravascular clots and causes
exquisite pain the first 48 h.
|
|
|

|
|
External
Hemorrhoids Multiple engorged
external hemorrhoids are seen in all quadrants. (Courtesy of the
American Society of Colon and Rectal Surgeons.)
|
|
Internal hemorrhoids (Figs. 9.31, 9.33) present with
painless rectal bleeding or possibly the sensation of prolapse. They are
graded according to the degree of prolapse, where the first degree is
identifiable at the dentate line and the fourth degree shows irreducible
prolapse through the anus. Internal hemorrhoids are not typically
painful, whereas external hemorrhoids do cause pain.
|
|
|

|
|
Internal
Hemorrhoids Internal
hemorrhoids are seen in this endoscopic view of the rectum. (Courtesy
of Virender K. Sharman, MD.)
|
|
Differential Diagnosis
Other diagnoses to consider
include infection, perianal or perirectal abscess, inflammatory bowel
disease, malignancy, local trauma, herpes or other sexually transmitted
infection, rectal polyp, or rectal prolapse.
Emergency Department Treatment
and Disposition
In the case of severe bleeding,
fluid resuscitation would need to be instituted and the bleeding vessel
located, clamped, and ligated. The treatment for less severe cases
warrants more conservative therapy, including increased dietary fiber,
increased fluid intake, hot sitz baths, bed rest, and nonnarcotic pain
medication. Advanced cases may require surgical consultation and
treatment. ED treatment of thrombosed external hemorrhoids includes an
elliptical excision and extrusion of the clot under local anesthesia.
Clinical Pearls
1. Many patients with any
anorectal problem complain of hemorrhoids. Therefore, careful examination
and consideration of the differential diagnosis should be undertaken with
each patient.
2. Having the patient strain
during the examination may reveal bleeding or prolapse that might
otherwise go unnoticed.
3. Hemorrhoids are a rare cause
of anorectal pruritus.
|
|
Prolapsed Rectum
Associated Clinical Features
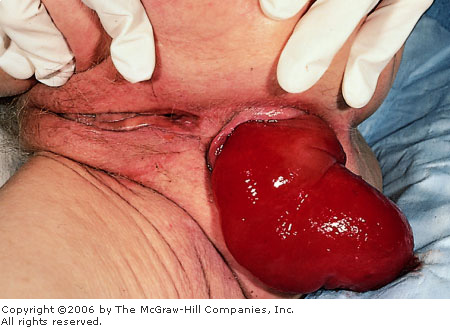
Rectal prolapse occurs when
anorectal tissue slides through the anal orifice; it can include mucosa
or a full-thickness layer. This is due to several anatomic features,
including laxity of the pelvic floor, weak anal sphincters, and lack of
mesorectal fixation. Patients complain of bleeding, mucous discharge,
rectal pressure, or a mass (Fig. 9.34). Problems with fecal incontinence,
constipation, and rectal ulceration are common as well. Prolapse may be
associated with an increased familial incidence, chronic cough,
dysentery, or parasitic infection.
|
|
|
|
|
Prolapsed
Rectum The rectum is
completely prolapsed in this elderly patient. (Courtesy of Alan B.
Storrow, MD.)
|
|
Differential Diagnosis
Other diagnoses to consider
include foreign body, tumor, perianal or perirectal abscess, rectal
polyp, or engorged external hemorrhoids.
Emergency Department Treatment
and Disposition
Usually reduction is possible
with gentle manual pressure. However, if this cannot be accomplished,
surgical consultation and admission are needed. Surgical treatment is
also indicated with a complete prolapse. All patients should undergo an
anoscopic and sigmoidoscopic examination at some point; if rectal
bleeding is a problem, full colonic evaluation should be completed.
Clinical Pearls
1. This is commonly seen in
children with cystic fibrosis (22%); therefore, all children with rectal
prolapse should have a sweat chloride test.
2. Examination of rectal
prolapse reveals concentric mucosal rings and a sulcus between the anal
canal and the rectum, whereas prolapsed hemorrhoids are separated by
radial grooves and the sulcus is absent.
3. To confirm the diagnosis,
prolapse may be reproduced by having the patient bear down.
|
|
Pilonidal Abscess
Associated Clinical Features
Pilonidal abscesses are typically
seen at or just superior to the gluteal fold (Fig. 9.35) and are more
common in teenage and young adult males. Patients complain of localized
pain, swelling, and drainage but usually do not have systemic symptoms.
The abscess begins with the formation of a small opening in the skin that
develops into a cystic structure involving surrounding hairs. This
opening is occluded by hair or keratin, creating a closed space that does
not allow drainage. The acute abscess contains mixed organisms including Staphylococcus
aureus and Streptococcus, but anaerobes and gram-negative
organisms may also be present.
|
|
|

|
|
Pilonidal
Abscess Redness, fluctuance,
and tenderness in the gluteal cleft seen with a pilonidal abscess.
(Courtesy of Louis La Vopa, MD.)
|
|
Differential Diagnosis
Evidence of cellulitis in the
sacrococcygeal area may result from a simple abscess or furuncle.
However, other causes should be considered, such as anal fistulae,
hidradenitis, inflammatory bowel disease, or tuberculosis.
Emergency Department Treatment
and Disposition
An acutely fluctuant abscess
requires incision and drainage under local anesthesia with removal of pus
and debris. The patient should be instructed on meticulous wound care and
sitz baths. Antibiotic therapy is not indicated unless the patient is
immunocompromised. Surgical referral is given, particularly with a
chronic or recurrent cyst, which may require surgical excision and
closure.
Clinical Pearls
1. Pilonidal abscesses almost
always occur in the midline but can have sinus tracts extending off the
midline.
2. Pilonidal disease is three
times more common in men than in women.
|
|
Rectal Foreign Body
Associated Clinical Features
The diagnosis of rectal foreign
body is usually made by history and confirmed by digital examination.
Most often the foreign body is inserted (Fig. 9.36), but it is possible
to have an ingested foreign body trapped in the rectum. The most serious
complication of a rectal foreign body is perforation of the rectum or
distal colon. The patient must be carefully evaluated for evidence of
perforation with x-rays demonstrating free air and clinically for the
presentation of an acute abdomen. Perforation above the peritoneal
reflection is associated with free air in the abdominal cavity and
peritoneal signs. Perforation below the peritoneal reflection presents
with more insidious signs of pain and infection in the perianal or
perineal region. It is important to determine the size, shape, and number
of objects to assess the risk of perforation. In children, rectal foreign
bodies usually present as rectal bleeding.
|
|
|

|
|

|
|
Rectal
Foreign Body Top:
The metallic outline of two batteries is seen in this x-ray. Bottom:
This foreign body (a 7-oz beer bottle) required removal in the
operating room. [Courtesy of David W. Munter, MD (top), and
Kevin J. Knoop, MD, MS (bottom).]
|
|
Differential Diagnosis
Depending on the clinical
scenario, the diagnoses of sexual assault or child abuse should be
considered.
Emergency Department Treatment
and Disposition
Removal can often take place in
the ED with sedation of the patient and local anesthesia of the anal
sphincter. If the risk of perforation appears high or adequate relaxation
and anesthesia cannot be obtained, then the patient is prepared for
emergency surgery. After removal, proctoscopic or sigmoidoscopic
examination is recommended to rule out perforation or laceration.
Clinical Pearls
1. A Foley catheter or an
endotracheal tube may be used to release the vacuum effect of some
foreign bodies, and the balloon can be inflated and aid in the removal.
2. A rectal foreign body in a
child should raise the suspicion of abuse.
|
|
Melena
Associated Clinical Features
Gastrointestinal bleeding
commonly presents with the alteration of stool color. By definition,
melena is the passage of dark, pitchlike stools stained with blood
pigments (Fig. 9.37). Generally, but not always, melena results from
bleeding into the upper gastrointestinal tract proximal to the ligament
of Treitz. Black stools have been seen with as little as 60 mL of blood
in the upper gastrointestinal tract, but melena typically does not
develop until 100 to 200 mL is present. Melena can be found in lower
bleeds with decreased transit time, as with an obstruction distal to the
site of bleeding.
|
|
|

|
|
Melena The black, tarry appearance of melena in a
patient with a duodenal ulcer. (Courtesy of Alan B. Storrow, MD.)
|
|
Differential Diagnosis
Melenic stools may occur from
swallowed blood, as from epistaxis or other oropharyngeal bleeding. Dark
or black stools can also be seen with the ingestion of bismuth
salicylate, food coloring, and iron supplements.
Emergency Department Treatment
and Disposition
Patients with melenic stools
should be evaluated in a monitored setting and undergo assessment for
signs and symptoms of hypovolemia and treated accordingly. At least one
large-bore intravenous line should be placed and saline infused.
Depending on the patient's stability, type-specific packed red blood cells
or other blood products may be required. Abdominal radiographs are done
to look for free air in the peritoneum, and gastric aspiration should be
done to assess for active gastric bleeding. Stable patients who present
with melena may be admitted to the ward. Evidence of unstable vital
signs, continued bleeding, severe anemia, or comorbid disease warrants
admission to the intensive care unit. Consultation with a
gastroenterologist should be sought unless patients require more than two
units of blood for resuscitation, which would call for surgical
intervention.
Clinical Pearls
1. Melena is the most common
presenting symptom of bleeding from peptic ulcer disease.
2. Melena represents
approximately 200 mL of blood loss in the gastrointestinal tract.
|
|